Translate this page into:
Characteristic patterns of segmental infantile hemangiomas in Indian children: A descriptive study
2 Consultant Dermatologist, Dr. Dhawan's Skin Clinic, Delhi, India
3 Department of Pediatrics, University College of Medical Sciences and GTB Hospital, New Delhi, India
4 Department of Radio-Diagnosis, University College of Medical Sciences and GTB Hospital, New Delhi, India
Correspondence Address:
Chander Grover
420-B, Pocket 2, Mayur Vihar, Phase-1, New Delhi - 110 091
India
| How to cite this article: Grover C, Kaul S, Dhawan AK, Narang M, Rathi V. Characteristic patterns of segmental infantile hemangiomas in Indian children: A descriptive study. Indian J Dermatol Venereol Leprol 2020;86:674-680 |
Abstract
Background: Approximately 18% of infantile hemangiomas are segmental. These are larger than other infantile hemangiomas, associated with higher rate of complications and developmental anomalies, and often require treatment. They follow nonrandom patterns on the head and neck as well as extremities which are probably related to embryologic development.
Aims: Our study aimed to describe segmental patterns of infantile hemangiomas in Indian children, with associated anatomical abnormalities if any.
Methods: Over a 9-year period, 59 infants presenting with lesions classified as segmental infantile hemangiomas were evaluated and analyzed. Associated developmental anomalies were assessed and recorded. In addition, patterns of “indeterminate” infantile hemangiomas in another 43 patients were analyzed.
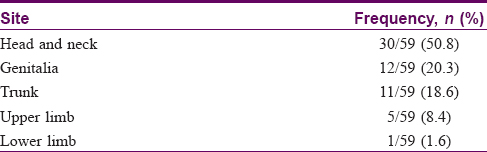
Results: There were 14 male and 45 female infants with an average birth weight of 2.7 ± 0.726 kg in our study; the average age at onset was 1 ± 1.25 months with most (50.8%) lesions localized to the head and neck area. Mapping of lesions showed that the most common facial segments involved were mandibular (33%) and maxillary (30%). However, additional repetitive patterns not previously described (such as an “inverted comma” pattern on the chest, bilateral neck involvement and unilateral labium involvement) were seen in our patients. Common local complications were ulceration (27%), amblyopia and nasal obstruction (3% each). Mapping of the additional 43 patients with indeterminate infantile hemangiomas also showed repetitive though incomplete patterns.
Limitations: Relatively small number of patients.
Conclusion: Segmental infantile hemangiomas present as large, distinctively patterned lesions, even on the trunk and genitalia. These patterns are probably based on embryologic developmental patterns. In addition, indeterminate lesions also showed distinctive repetitive patterns. Our study suggests that additional segments may need to be defined, particularly on the trunk and genital area.
Introduction
Infantile hemangiomas are the most common vascular tumors in infants.[1] They are hypothesized to originate from dysregulated stem cells arrested at an immature stage, prompting expression of genes for vasculogenesis and tumorigenesis.[2] The trigger could be localized tissue hypoxia leading to “compensatory” overgrowth after birth.[3],[4] Infantile hemangiomas evolve predictably with sequential proliferation and involution. Most require no treatment, though some lesions, impairing vital functions or causing significant disfigurement, need therapy. Infantile hemangiomas are classified on the basis of depth of involvement (superficial, deep, mixed) or morphology (localized, multifocal, segmental or indeterminate).[5],[6]
Segmental infantile hemangiomas are plaque-type lesions involving a defined cutaneous segment. They constitute almost 18% of infantile hemangioma lesions, are usually large, have a higher rate of associated developmental anomalies and require treatment more frequently.[7],[8] There is a rising interest in this subset because of the need for prompt management.
Facial segmental infantile hemangiomas have been delineated in four segments, corresponding to embryological developmental units.[7] Segmental infantile hemangioma patterns, together with associated anomalies, as in PHACE syndrome, may suggest the time of insult in utero.[7],[9],[10] Patterns of acral segmental infantile hemangiomas along embryonic arterial supply units are also described; however, literature on truncal or genital segmental infantile hemangiomas is sparse.[9] This descriptive study aimed to determine patterns of segmental and indeterminate infantile hemangiomas in Indian infants and their associations if any.
