Translate this page into:
Bullous lichen planus
2 Department of Pathology, Command Hospital and AFMC, Pune, Maharashtra, India
Correspondence Address:
Biju Vasudevan
Department of Dermatology, Command Hospital (Southern Command), Wanowrie, Pune - 411 040, Maharashtra
India
| How to cite this article: Verma R, Vasudevan B, Kinra P, Vijendran P, Badad A, Singh V. Bullous lichen planus. Indian J Dermatol Venereol Leprol 2014;80:279 |
Sir,
Lichen planus (LP) is a chronic inflammatory dermatosis involving mucocutaneous surfaces and nails. The world-wide prevalence of the disease is estimated to be 1%. [1] Bullous lichen planus is a rare variant which usually presents with blisters occurring over typical lesions of lichen planus. Raely, a few lesions occur in the adjoining skin. It is to be differentiated from lichen planus pemphigoides in which the blisters are more generalized and extensive and the course is prolonged.
A 45-year-old male patient presented with a 3-months history of insidiously developing multiple, itchy, red raised papules over both forearms that gradually spread to the trunk and all extremities over a few weeks. Two months later, a few vesicles developed over the pre-existing papules as well as on normal skin. The vesicles did not rupture spontaneously but on squeezing would release clear fluid and leave behind raw areas. There were no oral lesions. No drugs were taken prior to development of the eruption. There was no history of weight loss, fever or exacerbation of the eruption with sun exposure.
There were multiple, discrete to confluent, erythematous to violaceous papules coalescing to form plaques on the extremities, trunk and buttocks [Figure - 1]. Koebnerization was seen. There were multiple tense bullae over extremities including palms and soles. These bullae were present on the violaceous lesions as well as on normal skin [Figure - 2]. Bulla spread sign and Nikolsky′s sign were both negative. Mucosae, nails and hair were normal. General and systemic examination did not reveal any abnormality.
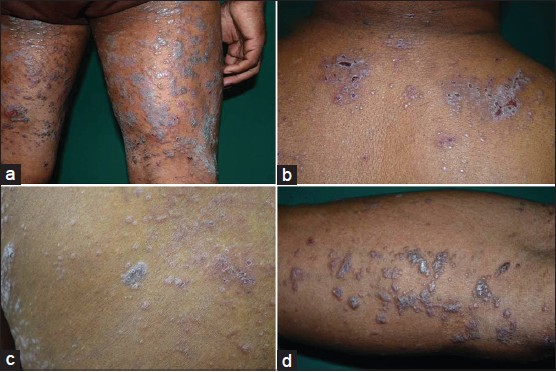 |
| Figure 1: Close up of lichen planus lesions - (a) Left leg showing coalescing lesions (b) upper back (c) well-defi ned scaly plaques on back (d) Koebnerization of lesions on forearm |
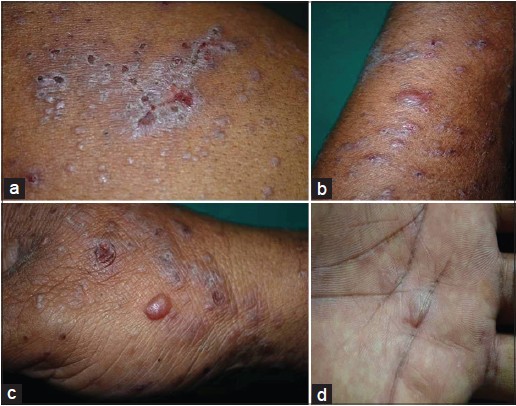 |
| Figure 2: Bullous lesions - (a) Ruptured bullae forming crusted erosions on lichen planus (LP) lesions (b) large bulla over LP lesion on forearm (c) bullae on lesional and non-lesional skin on hand (d) bullae on palm |
Routine blood tests and urinalysis were normal. Skin biopsy from a papule showed features of lichen planus. Biopsy of a tense blister overlying a violaceous papule revealed a spongiotic epidermis with marked basal vacuolar cell degeneration and foci of colloid bodies. The extensive vacuolation of basal cells led to the appearance of a dermo-epidermal cleft [Figure - 3]. There was a dense inflammatory infiltrate hugging the epidermis along with a moderate perivascular lympho-plasmacytic infiltrate. Direct immunofluorescence study showed no immunoreactants along the basement membrane zone. A final diagnosis of bullous lichen planus was made and the patient was treated with oral prednisolone 40 mg/day, which was tapered off in 6 weeks. He responded well to therapy with all lesions regressing in 6 weeks and no relapses until 6 months after follow-up.
