Translate this page into:
Bullous systemic lupus erythematosus in a pregnant woman with anaemia coexisting with asymptomatic hepatic haemangioma
Corresponding author: Prof. Angoori Gnaneshwar Rao, F12 B8 HIG II APHB Baghlingampally, Hyderabad 500044, Telangana, India. dr_a_g_rao@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Rao AG, Naresh M, Sruthi Ch, Jhawar J. Bullous systemic lupus erythematosus in a pregnant woman with anaemia coexisting with asymptomatic hepatic haemangioma. Indian J Dermatol Venereol Leprol 2023;89:585–8.
Dear Editor,
Cutaneous manifestations have been reported in approximately 76% patients with systemic lupus erythematosus during the disease course and vesiculobullous lesions are encountered in less than 1% patients.1 Bullous systemic lupus erythematosus was first described by Pedro and Dahl in 1973. It is a distinctive clinical presentation of systemic lupus erythematosus; usually affecting young adult females and presenting with blisters on an erythematous base involving the face, trunk and extremities.
A 24-year-old female, in the second trimester of third pregnancy, presented to the department of dermatology of SVS Medical College with recurrent blisters and crusted erosions all over her body for last 5 months, associated with severe itching. Initially, she noticed blisters on her trunk which subsequently involved her face, upper and lower limbs and oral mucosa. The blisters ruptured with minimal trauma resulting in crusted erosions. She reported a history of concomitant low-grade fever and denied any history of similar skin rash in her previous two pregnancies or any history of photosensitivity, alopecia, and malar rash. Examination revealed multiple crusted plaques and erosions distributed bilaterally on the face [Figure 1], chest and upper back [Figure 2], both legs, lower abdomen and both buttocks. A single bulla was noted on the left upper chest [Figure 3]. We also noticed a single ulcer on her buccal mucosa extending over to the left angle of mouth. Nikolsky’s sign and Asboe Hansen’s sign were negative. The lesions appeared to heal with irregular hypopigmentation to depigmentation without atrophy, scar or milia. A provisional diagnosis of pemphigoid gestationis was made. Bullous systemic lupus erythematosus, linear immunoglobulin A (IgA) bullous dermatosis, and epidermolysis bullosa acquisita were considered as differentials. Investigations revealed anaemia (haemoglobin 9 gms/dL) normal reticulocyte count 1.8%, normal WBC count: 4700 cells/cubic millimeter and differential count: neutrophils: 65%, lymphocytes: 27%, eosinophils: 05%, monocytes: 03%, basophils: 0.0%. Peripheral blood smear demonstrared mildly microcytic, hypochromic, and anisocytic RBCs, and adequate platelets.

- Crust at left angle of mouth, both supra clavicular region and irregularly linear hypopigmented patches and macules on face and neck
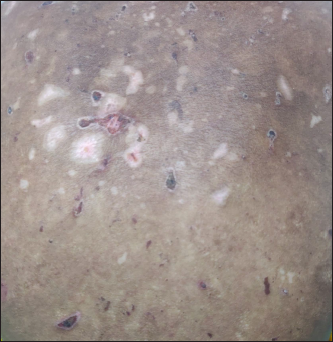
- Multiple irregular depigmented patches and crusts on the back of the trunk

- Large bulla with pus on left clavicular region and crusted plaque on the left shoulder
