Translate this page into:
Camouflage for patients with vitiligo
2 Department of Dermatology, Amrita Institute of Medical Sciences, Kochi, Kerala, India
Correspondence Address:
Feroze Kaliyadan
Department of Dermatology, College of Medicine, King Faisal University
Saudi Arabia
| How to cite this article: Kaliyadan F, Kumar A. Camouflage for patients with vitiligo. Indian J Dermatol Venereol Leprol 2012;78:8-15 |
Abstract
Vitiligo is known to be associated with social stigma and a decreased quality of life, especially when lesions are located over the face. While there are numerous treatment options for vitiligo, most of these need a long time to produce good cosmetic results. Camouflaging the skin lesions can be a useful option in such patients. The proper use of camouflage has been shown to improve the quality of life in patients with vitiligo. In this article, we discuss the different camouflage options available in vitiligo - products and techniques with their relative advantages and disadvantages.Introduction
The noun form of the word "camouflage" can mean either "concealment by some means that alters or obscures the appearance" or "a device/stratagem used for concealment." [1] Medical camouflage is now commonly used to cover scars, imperfections and pigmentary abnormalities including vitiligo. Camouflage techniques can be especially useful in patients who do not achieve complete or immediate attractive results from dermatologic therapy for vitiligo. Training in camouflage techniques is essential because the application is different from regular foundations. [2]
History
The concept of skin camouflage developed during the Second World War when plastic surgeons associated with the British Royal Air Force (RAF) began searching for durable skin-colored preparations to help conceal burn scars. Sir Archibald McIndoe, a plastic surgery consultant to the RAF, established a patient support group - the "Guinea pig club," members of which were the first to try camouflage creams prepared by Thomas Blake, a chemist from the company Veil. Another pioneer in the area of skin camouflage was Joyce Allsworth who also started work in the field of skin camouflage during the post World War II period. She went on to establish the British Association of Skin Camouflage (BASC) practitioners. [2],[3],[4]
Importance of Camouflage in Vitiligo
Vitiligo can be associated with social stigma, especially in darker skin types. Unlike most internal illnesses, skin diseases like vitiligo are often immediately visible to others and therefore may lead to significant psychosocial consequences. Focusing on enhancing self-esteem and improving the quality of life in vitiligo patients should be an important part of the management of vitiligo. [5],[6] Studies have shown that cosmetic camouflage can definitely improve the quality of life in patients with vitiligo. Patients should also be helped in selecting and using a camouflage preparation that best suits their needs. [7],[8],[9],[10] The concept of specialist "camouflage therapists" has gained ground in some countries. A camouflage therapist may educate the patient about the techniques involved in using camouflage preparations to normalize their appearance. A proper knowledge of camouflage therapy can be a very good adjunct to other dermatological treatments for vitiligo. [3]
Classification
Camouflage in vitiligo can be broadly classified into temporary camouflage and permanent camouflage. Temporary camouflage includes liquid dyes, indigenous products, foundation-based cosmetic camouflages and self-tanning products. [11] Permanent camouflage is achieved mainly by micropigmentation/medical tattooing.
Temporary Camouflage
Liquid dyes
Potassium permanganate, indigo carmine, Bismarck brown and henna pastes were commonly used to camouflage vitiligo. All these have the disadvantage of being washed away easily. Getting a color match with the surrounding skin is also very difficult.
Indigenous preparations (Traditional Indian Preparations)
Iron fillings (Loha Bhasma) and Suvarna Karini (clay mixed with henna and oils) have been used as camouflage materials. Getting a good color match is difficult with these preparations too. [11],[12]
Foundation-based cosmetic camouflage
These are the most common and best daily use preparations available for camouflage purposes. Camouflage preparations typically contain up to 25% more pigment compared to normal make-up foundations. They also contain fillers endowed with specific optical properties. Camouflage make-up products are also waterproof and are designed such that a single application lasts a whole day. [2] Camouflage preparations are essentially facial foundations. There are four basic facial foundation formulations: oil-based, water-based, oil-free and water-free forms. The most popular facial foundations are of the liquid oil-in-water emulsion types that contain a small amount of oil in which the pigment is emulsified with a relatively large quantity of water. The primary emulsifier is usually soap, such as triethanolamine or a non-ionic surfactant. The secondary emulsifier is usually glyceryl stearate or propylene glycol stearate. [13] Facial foundations are manufactured in a variety of finishes like matte, semi-matte, moist semi-matte and shiny. Matte-finish foundations are mostly suitable for cosmetic camouflage. Foundations are also available in a variety of forms: liquid, mousse, water-containing cream, soufflι, anhydrous cream, stick, cake and shake lotion. Most camouflage preparations are formulated as creams because it is possible to incorporate increased concentrations of iron oxide into a cream formulation to provide better coverage. [14],[15]
The following considerations must be addressed in an ideal camouflage: [2],[16]
- Color: Camouflage make-up must match all skin tones and it should blend with the color of the area on the skin it is intended to cover evenly.
