Translate this page into:
Bullous pemphigoid after femur fracture surgery: A mere coincidence?
Correspondence Address:
Hao Chen
12, Jiangwangmiao St., Nanjing - 210 042
China
| How to cite this article: Zeng R, Chen H, Jiang Y, Li M. Bullous pemphigoid after femur fracture surgery: A mere coincidence?. Indian J Dermatol Venereol Leprol 2014;80:195 |
Sir,
Bullous pemphigoid (BP) is an autoimmune blistering skin disease that occurs predominantly among elderly persons. It occurs in four to six cases per million people per year, of which only a few involving localized BP have been reported to occur after surgery [1],[2],[3],[4] and only one case of generalized BP devoloped after abdominal hernia surgery. [1] Herein, we report a case of generalized BP developing after femur fracture surgery.
In December 2010, an otherwise healthy 61-year-old woman had a traffic accident that caused a closed fracture of her right femur. An implantation with a titanium alloy plate was carried out immediately. The incision healed and scarred after 2 weeks. One month later, erythema and blistering accompanied by itching developed at the site of the post-surgical scar [Figure - 1], and gradually expanded to the lower limbs, upper limbs, trunk and face in the next 1 month. The patient had no history of bullous skin lesions, surgery or metal allergy.
 |
| Figure 1: A large crusted pink plaque and many tense hemorrhagic bullae developing along the postsurgical scar |
Results of routine blood cell count, serum creatinine and hepatic tests were normal. Biopsy showed a sub-epidermal vesicle with abundant eosinophil infiltrates in the papillary dermis [Figure - 2]. DIF of perilesional skin revealed a clear band of IgG-deposition at the dermo-epidermal junction [Figure - 3], and IIF of the circulating IgG antibodies to BMZ was 1:20. Salt-split IIF found the linear deposition of IgG localized on the epidermal side of the split. ELISA detected antibodies to BP180 in the serum of the patient, and the diagnosis of BP was accordingly confirmed.
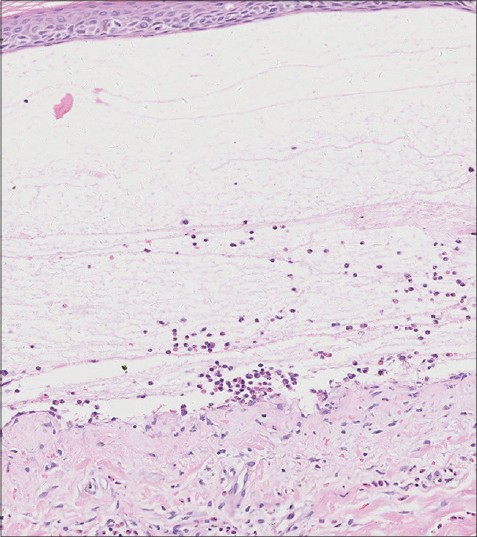 |
| Figure 2: Subepidermal bulla with upper dermal inflammatory infiltrate (H and E, ×200) |
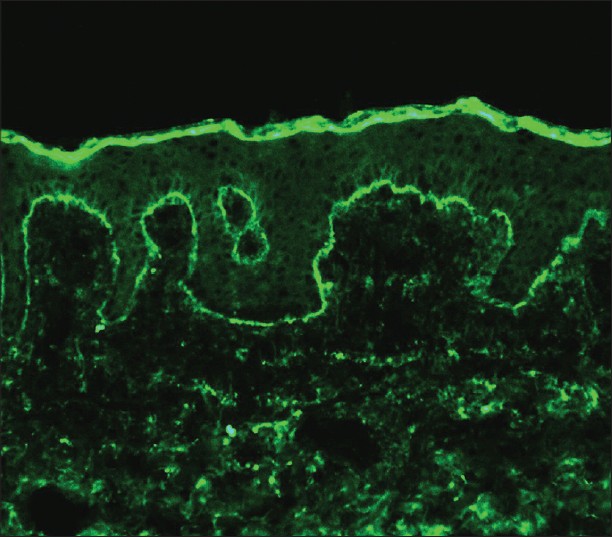 |
| Figure 3: Direct immunofluorescence showing linear deposits of IgG along the basement membrane zone (×200) |
Methyl-prednisolone (1 mg/kg daily) was administered initially to control the bullae for 2 weeks and gradually tapered over 1 year. Six months after surgery, the plate was removed and a patch test revealed no allergic reactions to metals such as titanium, nickel, and iron. Methyl prednisolone was stopped completely after 15 months, without signs of relapse after 3 years.
The onset and course of BP depend on various promoting and predisposing factors such as genetic susceptibility, infection and drugs. The pathogenesis of BP has been ascribed [5] to an autoantibody response to hemidemosome (BP180), which we have seen in this case as well. However, the identification of triggers for BP development is still difficult and often unsatisfactory. In the case we report here, generalized BP developed 1 month after femur injury and metal implantation in the right thigh. Since the femur injury was a closed fracture, we could argue that no skin elements were involved that could trigger BP. Also, the possibility that BP was caused by allergic reactions to the implants was excluded by the negative patch test. The fact that erythema and blistering lesions initially developed at the postsurgical scar in this case suggests that femur surgery may be one of the reasons for BP onset. However, the pathogenesis is still unclear and the occurrence of the BP after surgery may be a merely coincident event, especially when one considers other possible triggers such as drug administration during the surgery and even the trauma itself. Obviously, the contribution of surgery or trauma still needs to be verified since no BP episode occurred in this patient after the procedure to remove the alloy plate. Some skin diseases can develop isomorphic lesions along lines of trauma, for example, psoriasis and vitiligo. This phenomenon is the so-called Koebner phenomenon which mainly appears on pre-existing cutaneous disease. Clearly, our case does not comply with this situation.
BP after surgery usually presents with only localized eruptions. But it may precede generalization by weeks in the absence of intense effective medications. In our case, BP occurred at the incision site after 1 month of surgery and no treatment had been started for a month before the lesions spread to other parts of the body. Therefore, the early recognition of blistering at the surgery site should be recommended for a histopathological assessment. Moreover, although the patient has no history of surgeries or major skin lesions, a further follow-up of BP in this patient is necessary and even a genetic background study should be carried out when the opportunity arises.
| 1. |
Korfitis C, Gregoriou S, Georgala S, Christofidou E, Danopoulou I. Trauma-induced bullous pemphigoid. Indian J Dermatol Venereol Leprol 2009;75:617-9.
[Google Scholar]
|
| 2. |
Torchia D, Caproni M, Ketabchi S, Antiga E, Fabbri P. Bullous pemphigoid initially localized around a urostomy. Int J Dermatol 2006;45:1387-9.
[Google Scholar]
|
| 3. |
Batalla A, Peón G, De la Torre C. Localized bullous pemphigoid at urostomy site. Indian J Dermatol Venereol Leprol 2011;77:625.
[Google Scholar]
|
| 4. |
Pardo J, Rodrguez-Serna M, Mercader P, Fortea JM. Localized bullous pemphigoid overlying a fistula for hemodialysis. J Am Acad Dermatol 2004;51(Suppl 2):S131-2.
[Google Scholar]
|
| 5. |
Giudice GJ, Squiquera HL, Elias PM, Diaz LA. Identification of two collagen domains within the bullous pemphigoid autoantigen, BP180. J Clin Invest 1991;87:734-8.
[Google Scholar]
|
Fulltext Views
2,765
PDF downloads
2,411





