Translate this page into:
Childhood granulomatous periorificial dermatitis in children with extra-facial involvement
Correspondence Address:
Uday Khopkar
Department of Dermatology, Seth GS Medical College and KEM Hospital, Parel, Mumbai - 400 012
India
| How to cite this article: Gutte R, Holmukhe S, Garg G, Kharkar V, Khopkar U. Childhood granulomatous periorificial dermatitis in children with extra-facial involvement. Indian J Dermatol Venereol Leprol 2011;77:703-706 |
Abstract
Childhood granulomatous periorificial dermatitis (CGPD) is a self-limiting and well-recognized entity. A six-year-old male child, a known case of juvenile rheumatoid arthritis (JRA) presented with multiple red raised and yellowish lesions over the face, neck, trunk and upper extremities since one month with occasional itching. Cutaneous examination revealed multiple erythematous scaly papules of size up to 5 mm around the mouth, nose and periorbital areas, neck, trunk and upper extremities with few excoriations. Lesional skin biopsy was pathognomic of CGPD. We report a six-year-old Indian male child with extra-facial involvement and healing with small atrophic pigmented scars in a known case of JRA.Introduction
Childhood granulomatous periorificial dermatitis (CGPD) is also known as facial Afro-Caribbean childhood eruption (FACE), Gianotti-type perioral dermatitis and sarcoid-like granulomatous dermatitis. Though more common in dark races it also occurs in white patients. It occurs in healthy prepubertal children, affecting both sexes, characterized by monomorphous papular eruption around the mouth, nose and eyes with occasional extra-facial involvement clinically and upper dermal perifollicular granuloma histologically. It should be differentiated from sarcoidosis, rosacea, acne and perioral dermatitis both clinically and histologically. [1],[2] Gianotti et al., reported a case with monomorphic papules around the mouth and granulomatous pattern on histology in 1970. [3] Since then many cases have been reported. We report a case of CGPD in a six-year-old Indian male child with extra-facial involvement and self-limiting course. The correct diagnosis is important to minimize treatment as CGPD is ultimately benign and self-limiting.
To the best of our knowledge no such case has been reported from India.
Case Report
A six-year-old male child a known case of juvenile rheumatoid arthritis (JRA) on treatment with prednisolone 10 mg/day and methotrexate (10 mg/week for six months and 5 mg/week since the last three months) presented with multiple red raised and yellowish lesions over the face, neck, trunk and upper extremities since one month with occasional itching. There was history of anti-tuberculous therapy for one year for pulmonary tuberculosis stopped one year back. There was no history of atopy, photosensitivity or any irritant application. He had no pain or swelling of joints since the last four months. Family history was non-contributory. Differential diagnosis of miliaria profunda, childhood acne and lupus miliaris disseminatus faciei were considered.
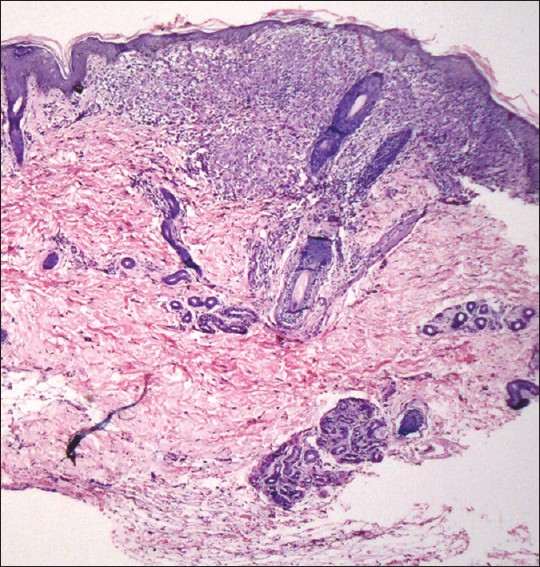
On examination the child was thin-built and stunted. His height was 102 cm and weight was 11 kg. There were multiple erythematous scaly papules of size up to 5 mm around the mouth, nose and periorbital areas [Figure - 1], neck, trunk and upper extremities with a few excoriations [Figure - 2]. Palms, soles, nails, mucosae, genitalia and the rest of the examination revealed no abnormality.
 |
| Figure 1: Multiple erythematous scaly papules over the face |
 |
| Figure 2: Multiple erythematous scaly papules over bilateral upper extremities |
Routine investigations revealed hemoglobin 9.3 g/dl, erythrocyte sedimentation rate 25 mm at the end of 1 h, normal liver and kidney function tests, electrolytes, lipid profile and serum proteins. Radiograph of the skull, chest and ultrasound of abdomen were also normal. Montoux test was negative and so also tests for rheumatoid factor, anti-nuclear and anti-dsDNA antibodies.
