Translate this page into:
Blue vitiligo: A dermoscopic perspective
2 Department of Dermatology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India
Correspondence Address:
Balachandra S Ankad
Department of Dermatology, S. Nijalingappa Medical College, Navanagar, Bagalkot - 587 102, Karnataka
India
| How to cite this article: Ankad BS, Nikam BP, Jaju PS. Blue vitiligo: A dermoscopic perspective. Indian J Dermatol Venereol Leprol 2019;85:634-637 |
Sir,
Dermoscopy is a rapidly progressive diagnostic technique which is expanding its utility, well beyond pigmented lesions including inflammatory conditions. Although the diagnosis of vitiligo is easy, the rarer variants constitute diagnostic challenges. Blue vitiligo is a unique variant of vitiligo that presents as asymptomatic bluish macules.[1],[2] Dermoscopy of vitiligo, per se, is well-documented.[3] Although dermoscopy of blue vitiligo is reported in literature, the basis of the visualized patterns is not explained.[1],[4] Herein, the authors evaluated the reported dermoscopic patterns and analyzed the rationale behind the bluish color in blue vitiligo.
Case Report
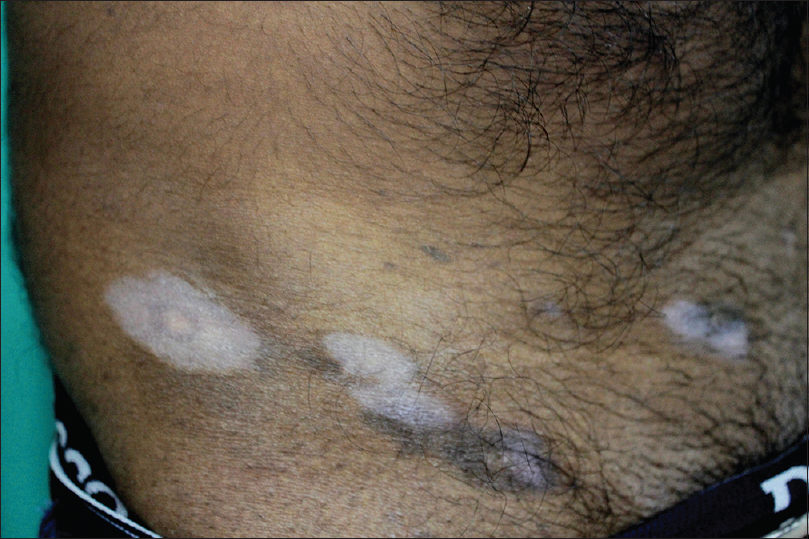
Two male patients aged 48 and 36 years, respectively, had progressive, white-colored lesions over the neck, chest, waist, and extremities. There was no history of drug intake, intralesional injection, or topical application. Cutaneous examination revealed milky-white depigmented patches over the neck, arm, and waist areas which had a bluish tinge [Figure - 1]. The second patient showed bluish-grey patches extending beyond the white patches over the abdomen. Interestingly, the bluish discoloration was observed only in a few patches [Figure - 2]. Wood's lamp examination revealed whitish fluorescence. Dermoscopy demonstrated white structureless areas studded with numerous bluish-black and bluish-gray dots. Dots were arranged in various patterns - linear, arcuate and semicircular. [Figure - 3] and [Figure - 4]. Biopsy showed unremarkable epidermis and moderate infiltrate, melanin incontinence, and numerous melanophages in the papillary dermis [Figure - 5] and [Figure - 6]. Immunohistochemistry (IHC) using HMB 45 and S100 revealed negativity suggesting absence of melanocytes in the epidermis [Figure - 7] and [Figure - 8]. Based on the dermoscopy, Wood's lamp examination, histopathology, and IHC studies, the diagnosis of blue vitiligo was confirmed.