- Opacity: Camouflage make-up must conceal all types of skin discoloration, yielding as natural and normal an appearance as possible.
- Waterproof: Camouflage make-up must ideally be waterproof.
- Sweat resistant: The camouflage preparation should not smudge or be washed away as a result of sweating.
- Holding power: Camouflage make-up must adhere to the skin without sliding off.
- Longer wear: Camouflage make-up must provide the assurance of long wear with easy reapplication as and when needed.
- Ease of application: Camouflage make-up must be easy to apply. Complicated colors and steps may make it difficult for the patient to use daily. [2],[16]
- Non-allergic/non-comedogenic/non-photosensitizing: Camouflage products should ideally be inert, without a tendency to cause allergic contact dermatitis, photodermatitis or acne. [14]
- Sun-screening capacity: Any opaque substance applied on the skin will, by default, have sun-protection capacity. Ideally, a camouflage should have a good, homogenous sun-protection capacity.
- Ease of removal: The products should also be relatively easy to remove at the end of the day with non-alcohol-/non-acetone-based make-up removers.
- Cost-effective: All the desirable properties of a camouflage product need to be in the context of also being cost-effective.
The steps involved in testing, prescribing and using a camouflage are:
1. Ask the patient details regarding prior experience of using camouflage creams. Counsel the patient regarding the limitations of the camouflage preparation. Understand the patient′s expectations. Enquire regarding the patient′s hobbies and outdoor activities. Also, note if any topical medicine is being used that might affect the skin color. Assess the patient′s skin texture and area of involvement properly. [2],[14]
2. Clean the area of vitiligo. Ideally, the area should be cleansed, exfoliated and moisturized prior to the use of camouflage.
3. The shade of the camouflage product should be selected according to the patient′s skin tone. The color in the container does not give a true idea of the actual final result when applied on the skin; hence, all shades should be tested on the skin directly. The three factors or coordinates of the color selected that should be kept in mind are - the hue, value and intensity. Hue refers to the name of the pure color (e.g., red, green, blue, etc.). Value refers to the lightness or darkness of the color and intensity refers to the brightness (saturation) of the color. In darker skin types with vitiligo, the common hues required are brown and pink. Most camouflage products have a wide range of values and intensities for each hue.
4. The steps for actual application of the cosmetic camouflage are as follows [Figure - 1],[Figure - 2],[Figure - 3],[Figure - 4]: [2]
 |
| Figure 1: Mixing the shades on the dorsum of the hand |
 |
| Figure 2: Applying the camouflage |
 |
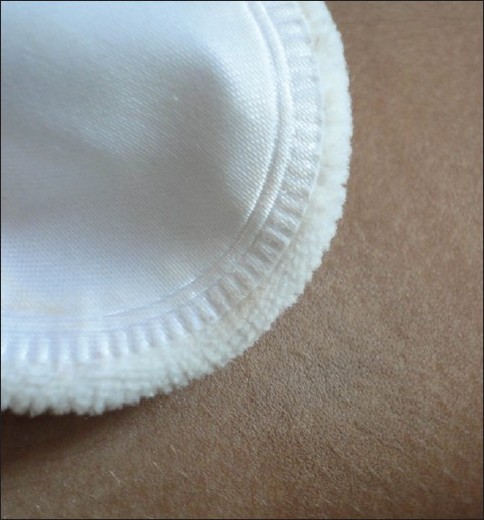
| Figure 3: Applying the fixing powder |
 |
| Figure 4: Wiping away excess powder |
- Remove a small amount of the camouflage product.
