Translate this page into:
Cancrum oris (noma): An early sign of acute lymphoblastic leukemia relapse
2 Department of Radiotherapy, Government Medical College, Haldwani, Uttarakhand, India
3 Department of Pulmonary Medicine, Indira Gandhi Medical College, Shimla, Himachal Pradesh, India
Correspondence Address:
Irappa Madabhavi
Department of Medical and Pediatric Oncology, Kerudi Cancer Hospital, Bagalkot, Karnataka
India
| How to cite this article: Madabhavi I, Revannasiddaiah S, Sarkar M. Cancrum oris (noma): An early sign of acute lymphoblastic leukemia relapse. Indian J Dermatol Venereol Leprol 2018;84:373 |
Sir,
We report a case of cancrum oris in an acute lymphoblastic leukemia patient from a tertiary cancer care center (Kerudi Cancer Hospital, Bagalkot, Karnataka). Cancrum oris is an infectious disease which involves the orofacial tissues and adjacent neighboring structures in its fulminating course. Cancrum oris can occur rarely in chemotherapy-induced neutropenic patients of acute lymphoblastic leukemia,[1] This rare case report reveals that cancrum oris can be a sign of acute lymphoblastic leukemia relapse.
A 27-year-old woman presented with complaints of redness and swelling of the upper lip and infranasal area. She was a known case of acute lymphoblastic leukemia diagnosed 6 months back and was on regular multiagent chemotherapy for the same. On clinical examination, there was gangrenous tissue in infranasal, intranasal and area on the upper lip [Figure - 1]. Her height, weight and body mass index were normal for her age. There was no lymphadenopathy, hepatomegaly or hepatosplenomegaly.
 |
| Figure 1: Gangrenous tissue over the infra-nasal area and upper lip |
Routine blood investigation (complete hemogram) showed normal leukocyte and platelet counts and manual differential count did not show any lymphoblasts. The bone marrow aspiration and cytology did not reveal any leukemic activity. Blood culture and swab culture from the gangrenous area, for both aerobic and anaerobic organisms were sterile. She was given 7 days of empirical antibiotics such as imipenem, vancomycin and fluconazole in view of infectious etiology. Despite 7 days broad-spectrum antibiotics, patient could not get relief of her symptoms.
With a high-degree of clinical suspicion of an isolated extramedullary relapse, fine-needle aspiration cytology from marginal and gangrenous area was taken and revealed infiltration of the soft tissues by lymphoblasts [Figure - 2]. In view of extramedullary relapse, four cycles of cyclophosphamide, vincristine and prednisolone and intrathecal methotrexate were given. After four cycles of chemotherapy, the facial lesions resolved completely and she was totally asymptomatic. At present, she is on maintenance therapy for her leukemic activity with 6-thioguanine, cytarabine, intrathecal methotrexate and oral methotrexate.
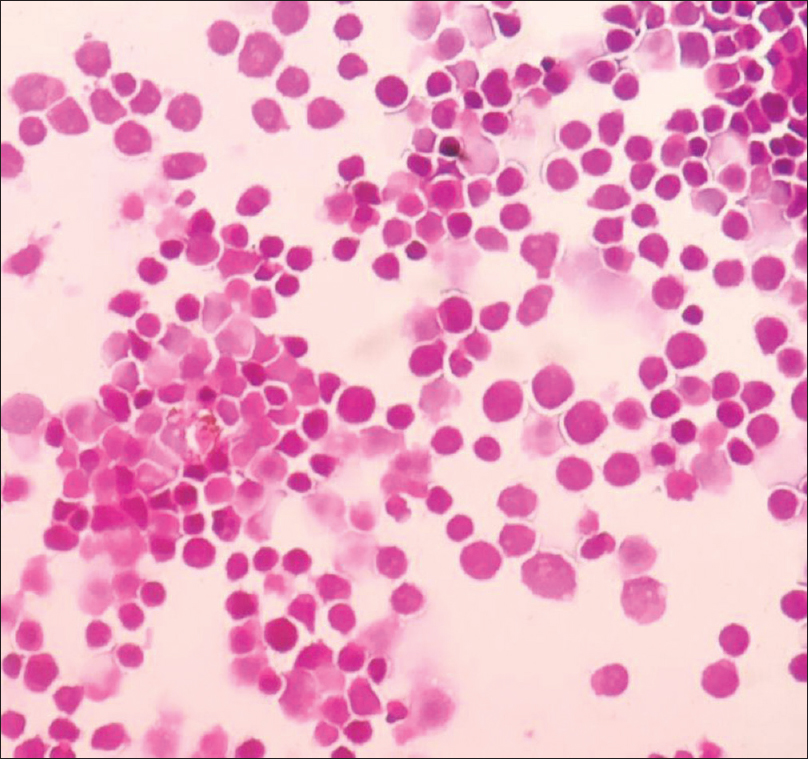 |
| Figure 2: Fine-needle aspiration cytology smear from marginal and gangrenous area showing infiltration with lymphoblasts (H and E, X100) |