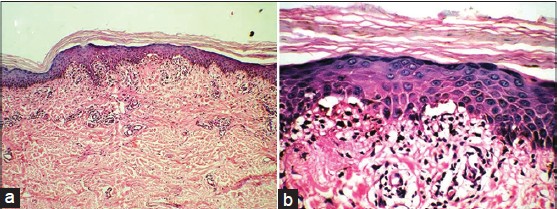 |
| Figure 3: Histopathology from bulla overlying lichen planus lesions revealing. (a) Appearance of subepidermal clefting due to extensive basal cell vacuolation and lymphocytic infi ltrate hugging the epidermis (H and E, ×10) (b) High power view revealing clefting, pigment incontinence and dermal melanophages (H and E, ×40) |
Bullous lichen planus is commonly seen on the legs. Blisters are tense and may be multilocular. Bulla formation may be due to the extensive liquefaction and vacuolation of the basal layer. Histopathologically, biopsy from the bullous lesion is characterized by a subepidermal bulla accompanied by classical changes of lichen planus. Direct and indirect immunofluorescence testing is negative.
Lichen planus pemphigoides is characterized by bullae developing over lesions of lichen planus and also on normal appearing and erythematous skin, especially during an acute episode of lichen planus. The condition occurs in a much younger age group than bullous pemphigoid which is a disease mainly seen in the elderly population. It is commoner in men and usually occurs on the extremities, though dissemination can occur. [2] As in bullous lichen planus, the bulla is subepidermal but features of lichen planus are not evident and inflammatory cells are mainly neutrophils and lymphocytes with a few eosinophils. [3] Direct immunofluorescence testing of perilesional skin shows linear deposits of C3 and IgG along the basement membrane zone. Circulating antibodies have been demonstrated against 130, 200 and 180 kda antigens. [4] Damage to the basal cells could unmask hidden antigenic determinants or create new antigens thus leading to autoantibody formation. Disturbances in local control of immune regulation may also be responsible. Healing may leave behind post-inflammatory hyperpigmentation. Lichen planus pemphigoides can also be associated with various drugs such as angiotensin-converting enzyme inhibitors, cinnarizine, simvastatin, or following psoralen combined with ultraviolet A therapy. [5]
In our patient, the appearance of bullous lesions on normal appearing skin away from the papules of lichen planus created a clinical impression of lichen planus pemphigoides. However, histopathology and immunofluorescence confirmed the diagnosis of bullous lichen planus. Another interesting aspect of our case was the development of bullae on the palms and soles, rarely reported previously.
| 1. |
Bhattacharya M, Kaur I, Kumar B. Lichen planus: A clinical and epidemiological study. J Dermatol 2000;27:576-82.
[Google Scholar]
|
| 2. |
Harjai B, Mendiratta V, Kakkar S, Koranne RV. Childhood lichen planus pemphigoides-A rare entity. J Eur Acad Dermatol Venereol 2006;20:117-8.
[Google Scholar]
|
| 3. |
Gawkrodger DJ, Stavropoulos PG, McLaren KM, Buxton PK. Bullous lichen planus and lichen planus pemphigoides - Clinico-pathological comparisons. Clin Exp Dermatol 1989;14:150-3.
[Google Scholar]
|
| 4. |
Yoon KH, Kim SC, Kang DS, Lee IJ. Lichen planus pemphigoides with circulating autoantibodies against 200 and 180 kDa epidermal antigens. Eur J Dermatol 2000;10:212-4.
[Google Scholar]
|
| 5. |
Zhu YI, Fitzpatrick JE, Kornfeld BW. Lichen planus pemphigoides associated with ramipril. Int J Dermatol 2006;45:1453-5.
[Google Scholar]
|
Fulltext Views
13,526
PDF downloads
3,523