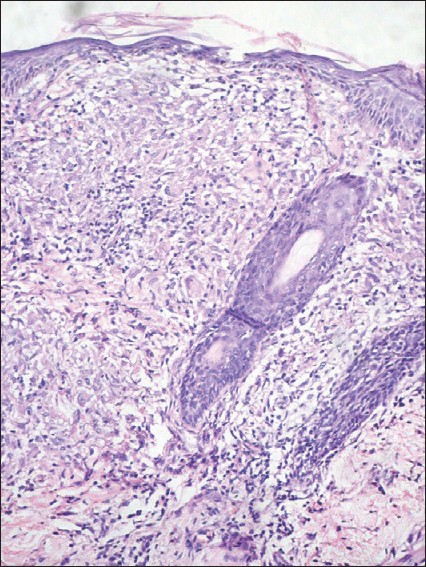
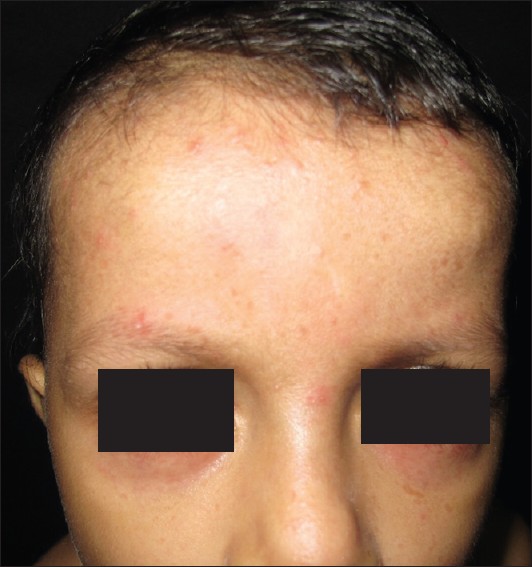
A lesional skin biopsy showed mild hyperkeratosis over a normal epidermis and a well-formed granuloma containing numerous lymphocytes, histiocytes, and giant cells within the upper dermis in a perifollicular distribution. Subcutaneous tissue appeared normal [Figure - 3] and [Figure - 4]. Special stains for organisms including periodic acid Schiff, Gram′s stain and Fite-Faraco satin were negative. On clinico-pathologic correlation a diagnosis of childhood granulomatous periorificial dermatitis was made.
 |
| Figure 3: Perifollicular infiltrate in the upper dermis (H and E, ×10) |
 |
| Figure 4: Perifollicular granuloma in the upper dermis with lymphocytes and foreign body type giant cell (H and E, ×20) |
The patient was treated with syrup amoxicillin clavulanic acid, syrup chlorpheniramine and moisturizers. His lesions subsided completely with pigmentation and small atrophic pits and pinpoint scarring at places over a period of a month [Figure - 5]. No recurrence has been seen till now.
 |
| Figure 5: Lesions subsided with small atrophic pigmented scars over face |
Discussion
Childhood granulomatous periorificial dermatitis is a distinctive disorder of otherwise healthy pre-pubertal children. The precise etiology of this benign and self-limiting entity is not known. This relatively uncommon condition is characterized by monomorphous, dome-shaped, skin-colored to yellowish-brown papular eruption with occasional overlying scale affecting the perioral, peri-ocular and perinasal areas predominantly. A few cases with extra-facial involvement affecting the neck, trunk, extremities and genital involvement have been reported. [1],[4] Involvement of the neck, trunk and extremities was seen in our case too. It is usually asymptomatic but occasionally pruritus may be associated. This benign dermatosis is not associated with any systemic involvement or serious sequelae and heals without scarring, but in a few cases atrophic pits and scarring as was seen in our case is reported. [4] We considered the presence of JRA and past history of pulmonary tuberculosis in our case as a coincidence.