- Warm the product on the back of the hand. The idea of warming the product is to make it more malleable and thereby easier to apply.
- After this, apply over the area of vitiligo to be covered. The product is ideally applied with a sponge in a patting motion but can also be applied with the fingertips. The patting ensures that the product does not clog pores thus allowing the skin to retain its natural characteristics.
- Blend in around the edges. Blending is very important to ensure that the corrected area does not stand out by having distinct edges. Improper blending tends to defeat the whole purpose of camouflage.
- Apply the fixing powder. Facial fixing powders help to set the camouflage make-up and prevent it from smudging off. They are valuable cosmetics that provide coverage of complexion imperfections, oil control, a matte finish and increased tactile smoothness to the skin. They predominantly contain talc (hydrated magnesium silicate). [11] Fixing sprays are also available that serve the same purpose as the fixing powder. [17]
- Finally, remove any surplus powder with a brush. The time taken for the fixing powder to act depends on the patient′s skin. It is best to wait for 10 min for the powder to set before brushing off the excess powder [14] [Figure - 5]a and b and [Figure - 6]a and b.
 |
| Figure 5 (a): Localized vitiligo face Figure 5 (b): After camouflage application |
 |
| Figure 6 (a): Localized vitiligo face Figure 6 (b): After camouflage application |
Camouflaging vitiligo tends to be easier than camouflaging uneven scars as rough scars are more difficult to conceal because unevenness may be exaggerated after camouflaging. For contouring, several products have to be applied. Hypertrophic scars appear lighter than the surrounding skin, and have to be camouflaged applying a darker product than the surrounding skin. Atrophic scars, however, appear darker than the surrounding skin, and have to be corrected using a lighter product. [2],[18] However, sometimes, in extensive vitiligo of the facial area, common skin "flaws" or imperfections may need to be reproduced to give a natural look and to avoid a mask-like appearance. For example, an appearance of beard stubble can be produced in men by patting the beard area with a sponge containing black pigment. [2],[19] Another point is that it is easier to match color for lighter skin than for darker skin in general. [14] Ensure that proper sun protection is obtained. If the camouflage product does not have a sufficiently good SPF, advise applying a sunscreen prior to the application of the camouflage. [20] While removing the camouflage, advise the patient against the use of too much alcohol- or acetone-based solutions that may irritate the skin. Water-soluble make-up removers are the best. For vitiligo over the lip, stick applicators are available that are more convenient to use [Figure - 7] and [Figure - 8].
 |
| Figure 7: Lip vitiligo |
 |
| Figure 8: Lip vitiligo after camouflage |
Recently, the advent of nanotechnology has brought in the possibility of camouflage cosmetics that need not be applied as a thick layer. [21]
Practical points and tips
- It is very difficult to get an exact color match with a single shade. Usually, at least two or three different shades need to be used to get a good color match.
- In general, the skin of the face and that of the other areas of the body do not have the same color tone. Different shades of the camouflage may be therefore required over different areas.
- Shades differ from product to product. If a new product is being prescribed, it is prudent to retest over the vitiligo area to ensure that the color matches.
- Always keep a tester kit of the common products that you prescribe in your office.
- Always use a mirror to ensure that the patient is also satisfied with the result of the test camouflage.
- Make it a point to photograph and document the results before and after the camouflage process.
- The testing process should take place in a room with good lighting. Ideally, the cosmetic appearance in natural daylight should also be assessed before finalizing the shade/product.
- Patients can be encouraged to use their normal cosmetic like blushes over or along with the camouflage products on the face. This will help to accentuate their better features and takes focus away from the vitiliginous areas.
- In patients with extensive vitiligo on the exposed body areas, it should be understood that the patches tend to look conspicuous because of the sudden contrast from the dark skin to the white patches caused by the disease. One option for such extensive lesions is to blur the border showing sudden contrast with a graded color cover up without the need to cover up whole vitiligo patches. This gives good results, takes less time and needs much less camouflage product. [17]
- For younger children, parents should be educated well regarding the application techniques. Preparations that are more smudge free and have better water-proof qualities should be preferred.
