Translate this page into:
Calcified dyspigmented plaques, discharging sinuses and guttate hypopigmentation: An unusual clinical presentation of clinically amyopathic dermatomyositis
Corresponding author: Dr. Vishal Gupta, Assistant Professor, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. doctor.vishalgupta@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kharghoria G, Ahuja R, Arava S, Jana M, Gupta V. Calcified dyspigmented plaques, discharging sinuses and guttate hypopigmentation: An unusual clinical presentation of clinically amyopathic dermatomyositis. Indian J Dermatol Venereol Leprol 2023;89:90-4.
Sir,
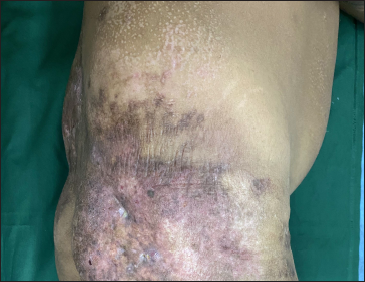
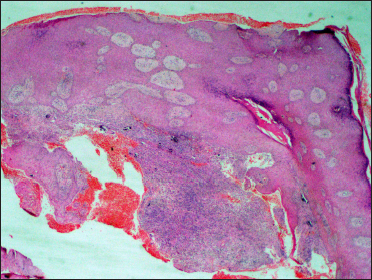
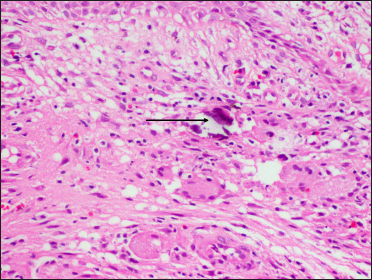
A 30-year-old male presented with mildly painful gradually increasing erythematous plaques on the lower back and right buttock for the last four years. The plaque on the right buttock developed sinuses 1½ years back, with a history of watery discharge and occasional whitish material from the sinuses. There were no systemic complaints. He had been previously treated elsewhere with antitubercular treatment, based on a skin biopsy showing granulomatous inflammation, for one month without much improvement. Examination revealed erythematous-to-dyspigmented, tender depressed indurated plaques, of size ranging from 15 × 10 cm to 30 × 20 cm, over the left lower back, right buttock extending to the postero-lateral thigh, and right medial thigh [Figure 1a]. There were two active sinuses overlying the plaque on the right buttock [Figure 1b]. Similar, but smaller (3 × 4 cm), plaques were also noted on the chest and right upper arm. Additionally, there were clustered guttate hypopigmented atrophic papules, coalescing to form plaques on the trunk and bilateral arms and thighs [Figure 1c and d]. The rest of the mucocutaneous and systemic examination was unremarkable. The patient was investigated with the differential diagnosis of cutaneous tuberculosis, atypical mycobacterial infection and deep mycoses. Complete haemogram and serum biochemistry were within normal limits, except for an elevated erythrocyte sedimentation rate (115 mm/hour) and C-reactive protein (1.6 mg/L, upper limit <0.5 mg/L). Mantoux test was negative. Enzyme linked immunosorbent assay for HIV-1 and -2 was negative. Skin biopsy from the edge of the sinus on the right buttock plaque showed a granulomatous tissue reaction, with small calcium deposits [Figure 2a and 2b]. Special stains and tissue culture for bacteria, mycobacteria and fungi were negative. Another biopsy from the buttock plaque showed features of hyalinising lobular panniculitis [Figure 2c], while those from the plaques on the right thigh and chest, as well as the hypopigmented papules, showed features of atrophic vacuolar interface dermatitis with dermal mucin deposition [Figures 3a and b]. An X-ray of the right hip joint and thigh showed soft tissue calcification, while a contrast-enhanced computerised tomography of chest, abdomen and pelvis also showed skin and subcutaneous tissue calcification in the upper anterior chest, lower back and around bilateral hip joints [Figure 4]. In light of these findings, the diagnostic possibility was revised to a connective tissue disease. Indirect immunofluorescence for antinuclear antibodies was negative; serum creatinine phosphokinase (80 U/L, range 39–308 U/L) was normal, while lactate dehydrogenase (337 U/L, range 135–225U/L) was slightly elevated, and the electromyographic study showed an inflammatory myopathic pattern. Evaluation for extractable nuclear antigen antibody profile was not carried out in view of a negative antinuclear antibodies test. A final diagnosis of autoimmune connective tissue disease, possibly hypomyopathic dermatomyositis was made. The patient was initiated on oral prednisolone 1 mg/kg/day, methotrexate 15 mg/week, and hydroxychloroquine 300 mg/day, along with oral diltiazem 240 mg/day for calcinosis. The guttate hypopigmented papules disappeared completely within two months. There was not much improvement in the right buttock plaque and sinuses over the next six months, while the other plaques on the lower back, chest and right upper arm showed significant improvement. At this time, the patient developed persistent transaminitis, and methotrexate was stopped. Monthly corticosteroid pulses (dexamethasone 100 mg × 3 days) were added in view of the lack of response of the right buttock plaque. Until the last follow-up, the patient has received six dexamethasone pulses, and prednisolone has been tapered and stopped with significant softening of the right buttock plaque and healing of sinuses [Figure 5].
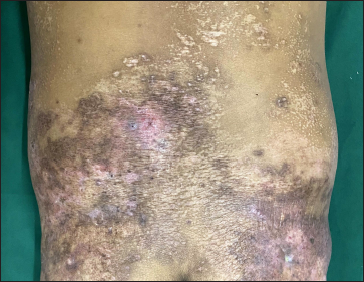
- Ill-defined depressed dyspigmented plaques over the lower back extending to the buttocks. Note the multiple guttate hypopigmented papules and plaques on the back
- Lateral view shows active sinuses over the plaque on right buttock.