Urine analysis revealed no abnormality and 24-hour urinary protein was 50 mg (normal < 150 mg). Liver function tests and renal function tests were unremarkable. The Coombs test was negative. Glucose–6–phosphate dehydrogenase was 10 U/g haemoglobin (normal range: 8.8–13.4U/g haemoglobin), venereal disease research laboratory test and human immunodeficiency virus 1 and 2 were unremarkable, and enzyme-linked immunosorbent assay test was done for pemphigoid gestationis antibody (BP180) and BP230 was negative. The antinuclear antibody test was positive with a speckled nuclear pattern. Anti-ds DNA (252 IU/mL) and anti-Sm antibodies were positive, while anti-Ro, anti-La, anti-U1RNP antibodies and anti-phospholipid antibodies were negative. Compliments 3 and 4 were normal. Antibodies to type VII collagen could not be assessed due to non-availability. Chest skiagram and 2-dimensional echocardiogram was unremarkable. Abdominal ultrasonography revealed a gravid uterus corresponding to 24 weeks of gestation and a single small haemangioma measuring 10 × 9 mm in the right lobe of liver. Tzanck smear showed neutrophils and was negative for acantholytic cells and multinucleated giant cells. Perilesional skin biopsy from the back demonstrated a subepidermal cleft with proteinaceous fluid, surrounded by neutrophils, few eosinophils and moderate lymphocytic infiltrate [Figure 4]. A direct immunofluorescence study showed dense immunoglobulin G (IgG) and sparse C3c and IgA deposits along the basement membrane [Figure 5]. To further characterize these immune deposits, an indirect immunofluorescence study was done on salt-split skin, which revealed dense IgG and sparse IgA deposits on the blister floor. [Figure 6]. She attained a score of 10 in the 2019 European League Against Rheumatism/(EULAR)classification criteria for diagnosis of systemic lupus erythematosus (fever-2, oral ulcers-2, anti-ds DNA antibodies and anti-Smith antibodies-6). Finally, she was diagnosed with bullous systemic lupus erythematosus type II (Camisa and Sharma criteria 1983) during pregnancy and we initiated dapsone 50 mg daily along with iron supplementation. Within a week, all lesions healed and we continued dapsone in a maintenance dose (25 mg/day). Ultrasound foetal monitoring was done every fortnight till 34 weeks and thereafter every week till delivery. Subsequently, she completed her pregnancy and delivered a healthy male baby; currently, he is nine months old, and there is no evidence of neonatal lupus erythematosus.

- Histopathology of skin; subepidermal cleft with proteinaceous material with neutrophils and eosinophils. Moderate infiltrate of lymphocytes, eosinophils and histiocytes in superficial dermis (H&E stain, ×400)
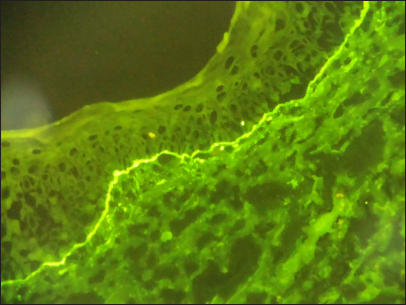
- Direct immunofluorescence study of biopsy from perilesional skin; strong IgG and weak IgA deposits along the basement membrane (FITC, ×200)
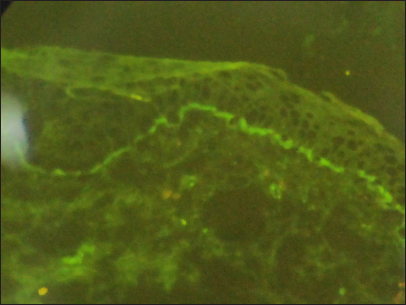
- Indirect immunofluorescence study on salt split skin; strong IgG and weak IgA deposits on the floor of the blister. (FITC, ×200)
The diagnosis of bullous systemic lupus erythematosus type II was established according to the criteria propounded by Camisa and Sharma.2 Gamman et al. have elucidated the role of immune complex-mediated inflammation in the pathogenesis of blister formation in bullous systemic lupus erythematosus. The pathogenic autoantibodies are directed against type VII collagen. It has been demonstrated in vitro studies that these antibodies activate complement and produce peptides that stimulate neutrophils and cause proteolysis resulting in dermo-epidermal junctional separation.3 Moreover, autoantigens such as the Sn RNP, Ro, La, Sm, nucleosomes, and ribosomes, with the help of toll-like receptors 7, induce inflammation in systemic lupus erythematosus