Cancrum oris (noma) has been most commonly described in malnourished debilitated children with poor oral hygiene following systemic childhood infections such as measles, pertussis or scarlet fever. Treatment of cancrum oris involves correction of underlying immune status, antibiotics and surgical reconstruction. Cancrum oris as an initial presentation of extramedullary relapse of acute lymphoblastic leukemia has not yet been documented in the literature. In our case, underlying immune dysfunction due to the acute lymphoblastic leukemia may be an underlying predisposing factor.
Cancrum oris is an infectious disease which involves the orofacial tissues and adjacent neighboring structures in its fulminating course. It is not a primary disease, usually preceded by measles, tuberculosis, leukemia and acquired immunodeficiency syndrome. Malnutrition causes alteration in cell-mediated immune function resulting in early breakdown of the epithelial tissues and changes in the oral mucosa which facilitate invasion by pathogens.[2]
Cancrum oris can occur rarely in chemotherapy-induced neutropenic patients of acute lymphoblastic leukemia; but presentation as an early sign of extramedullary disease relapse has not yet been documented in the English literature. The exact causative organism is not clear although spirochetes and fusiform bacillus in symbiosis have been considered to be the primary cause of the condition.[3] There is postulation or hypothesis that evolution of oral mucosal ulcers including acute necrotizing gingivitis to noma is triggered by a consortium of microorganisms, of which Fusobacterium necrophorum is a key component. Fusobacterium necrophorum elaborates several dermonecrotic toxic metabolites that help in rapid progression of the disease and is acquired through fecal contamination.[4] The active agents against this organism are metronidazole, co-amoxiclav, chloramphenicol, cefoxitin, clindamycin and imipenem. Without appropriate treatment, the mortality rate is reported to be 70%–90% and surviving patients suffer with functional disturbances and disfigurement.
Treatment of cancrum oris involves correction of underlying immune status, antibiotics and surgical reconstruction. Correction of an underlying immune dysfunction and primary disease as in our case, the extramedullary relapse of acute lymphoblastic leukemia, is the most important treatable condition to be kept in mind.
Hence, to conclude: the rare possibility of relapse of acute lymphoblastic leukemia presenting as cancrum oris should be kept in mind in patients with acute lymphoblastic leukemia on chemotherapy with skin manifestations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Brady-West DC, Richards L, Thame J, Moosdeen F, Nicholson A. Cancrum oris (noma) in a patient with acute lymphoblastic leukaemia. A complication of chemotherapy induced neutropenia. West Indian Med J 1998;47:33-4.
[Google Scholar]
|
| 2. |
Berthold P. Noma: A forgotten disease. Dent Clin North Am 2003;47:559-74.
[Google Scholar]
|
| 3. |
Devi SR, Gogoi M. Aesthetic restoration of facial defect caused by cancrum oris: A case report. Indian J Plast Surg 2003;36:131-3.
[Google Scholar]
|
| 4. |
Enwonwu CO, Falkler WA Jr., Idigbe EO, Afolabi BM, Ibrahim M, Onwujekwe D, et al. Pathogenesis of cancrum oris (noma): Confounding interactions of malnutrition with infection. Am J Trop Med Hyg 1999;60:223-32.
[Google Scholar]
|
Fulltext Views
3,519
PDF downloads
2,417