- Dyspigmented plaques on the right chest and shoulder, and guttate hypopigmented papules on the left chest

- Guttate hypopigmented papules, and some coalescing to form plaques, on the upper back
- Histopathology from the edge of sinus showing irregular epidermal acanthosis and dense upper dermal inflammatory infiltrate (H&E, ×40)
- Histopathology from the edge of sinus showing a granulomatous tissue reaction with epithelioid cells, Langhans giant cells and calcium deposits (arrow) in the dermis (H&E, ×400)
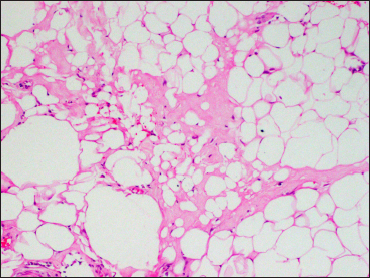
- Histopathology from the buttock plaque showing lobular panniculitis with hyaline necrosis, and macrocyst and microcyst formation (H&E, ×400)
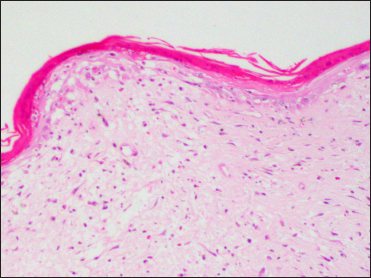
- Histopathology from the hypopigmented papule showing an atrophic epidermis, necrotic keratinocytes with vacuolar interface dermatitis (H&E, ×100)
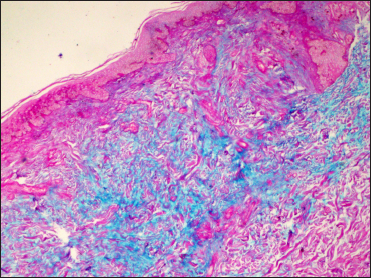
- Prominent dermal mucin deposition (Alcian blue, ×100)
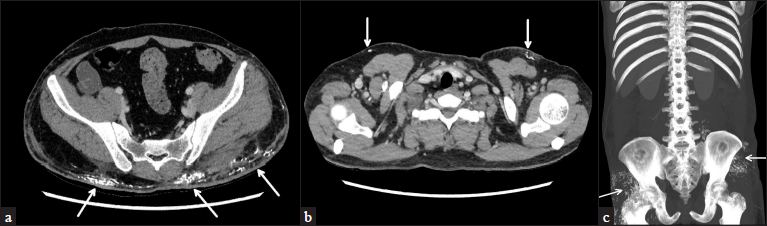
- CECT of chest, abdomen and pelvis showing multiple areas of soft tissue calcification (arrows) over (a) upper anterior chest, (b) lower back and (c) around bilateral hip joints

- Resolution of the dyspigmented plaques over lower back and right buttock. Guttate hypopigmented papules over the lower back have completely resolved

- Lateral view showing healed sinuses over the plaque on right buttock

- Residual post-inflammatory hyperpigmentation after healing of dyspigmented plaque on right chest.