Limitation of cosmetic camouflage
- Difficult to apply over larger surface area.
- Good products are relatively costly.
- Smudging/wear off of creams over hands and feet because of friction.
- Difficult to apply in patients with open lesions, severe acne and infectious skin conditions. [19]
Self-tanning products
Self-tanning products have been used effectively for the camouflage of vitiligo lesions. The most common self-tanning products used for camouflage purposes contain Dihydroxyacetone (DHA). [22],[23] DHA offers a safe and effective therapeutic option for recalcitrant vitiligo, which is also cost-effective. Subjects with dark skin need a higher concentration of DHA cream than lighter-skin subjects. [22] It temporarily stains the skin with a golden brown color by reacting with proteins in the stratum corneum to form brown chromophores, called melanoidins. [24],[25] The staining can last up to 10 days. [23] DHA also has sun-screening properties, but the SPF is very low and tends to decrease with each day of application. [23],[26]
The main disadvantage of DHA is that getting a proper color match is very difficult. Blending with the surrounding skin is also difficult to obtain. DHA has also been reported to cause allergic contact dermatitis,[27],[28] and one report has suggested that DHA can cause DNA damage and mutagenic effect on keratinocytes. [29] Both DHA and regular camouflage products can be used in patients on phototherapy. Daily use products have to be removed completely before the phototherapy session. There are no specific guidelines on the use of phototherapy while on DHA camouflage. Interestingly though, in a study by Taylor et al., [30] in 30 psoriatic patients on PUVA treatment, it was suggested that protection of uninvolved skin by DHA during PUVA treatment allows higher UV-A exposures to be tolerated, demonstrates faster clearing and requires fewer treatments to clear psoriasis. This could probably be extrapolated to the use of PUVA in vitiligo too.
Micropigmentation
Tattooing for cosmetic and medicinal purposes, referred to as either micropigmentation, dermatography or medical tattooing, may ensure permanent camouflage in a wide range of dermatological diseases. It can also be a valuable finishing step in several surgical procedures in the fields of craniofacial surgery, plastic and reconstructive operations, cosmetic surgery procedures and breast reconstruction. [31] Properly done micropigmentation procedures are associated with high patient satisfaction and low complication rates. [32]
The substances used in the process of medical micropigmentation are inert, non-toxic, non-allergenic, tissue-stable pigments with a minute particle size of about 6 μm.
Micropigmentation used to be a common mode of camouflage in recalcitrant lesions of vitiligo, especially over distal digits, lips, hands, wrists, axillae, elbows, perianal areas, lower legs, mucosae and mucocutaneous junctions. [33] However, most centers presently use micropigmentation mainly for cosmetic correction of vitiligo over the lip area. The procedure is indicated in resistant, stable and localized vitiligo. The best results are obtained in darker skin types.
Ideally, the pigment should be implanted between the superficial and middle dermis. Over the years, a small amount of this pigment may migrate to the regional lymph nodes with resultant fading. It has been observed on histopathology that the initial pigment, which is largely intracellular, gradually becomes extracellular and lies among collagen bundles, blood vessels and hair follicles without causing foreign body inflammation in the majority of cases. [34],[35]
Pigments used: Iron oxide is the most common pigment used. Various chemicals used and the respective colors produced include [Figure - 9] black, camel yellow, light and dark brown (iron oxide), white (titanium dioxide), yellow (cadmium sulfide) and red (mercuric sulfide/cinnabar, with cadmium sulfide added to make the red shade brighter). [35]
 |
| Figure 9: Tattoo gun with commonly used colors |
Pre-operative considerations: It is very important for the patient to have a realistic expectation regarding the results.
Ensure that the tattoo needles and pigment are sterilized before each procedure.
Procedure: Tattooing can be done manually, but is time-consuming. A watchmaker′s pin-vise loaded with disposable sewing needles is a cheap option for manual tattooing. [36] A variety of tattoo machines (guns/pencils) are available with different features. These include single-needle devices and multiple-needle devices. Multi-needle devices are preferred for larger patches as it is less time consuming. Single-needle devices are used for areas like the eyelids [Figure - 9].