Methods
This was a retrospective case record analysis of infants with segmental infantile hemangiomas seen over a 9-year period. Case records of hemangiomas along with photographic data at presentation were analyzed. Lesions were classified as segmental, focal, multifocal or indeterminate [Figure - 1] by two dermatologists independently. Focal hemangiomas were defined as lesions which were localized without any apparent pattern [Figure - 1]a. Multifocal hemangiomas were defined as more than five lesions in a child.[7],[11] Those hemangiomas whose distribution corresponded to recognizable developmental segments were classified as segmental infantile hemangiomas [Figure - 1]b. Hemangiomas which could not be classified convincingly as either focal or segmental were deemed indeterminate [Figure - 1]c. Hemangioma morphology, local complications, pertinent history and associated developmental anomalies were noted. In case of head and neck segmental infantile hemangiomas, ophthalmological and otorhinolaryngological assessments were also done. Imaging studies viz. contrast-enhanced computed tomography of the brain and echocardiography were performed in those with a suspicion of associated developmental abnormalities, especially the large segmental hemangiomas of the face (fronto-temporal and mandibular) as they carry a high risk of associated anomalies. Ultrasonography was done for cases with a suspected deeper component, suggested by a bluish hue or swelling underneath the hemangioma.
 |
Results
A total of 59 cases classified as segmental infantile hemangiomas, and 43 classified as indeterminate, were included in the study. The 59 infants with segmental infantile hemangiomas had a total of 70 lesions. There were 45 females and 14 males (sex ratio 3.2:1). A majority (52/59, 88.1%) had a solitary lesion. The rest had focal infantile hemangiomas in addition (7 patients with 11 additional infantile hemangiomas). Of these latter, three (5.1%) infants had one additional focal infantile hemangioma, and four (6.7%) had two additional infantile hemangiomas. The frequency distribution of segmental infantile hemangiomas is presented in [Table - 1]. Head and neck segmental infantile hemangiomas (n = 30) were delineated into the segments described by Haggstrom et al.[7] The commonest segments involved were mandibular [Figure - 2]a and maxillary, followed by fronto-temporal [Figure - 2]b and fronto-nasal [Figure - 2]c. The distribution pattern and frequencies are outlined. Cases not classifiable using this system (20% of cases) included five (16.6%) with segmental infantile hemangiomas on the neck [Figure - 3]a and one (3.3%) involving the entire ear and retroauricular region [Figure - 3]b.
 |
 |
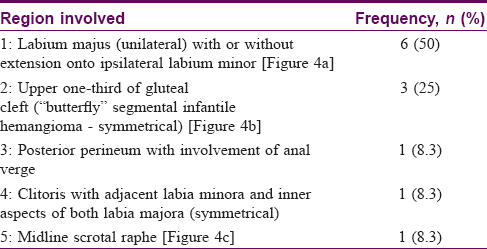
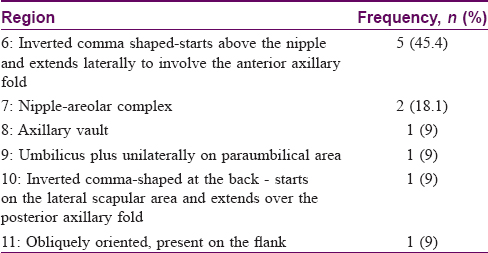
The next commonest site involved was the genital region (12/59, 20.3%). Patterns involving genitalia, not hitherto described, were mapped out [Figure - 4]a, [Figure - 4]b, [Figure - 4]c; frequencies in [Table - 2]. Segmental infantile hemangiomas on the trunk (n = 11, 18.6%) also followed recurring patterns which were mapped [frequencies in [Table - 3]. An inverted comma-shaped pattern, not described earlier, was commonly noted in this series.