 |
| Figure 1: Clinical image of blue vitiligo showing depigmented patches with bluish hue on some of the patches over the neck area |
 |
| Figure 2: Clinical image of blue vitiligo with bluish-white patches on the waist area |
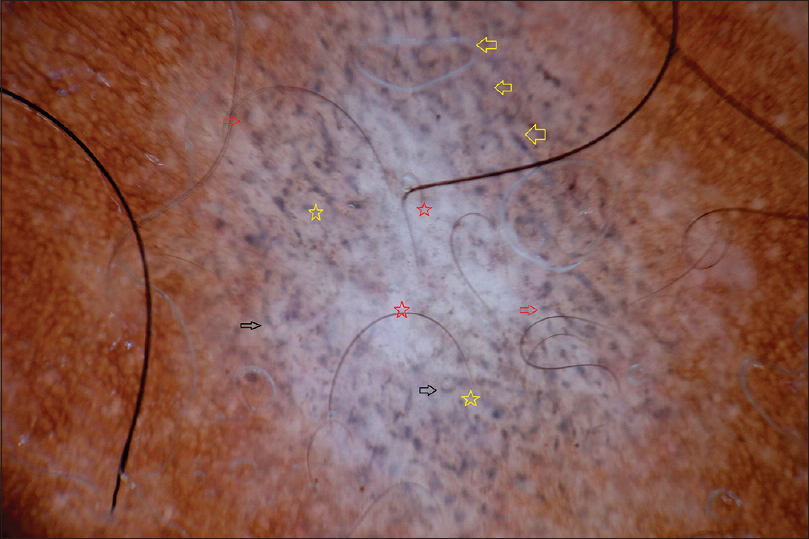 |
| Figure 3: Dermoscopy shows white structureless areas (red stars). Arrangement of bluish-black and bluish-gray dots in linear (yellow arrows), arcuate (red arrows), semicircular (black arrows), and speckled (yellow stars) patterns is very well appreciated (DermLite 3, non-contact polarized, ×10) |
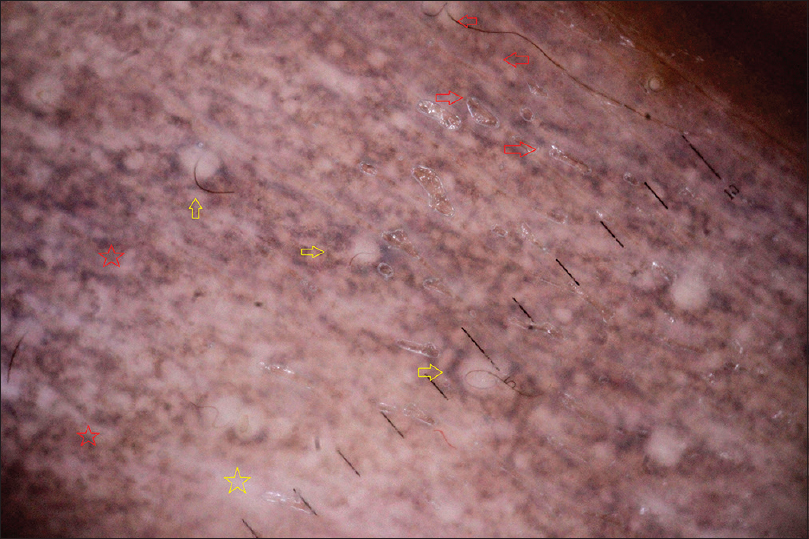 |
| Figure 4: Dermoscopy shows white structureless areas (yellow star) and arrangement of bluish-black and bluish-gray dots in linear (red arrows), semicircular (yellow arrows), and speckled (red stars) pattern is very well noted (DermLite 3, non-contact polarized, ×10) |