The pigments are mixed in a Petri-dish using isopropyl alcohol to obtain a paste with a color match according to the patient′s normal skin color. A few drops of glycerin are added to prevent drying of the paste. The paste is applied over a small test site. If the results are satisfactory, the whole area is treated (it is always better to treat the whole area in the same sitting to ensure a homogenous color). The area to be to be treated should be outlined initially by tattooing a thin line or dots at the edge of the lesions. The area is then shaded within the outline by circular motions of the tattoo machine till a uniform color is obtained. Both local and systemic antibiotics are ideally needed after the procedure. The post-procedure crust and scab falls off in about 7 days. The patient can be reviewed after 4 weeks to assess if any further corrective touch-up micropigmentation is required.
Depth and density of pigment deposition: The two most important factors deciding the cosmetic results of the micropigmentation procedure are the depth and the density of pigmentation. The ideal depth is in the upper and mid-papillary dermis (about 1-2 mm depth). Deposition at a more superficial level will lead to the pigment being extruded along with the crust, while deeper deposition will lead to the pigment being leached or washed away by macrophages after a period of 2-3 months.
Density of deposition depends mainly on the consistency of the pigment paste and also the number of needles used. A thick creamy consistency of the paste ensures a better and uniform density. Similarly, a larger number of needles that are closely set will give a better pigment density. [37],[38]
Advantages
- Micropigmentation gives rapid and instantaneous results
- It is a simple office procedure and is not time consuming
- Can be used for areas like the eyelid margin where other modalities are difficult
- Relatively inexpensive procedure
Disadvantages and Limitations
- Difficulty in getting an exact color match - Other than the lips, it is often difficult to get an exact color match with the surrounding skin in patients with vitiligo. The process of color matching takes some skill, and a steep learning curve may be involved.
- Color fading - The original color tends to fade gradually and, in some patients, an unsightly bluish discoloration is seen because of the black pigment dropping down to lower levels in the deeper dermis (a "Tyndall effect" is produced imparting a slate blue discoloration). Similarly, tattoos containing certain metal oxides can become oxidized and turn black. It is often difficult to remove this pigmentation even with lasers.[35]
- The immediate adverse effects of micropigmentation usually result from improper technique and lack of adherence to asepsis. These include ecchymosis, crusting and edema lasting for a few days, reactivation of herpes simplex virus infection and secondary bacterial infection. [35],[39]
- Contact allergy to the pigments is very rare with the newer inert pigments that are used now. Reactions to tattoos can include allergic hypersensitivity and also granulomatous,[40] lichenoid [41] and pseudolymphomatous types [42] of histopathologic reactions. Photo-aggravated reactions are most commonly caused by yellow (cadmium sulfide) tattoo pigment. Most commonly, mercury (red pigment) is associated with a granulomatous tattoo reaction; however, several reactions involving chromium (green pigment) and cobalt (blue pigment) have also been reported. [40] In contrast to hypersensitivity reactions to red tattoos, reactions to pigments used to create green, blue and black tattoos are much less common. Chromium in green tattoo pigment is associated with localized eczematous reactions at the site of the pigment, eczema of the hands and generalized eczematous reactions. [43]
- The risk of transmission of infective diseases including HIV and Hepatitis B is always present, although it can be avoided by adopting proper sterilization procedures.
- Koebnerization of underlying skin diseases like lichen planus has been reported. [35]
- Micropigmentation can be effectively used only for small, localized lesions of vitiligo.
Conclusion
Properly applied camouflage techniques can help improve the patient′s appearance considerably, thereby improving the patient′s self-esteem and quality of life. For practical purposes, the best camouflage products are the foundation-based cosmetic preparations. These can be used as daily wear creams and provide the best color match options. Permanent camouflage can be done by micropigmentation, but it has to be used understanding its limitations and disadvantages.
| 1. |
Dictionary.com [Internet]. Available from: http://dictionary.reference.com/browse/camouflage. [Last cited on 2011 Aug 15].
[Google Scholar]
|
| 2. |
Bouloc A. Camouflage techniques. In: Draelos ZD, editor. Cosmetic dermatology: Products and procedures. 1 st ed. Oxford: Wiley-Blackwell; 2010. p. 176-83.
[Google Scholar]
|
| 3. |
LeRoy L. Camouflage therapy. Dermatol Nurs 2000;12 : 415-6.