 |
Upper limb segmental infantile hemangiomas (n = 5) were commonest on the forearm, with extension upto the wrist (3/5, 60%). A single case each in this category had the 'biker-glove' pattern [Figure - 5] described by Weitz et al. and a segmental infantile hemangioma on the shoulder similar to Reimer et al.'s description.[9],[10] One other case had segmental infantile hemangioma on the lower limb with the biker-glove pattern.
 |
| Figure 5: “Biker-glove” segmental infantile hemangioma |
Mucosal involvement (intranasal, oral cavity [Figure - 6] or genital) was present in 10/59 (16.9%) cases.
 |
| Figure 6: Mucosal involvement with a lip lesion |
Segmental infantile hemangiomas were divided into superficial, deep and mixed types.[5],[11] These constituted 52/70 (74.5%), 0% and 18/70 (25.4%) respectively. Segmental infantile hemangiomas posed a purely esthetic problem in 38 (64.4%) patients. Ulceration was the commonest complication, seen in 16/59 (27.1%) patients. Two (3.3%) cases each had amblyopia and nasal obstruction. There were no cardiovascular abnormalities in our patients, including two female infants suspected to have PHACES syndrome. However, there were posterior fossa abnormalities in one of these latter two infants. Two patients with mandibular segmental infantile hemangiomas had involvement of the underlying parotid gland.
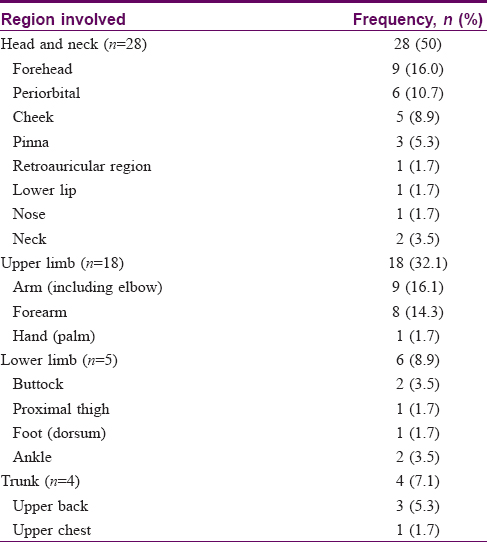
Indeterminate infantile hemangiomas were diagnosed in 43 infants. Of these, 25.5% had more than one lesion (nine infants having two lesions each and two infants having three lesions each) yielding a total of 56 hemangiomas in these patients. The head and neck region was the commonest site involved in 28 (50%) lesions, followed by 18 (32.1%) upper limb lesions, 6 (10.7%) lower limb lesions and 4 (7.1%) trunk lesions. Ulceration occurred in 20 (35.7%) indeterminate lesions. The body distribution of indeterminate segmental infantile hemangiomas is pictorially represented and detailed in [Table - 4]. Several truncal and upper limb indeterminate lesions had a mushroom-like globular growth (9/56; 16%) and were all ulcerated.
Discussion
In line with previous reports, the majority of our study population comprised female infants (M/F ratio of 1:3.2), and the head and neck region was the most common site affected (50.8%).[1],[11],[12],[13],[14] However, we found around half of the segmental infantile hemangiomas in areas other than the head and neck.
Among the head and neck segmental infantile hemangiomas, we observed mandibular segmental infantile hemangiomas (segment 3 of Haggstrom et al.) to be the most common (33%), closely followed by maxillary segmental infantile hemangiomas (segment 2 in 30%). Fronto-temporal segmental infantile hemangiomas (segment 1) accounted for 10%, whereas fronto-nasal segmental infantile hemangiomas (segment 4) were least common (6% cases). This was broadly similar to earlier reports.[7],[15] We noted that several clearly segmental lesions on the neck or ear defy classification into Haggstrom segments. Neck lesions were oriented horizontally and crossed the midline (were bilateral) [Figure - 3]a and involvement of the ear lobe (anterior and posterior) was also seen [Figure - 3]b.