by driving the production of IFN alpha, TNF alpha, IL-12 and other proinflammatory cytokines.4 The disease activity of systemic lupus erythematosus may be enhanced by pregnancy, and it may precipitate flares. Moreover, it has been reported that flares are highest during the second trimester of pregnancy and postpartum, which are attributed to lower levels of oestradiol and progesterone during the second trimester of pregnancy and decreased levels of steroid and elevated levels of prolactin during postpartum period.5 In consistence, the present patient experienced a flare with generalized bullous eruption during the second trimester of pregnancy. However, the patient did not manifest a flare during postpartum. Skin and joints are frequently involved during flares. Notably, bullous lesions in systemic lupus erythematosus are rare; only less than 5% of systemic lupus erythematosus patients develop bullous lesions. Moreover, the occurrence of bullous lesions in systemic lupus erythematosus is a pointer to the development of bullous systemic lupus erythematosus.6 Pregnancies in systemic lupus erythematosus are considered high-risk as they are prone to maternal and foetal complications. Smyth et al. conducted a recent meta-analysis involving 2571 pregnancies in systemic lupus erythematosus, and reported unsuccessful pregnancies in 23% and preterm births in 39%, while maternal complications reported were hypertension (16%), nephritis (16%), and pre-eclampsia (7%).7 There seems to be a correlation between blisters and renal involvement in bullous systemic lupus erythematosus, and most authors observed that the bullous eruption coincided with disease activity.8 Moreover, Huong et al. have reported renal involvement in 30.7% of systemic lupus erythematosus patients (n = 180).9 Nonetheless, there is no evidence of renal involvement in the present case. She is under observation for systemic involvement. Anaemia may be explained by iron deficiency. Additionally, autoantibodies in systemic lupus erythematosus might have caused impairment of erythropoietin production, leading to reduced iron metabolism and erythropoiesis.
Camisa and Sharma first reported the potential association between bullous systemic lupus erythematosus and glomerulonephritis.2 Furthermore, they reported a high incidence of IgA deposits along the basement membrane zone in patients with bullous systemic lupus erythematosus. However, there was no evidence of glomerulonephritis even though there were weak IgA deposits along the basement membrane zone in the present case.
The occurrence of bullous systemic lupus erythematosus in pregnancy is very rare, and so far, only three cases have been reported [Table 1].10-12 Interestingly, all three were known cases of systemic lupus erythematosus and developed bullous systemic lupus erythematosus in the first and second trimesters of pregnancy. Conversely, the present patient was diagnosed as bullous systemic lupus erythematosus without pre-existing systemic lupus erythematosus. Notably, all the reported cases developed systemic involvement during pregnancy, including nephritis, septicemia and central nervous system involvement, and were managed with systemic steroids, dapsone, azathioprine, hydroxychloroquine and broad-spectrum antibiotics, which resulted in favorable pregnancy outcome However, the present patient had no systemic involvement and was managed with only dapsone resulting in a successful outcome.