[Google Scholar]
|
| 4. |
Skin camouflageadvice.com [Internet]. Available from: http://www.skincamouflageadvice.co.uk/wp-content/uploads/2010/11/Skin-Cam-Article.pdf. [Last cited on 2011 Aug 15].
[Google Scholar]
|
| 5. |
Talsania N, Lamb B, Bewley A. Vitiligo is more than skin deep: A survey of members of the vitiligo society. Clin Exp Dermatol 2010;35:736-9.
[Google Scholar]
|
| 6. |
Kent G, Al'Abadie M. Psychologic effects of vitiligo: A critical incident analysis. J Am Acad Dermatol 1996;35:895-8.
[Google Scholar]
|
| 7. |
Holme SA, Beattie PE, Fleming CJ. Cosmetic camouflage advice improves quality of life. Br J Dermatol 2002;147:946-9.
[Google Scholar]
|
| 8. |
Tedeschi A, Dall'Oglio F, Micali G, Schwartz RA, Janniger CK. Corrective camouflage in pediatric dermatology. Cutis 2007;79:110-2.
[Google Scholar]
|
| 9. |
Ongenae K, Dierckxsens L, Brochez L, van Geel N, Naeyaert JM. Quality of life and stigmatization profile in a cohort of vitiligo patients and effect of the use of camouflage. Dermatology 2005;210:279-85.
[Google Scholar]
|
| 10. |
Tanioka M, Yamamoto Y, Kato M, Miyachi Y. Camouflage for patients with vitiligo vulgaris improved their quality of life. J Cosmet Dermatol 2010;9:72-5.
[Google Scholar]
|
| 11. |
Sarveswari KN. Cosmetic camouflage in vitiligo. Indian J Dermatol 2010;55:211-4.
[Google Scholar]
|
| 12. |
Sugathan P, Nejeeba R. A new camouflage for vitiligo. Indian J Dermatol Venerol Leprol 1991;57:45-6.
[Google Scholar]
|
| 13. |
Draelos ZD. The multifunctional value of sunscreen-containing cosmetics. Skin Therapy Lett 2011;16:1-3.
[Google Scholar]
|
| 14. |
Antoniou C, Stefanaki C. Cosmetic camouflage. J Cosmet Dermatol 2006;5:297-301.
[Google Scholar]
|
| 15. |
Rayner V. Camouflaging skin lesions and other disfiguring conditions. In: Shai A, Maibach HI, Baran R, editors. Handbook of Cosmetic Skin Care. London: Martin Dunitz; 2001. p. 241-50.
[Google Scholar]
|
| 16. |
Westmore MG. Camouflage and make - up preparations. Dermatol Clin 2001;19:406-12.
[Google Scholar]
|
| 17. |
Tanioka M, Miyachi Y. Waterproof camouflage for vitiligo of the face using Cavilon 3M as a spray. Eur J Dermatol 2008;18:93-4.
[Google Scholar]
|
| 18. |
Draelos ZK. Cosmetic camouflaging techniques. Cutis 1993;52:362-4.
[Google Scholar]
|
| 19. |
Rayner VL. Camouflage therapy. Dermatol Clin 1995;13:467-72.
[Google Scholar]
|
| 20. |
Séhédic D, Hardy-Boismartel A, Couteau C, Coiffard LJ. Are cosmetic products which include an SPF appropriate for daily use? Arch Dermatol Res 2009;301:603-8.
[Google Scholar]
|
| 21. |
Kaur IP, Agrawal R. Nanotechnology: A new paradigm in cosmeceuticals. Recent Pat Drug Deliv Formul 2007;1:171-82.
[Google Scholar]
|
| 22. |
Rajatanavin N, Suwanachote S, Kulkollakarn S. Dihydroxyacetone: A safe camouflaging option in vitiligo. Int J Dermatol 2008;47:402-6.
[Google Scholar]
|
| 23. |
Hsu S. Camouflaging vitiligo with dihydroxyacetone. Dermatol Online J 2008;14:23.
[Google Scholar]
|
| 24. |
Draelos ZD. Self-tanning lotions: Are they a healthy way to achieve a tan? Am J Clin Dermatol 2002;3:317-8.