Clinical patterns for segmental infantile hemangiomas of the anogenital area have not been delineated earlier. We observed unilateral labial involvement (50%) [Figure - 4]a; or involvement of the scrotum [Figure - 4]b commonly. The next most common pattern was a butterfly-shaped, bilaterally symmetrical lesion on the upper third of the gluteal cleft (25%) [Figure - 4]c. Embryological development of the external genitalia could explain this. An indifferent external genital organ developing from the cloacal folds is discernible at the third week; from this, the genital tubercle, urethral folds and anal folds are formed. A second pair of swellings (genital folds) gives rise to the labia majora in the female and scrotum in males (the latter by fusion). Development is completed by the sixth week, suggesting that unilateral lesions may be due to a hypoxic insult between 3 and 6 weeks of intrauterine life.[16]
We also observed distinctive patterns in truncal segmental infantile hemangiomas, the commonest being an inverted comma-like lesion. These involved the upper chest (sparing the nipple) extending upwards and laterally up to the anterior axillary fold. Fetal upper limb development begins on the 24th day of life, with small bulges appearing at the lower cervical region. By day 33, the rudimentary shoulder, arm, forearm and hand plate can be distinguished.[17] The “inverted comma” segmental infantile hemangioma (extending from upper chest onto the anterior part of shoulder) hints at a hypoxic event probably around the time of appearance of upper limb buds.
Patterns of upper and lower limb segmental infantile hemangiomas have been reported by Reimer et al. One frequent pattern noted in their study and ours was segmental infantile hemangiomas on the radial forearm with extension to the wrist, which probably correlates with the area supplied by the superficial brachio-ulnar-radial or superficial brachio-ulnar artery.[9] The recently described “biker-glove pattern” (infantile hemangioma involving hands or feet with a contiguous border and sparing of digital tips) [Figure - 5] was seen in only one upper limb and one lower limb segmental infantile hemangioma respectively in our study. However, Weitz et al. found it to be the predominant pattern in upper and lower limb segmental infantile hemangiomas, comprising 73% of their cases.[10]
Superficial segmental infantile hemangiomas comprised the majority (74.5%); the remaining were of the mixed type. This was similar to earlier reports, where the superficial type contributed to >50% of infantile hemangiomas, though some reports have found the mixed subtype to be most common.[7],[18] As in our study, ulceration is by far the most commonly reported complication in literature.[14],[15],[18],[19] In contrast to the present study, parotid gland involvement as high as 39% was recorded by Bradling-Bennett et al. This large difference is probably attributable to the higher number of deep infantile hemangiomas included in their study.[15] Our findings suggest that although segmental infantile hemangiomas can indicate associated underlying abnormalities, only a minority are found to have associated anomalies on investigation.
Indeterminate infantile hemangiomas are considered an incomplete or abortive form of segmental infantile hemangiomas. This was partially supported by our study findings as these too tended to follow repetitive patterns. Further mapping may help gain clarity and possibly better classify them as segmental lesions.
Limitations
Our study describes patients with segmental infantile hemangiomas; as these constitute a minority of infantile hemangiomas seen in practice, a small study population was the main drawback of our study.
Conclusion
Genital and truncal segmental infantile hemangiomas were found to be next in order of frequency to head and neck lesions. Novel repetitive patterns such as a truncal “inverted comma” pattern and unilateral genital lesions should be looked for. Even indeterminate lesions share patterns similar to segmental lesions. Future evaluation of more patients could refine classification, perhaps offering further insights into hemangioma pathogenesis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Abraham A, Job AM, Roga G. Approach to infantile hemangiomas. Indian J Dermatol 2016;61:181-6.
[Google Scholar]
|
| 2. |
Harbi S, Wang R, Gregory M, Hanson N, Kobylarz K, Ryan K, et al. Infantile hemangioma originates from A dysregulated but not fully transformed multipotent stem cell. Sci Rep 2016;6:35811.
[Google Scholar]
|
| 3. |
de Jong S, Itinteang T, Withers AH, Davis PF, Tan ST. Does hypoxia play a role in infantile hemangioma? Arch Dermatol Res 2016;308:219-27.