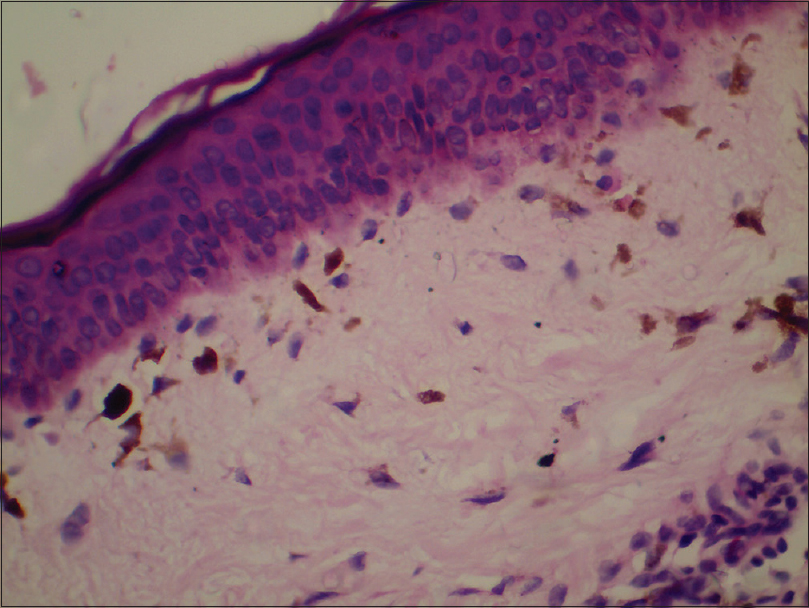 |
| Figure 5: Histopathology of case 1 shows absence of melanin in epidermis and presence of melanophages and heavy inflammatory infiltrate (H and E, ×400) |
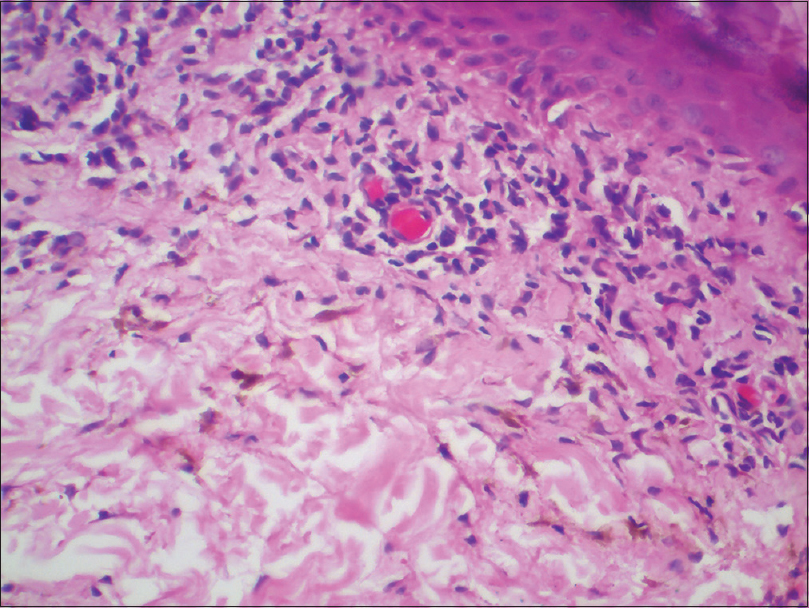 |
| Figure 6: Histopathology case 2 shows absence of melanin in epidermis and presence of heavy and intense inflammatory infiltrate and melanophages in the dermis (H and E, ×400) |
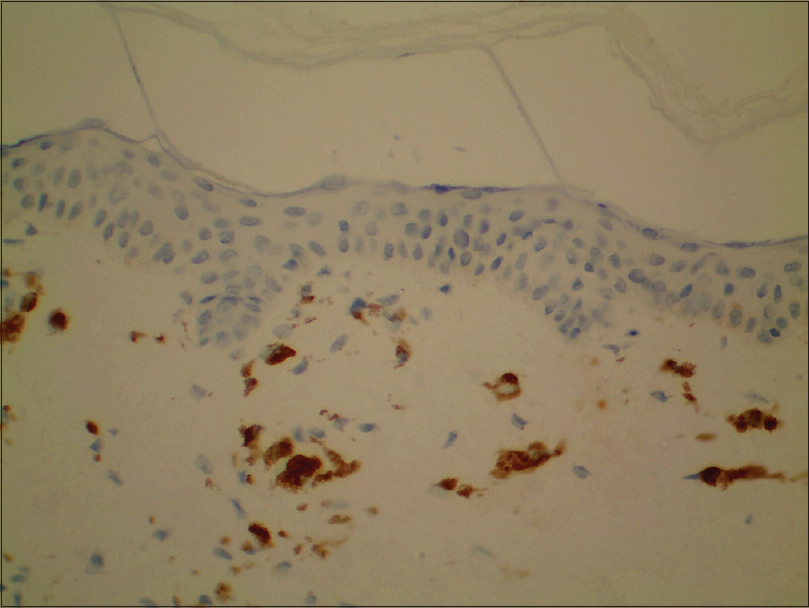 |
| Figure 7: Immunohistochemistry study in case 1 shows melanocyte was negative for HMB 45. Melanophages were well appreciated and delineated in dermis |
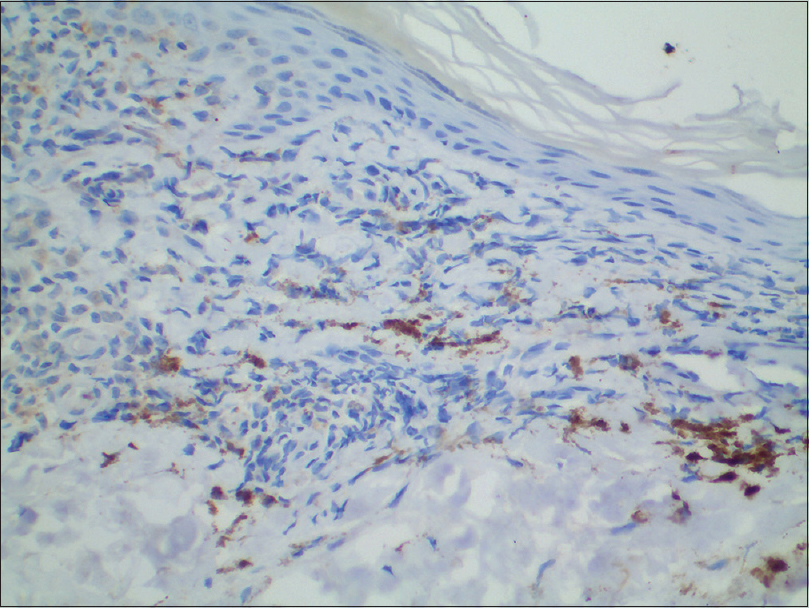 |
| Figure 8: Immunohistochemistry study in case 2 shows melanocytes were negative for HMB 45 which has stained the melanophages in the dermis |
Dermoscopy of blue vitiligo demonstrates white patches and linear areas with multiple blue dots.[1] Reticular telangiectasias were noted in one case in literature.[1],[4] In this series, case 1 revealed a homogenous white, structureless area with multiple bluish-black and bluish-gray dots in arcuate, linear, semi-circular and speckled patterns explaining the arrangement of melanophages in the dermis. Case 2 showed similar patterns, but the perifollicular arrangement of dots was more pronounced. Nevertheless, telengiectasia were not observed in our cases. Hence, this study differs from previous studies with respect to color, arrangement of dots, and vascular structures.