[Google Scholar]
|
| 25. |
Muizzuddin N, Marenus KD, Maes DH. Tonality of suntan vs. sunless tanning with dihydroxyacetone. Skin Res Technol 2000;6:199-204.
[Google Scholar]
|
| 26. |
Faurschou A, Wulf HC. Durability of the sun protection factor provided by dihydroxyacetone. Photodermatol Photoimmunol Photomed 2004;20:239-42.
[Google Scholar]
|
| 27. |
Zokaie S, Singh S, Wakelin SH. Allergic contact dermatitis caused by dihydroxyacetone - optimal concentration and vehicle for patch testing. Contact Dermatitis 2011;64:291-2.
[Google Scholar]
|
| 28. |
Bovenschen HJ, Körver JE, van der Valk PG. Contact dermatitis to self-tanning products. Contact Dermatitis 2009;60:290-1.
[Google Scholar]
|
| 29. |
Petersen AB, Wulf HC, Gniadecki R, Gajkowska B. Dihydroxyacetone, the active browning ingredient in sunless tanning lotions, induces DNA damage, cell-cycle block and apoptosis in cultured HaCaT keratinocytes. Mutat Res 2004;560:173-86.
[Google Scholar]
|
| 30. |
Taylor CR, Kwangsukstith C, Wimberly J, Kollias N, Anderson RR. Turbo-PUVA: Dihydroxyacetone-enhanced photochemotherapy for psoriasis: A pilot study. Arch Dermatol 1999;135:540-4.
[Google Scholar]
|
| 31. |
Vassileva S, Hristakieva E. Medical applications of tattooing. Clin Dermatol 2007;25:367-74.
[Google Scholar]
|
| 32. |
Mazza JF Jr, Rager C. Advances in cosmetic micropigmentation. Plast Reconstr Surg 1993;92:750-1.
[Google Scholar]
|
| 33. |
Halder RM, Pham HN, Breadon JY, Johnson BA. Micropigmentation for treatment of vitiligo. J Dermatol Surg Oncol 1989;15:1092-8.
[Google Scholar]
|
| 34. |
Wolfley DE, Flynn KJ, Cartwright J, Tschen A. Eyelid pigment implantation: Early and late histopathology. Plast Reconstr Surg 1988;82:770-4.
[Google Scholar]
|
| 35. |
Garg G, Thami GP. Micropigmentation: Tattooing for medical purposes. Dermatol Surg 2005;31:928-31.
[Google Scholar]
|
| 36. |
Singal A, Thami GP, Bhalla M. Watchmaker's pin-vise for manual tattooing of vitiligo. Dermatol Surg 2004;30:203-4.
[Google Scholar]
|
| 37. |
Savant SS. Tattooing versus punch grafting for nipple-areola vitiligo. Indian J Dermatol Surg 2000;2:9-25.
[Google Scholar]
|
| 38. |
Savant SS. Tattooing. In: Savant SS, editor. Textbook of Dermatosurgery and Cosmetology. 2 nd ed. Mumbai: ASCAD; 2005. p. 337-44.
[Google Scholar]
|
| 39. |
Epstein E. Therapeutic tattooing. In: Epstein E, editor. Skin Surgery. 2 nd ed. Philadelphia: Lea and Febiger; 1962. p. 308-15.
[Google Scholar]
|
| 40. |
Tazelaar DJ. Hypersensitivity to chromium in a light-blue tattoo. Dermatologica 1970;141:282-7.
[Google Scholar]
|
| 41. |
Clarke J, Black MM. Lichenoid tattoo reactions. Br J Dermatol 1979;100:451-4.
[Google Scholar]
|
| 42. |
Patrizi A, Raone B, Savoia F, Bacci F, Pileri A, Gurioli C, et al. Tattoo-associated pseudolymphomatous reaction and its successful treatment with hydroxychloroquine. Acta Derm Venereol 2009;89:327-8.
[Google Scholar]
|
| 43. |
Jacob SE, Castanedo-Tardan MP, Blyumin ML. Inflammation in green (chromium) tattoos during patch testing. Dermatitis 2008;19:33-4.
[Google Scholar]
|
Fulltext Views
20,717
PDF downloads
5,121