[Google Scholar]
|
| 4. |
Itinteang T, Withers AH, Davis PF, Tan ST. Biology of infantile hemangioma. Front Surg 2014;1:38.
[Google Scholar]
|
| 5. |
Higgins EM, Glover MT. Dermatoses and Haemangiomas of Infancy. In: Rook's Textbook of Dermatology. 9th ed. New Delhi: Wiley-Blackwell; 2016. p. 117.16-117.23.
[Google Scholar]
|
| 6. |
Chiller KG, Passaro D, Frieden IJ. Hemangiomas of infancy: Clinical characteristics, morphologic subtypes, and their relationship to race, ethnicity, and sex. Arch Dermatol 2002;138:1567-76.
[Google Scholar]
|
| 7. |
Haggstrom AN, Lammer EJ, Schneider RA, Marcucio R, Frieden IJ. Patterns of infantile hemangiomas: New clues to hemangioma pathogenesis and embryonic facial development. Pediatrics 2006;117:698-703.
[Google Scholar]
|
| 8. |
Metry DW, Hawrot A, Altman C, Frieden IJ. Association of solitary, segmental hemangiomas of the skin with visceral hemangiomatosis. Arch Dermatol 2004;140:591-6.
[Google Scholar]
|
| 9. |
Reimer A, Fliesser M, Hoeger PH. Anatomical patterns of infantile hemangioma (IH) of the extremities (IHE). J Am Acad Dermatol 2016;75:556-63.
[Google Scholar]
|
| 10. |
Weitz NA, Bayer ML, Baselga E, Torres M, Siegel D, Drolet BA, et al. The “biker-glove” pattern of segmental infantile hemangiomas on the hands and feet. J Am Acad Dermatol 2014;71:542-7.
[Google Scholar]
|
| 11. |
Léauté-Labrèze C, Harper JI, Hoeger PH. Infantile haemangioma. Lancet 2017;390:85-94.
[Google Scholar]
|
| 12. |
Hemangioma Investigator Group, Haggstrom AN, Drolet BA, Baselga E, Chamlin SL, Garzon MC, et al. Prospective study of infantile hemangiomas: Demographic, prenatal, and perinatal characteristics. J Pediatr 2007;150:291-4.
[Google Scholar]
|
| 13. |
Kwon EK, Seefeldt M, Drolet BA. Infantile hemangiomas: An update. Am J Clin Dermatol 2013;14:111-23.
[Google Scholar]
|
| 14. |
Haggstrom AN, Drolet BA, Baselga E, Chamlin SL, Garzon MC, Horii KA, et al. Prospective study of infantile hemangiomas: Clinical characteristics predicting complications and treatment. Pediatrics 2006;118:882-7.
[Google Scholar]
|
| 15. |
Brandling-Bennett HA, Metry DW, Baselga E, Lucky AW, Adams DM, Cordisco MR, et al. Infantile hemangiomas with unusually prolonged growth phase: A case series. Arch Dermatol 2008;144:1632-7.
[Google Scholar]
|
| 16. |
Sadler TW. Urogenital system. In: Langman's Medical Embryology. 13th ed. China: Wolters Kluwer Health; 2015. p. 250-77.
[Google Scholar]
|
| 17. |
Schoenwolf G, Larsen W, editors. Larsen's Human Embryology. Philadelphia (PA): Churchill Livingstone/Elsevier; 2009.
[Google Scholar]
|
| 18. |
Castrén E, Salminen P, Gissler M, Stefanovic V, Pitkäranta A, Klockars T, et al. Risk factors and morbidity of infantile haemangioma: Preterm birth promotes ulceration. Acta Paediatr 2016;105:940-5.
[Google Scholar]
|
| 19. |
Kim HJ, Colombo M, Frieden IJ. Ulcerated hemangiomas: Clinical characteristics and response to therapy. J Am Acad Dermatol 2001;44:962-72.
[Google Scholar]
|
Fulltext Views
5,564
PDF downloads
2,454