- Upper back shows complete healing of guttate hypopigmented papules and plaques
Our patient had several unusual features. The clinical presentation of inflammatory plaques with discharging sinuses coupled with granulomatous tissue reaction on histopathology made us initially suspect a chronic infectious aetiology. However, subsequent investigations revealed subcutaneous calcification underneath these plaques and repeated biopsies showed vacuolar interface dermatitis, which prompted us to reconsider our diagnosis. The dyspigmented indurated plaques, their location on fat-bearing sites such as buttocks, thighs and arms, along with hyalinizing lobular panniculitis on histopathology, and dystrophic calcification were consistent with autoimmune connective tissue disease-associated panniculitis.1,3 The dyspigmentation lacked the typical reticulate character of poikiloderma but did have the individual elements of hypo-and hyperpigmentation, along with erythema and atrophy. The sinuses and the granulomatous response could be explained by ruptured calcinosis. Panniculitis can rarely be the sole initial presentation of dermatomyositis.4 Calcinosis complicated with discharging sinuses has been previously reported in dermatomyositis.5
Apart from these features, our patient also had guttate hypopigmented atrophic papules and plaques on the trunk and proximal extremities which raised several differential diagnoses. Such hypopigmented lesions, in the setting of an autoimmune connective tissue disease, could represent the cutaneous vasculopathic sequelae (atrophie blanche’) of Degos disease,6 however the absence of preceding ulcerations and absence of suggestive histopathology and systemic manifestations, coupled with a striking response to treatment excluded this possibility. Lichen sclerosus was excluded by the lack of papillary dermal sclerosis on histopathology, while the clinical pattern did not fit well with salt-and-pepper pigmentation. Given the histological features of atrophic vacuolar interface dermatitis and dermal mucin deposition, along with an excellent response to oral corticosteroids, these lesions could represent a specific cutaneous manifestation of autoimmune connective tissue disease. However, these have not been described in dermatomyositis or other autoimmune connective tissue disease, to the best of our knowledge.
Though our patient had sub-clinical inflammatory myopathy and panniculitis with dystrophic calcification, he lacked the pathognomonic or characteristic cutaneous manifestations of dermatomyositis.7 It remains to be seen if he develops the more typical skin lesions later.
We report this case for its atypical clinical presentation. Panniculitis is an infrequent cutaneous manifestation of dermatomyositis; the overlying sinuses and the initial granulomatous histopathology initially mislead us, while the guttate hypopigmentation further added to the diagnostic challenge.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Calcinosis cutis in autoimmune connective tissue diseases. Dermatol Ther. 2012;25:195-206.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatomyositis panniculitis: Aclinicopathological and immunohistochemical study of 18 cases. J Eur Acad Dermatol Venereol. 2018;32:1352-59.
- [CrossRef] [PubMed] [Google Scholar]
- Update on management of connective tissue panniculitides. Dermatol Ther. 2012;25:173-82.
- [CrossRef] [PubMed] [Google Scholar]
- Covert clues: The non-hallmark cutaneous manifestations of dermatomyositis. Ann Transl Med. 2021;9:436.
- [CrossRef] [PubMed] [Google Scholar]
- Calcinosis with sinuses caused by dermatomyositis. Orthop Surg. 2010;2:316-8.
- [CrossRef] [PubMed] [Google Scholar]
- Is Degos’ disease a clinical and histological end point rather than a specific disease? J Am Acad Dermatol. 2004;50:895-9.
- [CrossRef] [PubMed] [Google Scholar]
- Polymyositis and dermatomyositis (first of two parts) N Engl J Med. 1975;292:344-7.
- [CrossRef] [PubMed] [Google Scholar]