Dermoscopically, speckled blue-black dots are seen in lichen sclerosus and discoid lupus erythematosus (DLE) similar to blue vitiligo.[5],[6] Nevertheless, comedo-like openings, linear vessels, and chrysalis strands; and white areas, red dots, telangiectasia, and follicular plugs characterize lichen sclerosus and DLE, respectively. Thus, dermoscopy benefits in distinction of inflammatory conditions. Dermoscopy of lichen planus pigmentosus (LPP) in skin type 4 and 5 shows dense, irregular bluish-gray dots in perieccrine and perifollicular distribution, and the characteristic hem-like pattern, whereas in type 1 and 2, large brownish globules are noted.[7],[8] This disparity is due to color in different skin types. Although possibility of LPP on vitiligo patch was considered, it is precluded by the absence of clinical patches of LPP, epidermal melanin, and colloid bodies in IHC studies as well.
Depigmentation in vitiligo is due to absence of melanocytes in the epidermis. Many theories explain the destruction of melanocytes in vitiligo. Theory of melanocytorrhagy proposes that altered melanocyte responses to friction and stress, induce their detachment and transepidermal loss. This results in depigmentation in the vitiligo patch.[9] The exact pathogenesis for deposition of melanophages in the dermis in blue vitiligo is not known. Previous publications mention that bluish tinge is due to deposition of drugs like psoralens and ziduvudine or as post-inflammatory process.[1],[2] In this study, the bluish tinge appeared without any triggering factors. Hence, the authors believe that acutely heavy, intense inflammatory infiltrate in dermo-epidermal junction leading to basal cell degeneration and dropping off of melanocytes into dermis gives a bluish hue to the patches due to Tyndall effect. When viewed by dermoscopy, melanophages are seen directly without a bed or a layer of melanocytes in the epidermis making dots to appear as bluish-black to bluish-gray in color. Hence, the authors propose that these are de novo blue vitiligo cases, which demonstrate a bluish hue clinically, and bluish-black to bluish-gray tinge under dermoscopy.
To conclude, destruction of dermo-epidermal junction by heavy infiltrate due to intense autoimmune burden of the disease process results in melanophages in dermis, which appear as bluish-black to bluish-gray dots under dermoscopy. Furthermore, dermoscopy differentiates blue vitiligo from similar clinical conditions and aids in accurate diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Zhang JA, Yu JB, Lv Y, Thapa P. Blue vitiligo following intralesional injection of psoralen combined with ultraviolet B radiation therapy. Clin Exp Dermatol 2015;40:301-4.
[Google Scholar]
|
| 2. |
Ivker R, Goldaber M, Buchness MR. Blue vitiligo. J Am Acad Dermatol 1994;30:829-31.
[Google Scholar]
|
| 3. |
Kumar Jha A, Sonthalia S, Lallas A, Chaudhary RK. Dermoscopy in vitiligo: Diagnosis and beyond. Int J Dermatol 2018;57:50-4.
[Google Scholar]
|
| 4. |
Chandrashekar L. Dermatoscopy of blue vitiligo. Clin Exp Dermatol 2009;34:e125-6.
[Google Scholar]
|
| 5. |
Ankad BS, Beergouder SL. Dermoscopic patterns in lichen sclerosus: A report of three cases. Indian Dermatol Online J 2015;6:237-40.
[Google Scholar]
|
| 6. |
Lopez-Tintos BO, Garcia-Hidalgo L, Orozco-Topete R. Dermoscopy in active discoid lupus. Arch Dermatol 2009;145:358.
[Google Scholar]
|
| 7. |
Neema S, Jha A. Lichen planus pigmentosus. Pigment Int 2017;4:48-9.
[Google Scholar]
|
| 8. |
Errichetti E, Angione V, Stinco G. Dermoscopy in assisting the recognition of ashy dermatosis. JAAD Case Rep 2017;3:482-4.
[Google Scholar]
|
| 9. |
Kumar R, Parsad D. Melanocytorrhagy and apoptosis in vitiligo: Connecting jigsaw pieces. Indian J Dermatol Venereol Leprol 2012;78:19-23.
[Google Scholar]
|
Fulltext Views
7,094
PDF downloads
2,044