| Authors | Age of patient in years | Duration of SLE | Trimester | System involved | Treatment received | Pregnancy outcome |
|---|---|---|---|---|---|---|
| Goncalves et al. (2006)10 | 25 | 2 years | 2nd | Renal CNS |
Prednisolone 40 mg/day | Delivered healthy baby |
| Santos et al. (2013)11 | 25 | 1 year | 1st | Secondary bacterial infection | Prednisolone 40 mg/day Hydroxychloroquine Broad spectrum antibiotics |
Intra-uterine growth retardation |
| Vinicki et al. (2016)12 | 23 | 6 months | 1st | Renal | Prednisolone 1 mg/kg/day Azathioprine 2 mg/kg/day Dapsone 100 mg/day |
Postpartum details unavailable. Lost to follow up |
| Current report | 24 | Not known case of SLE | 1st | No | Dapsone 100 mg/day | Delivered healthy male baby |
SLE: systemic lupus erythematosus
Bullous systemic lupus erythematosus usually does not respond to systemic steroids, unlike the other manifestations of systemic lupus erythematosus [Table 2]. Dapsone (25–50 mg daily) is the drug of choice in bullous systemic lupus erythematosus and it can arrest the development of blisters within 24–48 hours, but requires continuation for 6–12 months as there is a likelihood of relapse after discontinuation. The European League Against Rheumatism task force 2016 recommended certain drugs in the management of rheumatic diseases during pregnancy, such as antimalarials, azathioprine, cyclosporine, intravenous immunoglobulin, infliximab and etanercept, as these drugs are not associated with miscarriages and congenital malformations. Conversely, certain drugs such as cyclophosphamide, rituximab, methotrexate and tacrolimus are not recommended by the European League Against Rheumatism task force as they may promote miscarriages and congenital malformations.13
| Bullous SLE | SLE | |
|---|---|---|
| Clinical features | Vesiculobullous lesions often on the background of erythema or urticaria involving upper trunk, proximal extremities, neck and face. Mucosal ulceration + |
Photosensitive rash involving malar area of face. Mucosal ulceration: ++ |
| Diagnostic criteria | Camisa and Sharma criteria (all 5 criteria) | ARA criteria (4 or more) |
| Treatment | Dapsone- drug of choice No response to systemic steroids |
Systemic steroid as indicated Immunosuppressive drugs |
| Time for response to treatment | Rapid response 24–48 hours | longer |
| Risk to mother | Low risk | High risk |
| Risk to foetus | Low risk | High risk |
SLE: systemic lupus erythematosus
In conclusion, bullous systemic lupus erythematosus in pregnancy poses a diagnostic and therapeutic challenge. It demands meticulous diligence for appropriate investigations and early therapy, as it affects both maternal and foetal health.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Bullous eruption of systemic lupus erythematosus In: Wojnarowska F, Briggaman RA, eds. Management of Blistering Diseases. London: Chapman and Hall Ltd; 1990. p. :263-75.
- [Google Scholar]
- Vesiculobullous systemic lupus erythematosus. Report of two cases and a review of the literature. J Am Acad Dermatol. 1983;9:924-33.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence supporting a role for immune complex-mediated inflammation in the pathogenesis of bullous lesions of systemic lupus erythematosus. J Invest Dermatol. 1983;81:320-5.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanism of auto antibody production in systemic lupus erythematosus. Front Immunol. 2015;6:228.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges of lupus pregnancies. Rheumatology (Oxford). 2008;47(Suppl):9-12. iii
- [CrossRef] [PubMed] [Google Scholar]
- Bullous lupus: An unusual initial presentation of systemic lupus erythematosus in an adolescent girl. Pediatr Dermatol. 2010;4:373-6.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review and meta-analysis of pregnancy outcomes in patients with systemic lupus erythematosus and lupus nephritis. Clin J Am Soc Nephrol. 2010;5:2060-8.
- [CrossRef] [PubMed] [Google Scholar]
- Concomitant lupus nephritis and bullous eruption in systemic lupus erythematosus. Nephrol Dial Transplant. 1999;14:1739-43.
- [CrossRef] [PubMed] [Google Scholar]
- Renal involvement in systemic lupus erythematosus. A study of 180 patients from a single center. Medicine (Baltimore). 1999;78:148-66.
- [CrossRef] [PubMed] [Google Scholar]
- Bullous systemic lupus erythematosus: A case report. FC–08–006. Abstracts of the European Congress of Perinatal and Neonatal Medicine 2006
- [Google Scholar]
- Bullous systemic lupus erythematosus in a pregnant woman: A case report. Rev Bras Rheumatol. 2013;53:438-40.
- [PubMed] [Google Scholar]
- Bullous systemic lupus erythematosus in a pregnant woman associated with lupus nephritis responding to dapsone. J Rheumatol Arthritic Dis. 2016;1:1-3.
- [Google Scholar]
- Steroid hormones and disease activity during pregnancy in systemic lupus erythematosus. Arthritis Rheum. 2002;47:202-9.
- [CrossRef] [PubMed] [Google Scholar]