Histopathologically it shows upper dermal non-caseating granulomas with predilection for follicle and perifollicular dermis and mixed infiltrate of lymphocytes, histiocytes with occasional epidermal changes like hyperkeratosis, acanthosis and spongiosis. [4],[5]
It was first reported in the French literature in 1970 by Gianotti et al., in five children with additional four children reported in 1975 with a perioral eruption. [3],[5]
It should be differentiated from sarcoidosis (rare under the age of 15 years and usually associated with systemic involvement), perioral dermatitis (more common in women in the third to fourth decade, papulopustules and papulovesicular lesions with erythema and scaling and sparing of narrow zone around lips), lupus milaris disseminatous faciei (adult onset, more common in females, chronic course, central face and eyelid predilection, caseating granuloma on histology and heals with severe, depressed scars), acne (has inflammatory pustules, comedones and affects postpubertal children with chronic course) and granulomatous rosacea (presents with facial erythema, telengiectasias, flushing and no spontaneous regression), and papular eruption of black (seen in adult black and spares the face). Blau syndrome, also known as familial juvenile systemic granulomatosis, is characterized by asymptomatic skin lesions of varying morphology that have been described as eczematous, ichthyosiform, and lichenoid. Rheumatoid factor is often positive, a finding not typical of patients with JRA and has more systemic involvement. [5],[6],[7],[8] Causes for cutaneous granulomas in rheumatoid arthritis include rheumatoid nodule, interstitial granulomatous dermatitis with arthritis, palisaded neutrophilic and granulmatous dermatitis. [9]
Treatment options based on anecdotal reports are topical metronidazole, tetracycline, erythromycin, clindamycin with or without oral antibiotics like macrolides, doxycycline, tetracycline and minocycline. [2],[4] A rapid resolution of lesions with topical tacrolimus and oral minocycline have been observed by Misago et al., [2] however, topical steroids are known to initiate and exacerbate the condition and should be avoided. [1],[4]
The importance of recognizing this condition lies in its self-limiting and purely cutaneous nature, exacerbation by topical steroids, reassuring patient and family members, and avoidance of extensive investigations and limiting treatment. [7] Childhood granulomatous periorificial dermatitis is known by various names (vide supra) creating confusion and various diagnostic labels for essentially the same disease process.
"An unusual papular and acneiform facial eruption in the Negro child" as called by Marten et al., is not only cumbersome to remember but also socially unacceptable. [6],[7] Moreover "perioral dermatitis" is a misnomer as there is frequent perinasal, periocular and occasionally extra-facial involvement with features distinct from traditional perioral dermatitis. "Facial Afro-Caribbean childhood eruption" (FACE) may be under-diagnosed in the white population. "Granulomatous perioral dermatitis in children" as called by Frieden et al., is also misleading as it also affects other sites and these is lack of erythema and pustules. [1],[5],[7] Absence of granuloma on histology in some cases makes the term "childhood granulomatous periorificial dermatitis" also unsuitable. [7] "Gianotti-type perioral dermatitis" and "Sarcoid-like granulomatous dermatitis" as a synonym [1] serve no purpose other than increasing confusion. We prefer the term "childhood granulomatous periorificial dermatitis" as the most suitable term for this condition till a better name is given.
Our case demonstrated extra-facial involvement, healing with atrophic pigmented scars, fast resolution with amoxicillin and clavulanic acid combination and coincidental association with JRA. Patient is under follow-up and no recurrence of lesions has been seen till date.
| 1. |
Urbatsch AJ, Frieden I, Willialms ML, Elevaski BE, Mancini AJ, Paller AS. Extarfacial and generalized granulomatous periorificial dermatitis. Arch Dermatol 2002;138:1354-8.
[Google Scholar]
|
| 2. |
Misago N, Nakafusa J, Narisawa Y. Childhood granulomatous periorificial dermatitis: Lupus miliaris disseminatus faciei in children? J Eur Acad Dermatol Venereol 2005;19:470-3.
[Google Scholar]
|
| 3. |
Gianotti F, Ermacora E, Benelli MG, Caputo R. Particuliere dermatite periorale infantile:obsernvations sur 5 cas. Bull Soc Fr Dermatol Syphiligr 1970;77:341.
[Google Scholar]
|
| 4. |
Cox ES, Shannon AB. Papular facial eruption in an African American adolescent-quiz case. Arch Dermatol 2006;142:775-80.
[Google Scholar]
|
| 5. |
Knautz MA, Lesher JL Jr. Childhood granulomatous periorificial dermatitis. Padiatr Dermatol 1996;13:131-4
[Google Scholar]
|
| 6. |
Marten RH, Prebury DG, Adamson JE, Cardell BS. An unusual papular and acneiform facial eruption in the Negro child. Br J Dermatol 1974;91:435-8.
[Google Scholar]
|
| 7. |
Williams HC, Ashworth J, Pembroke AC, Breathnach SM. FACE- Facial Afro-Caribbean childhood eruption. Clin Exp Dermatol 1990;15:163-6.
[Google Scholar]
|
| 8. |
Glass DA 2nd, Maender J, Metry D. Two pediatric cases of Blau syndrome. Dermatol Online J 2009;15:5.
[Google Scholar]
|
| 9. |
Kanwar AJ, De Dipankar. Systemic collagen disorders. In: Valia RG, Valia AR, Editors. IADVL Textbook of dermatology. 3 rd ed. Mumbai, India: Bhalani publishing house; 2008. p. 1220-66.
[Google Scholar]
|
Fulltext Views
3,247
PDF downloads
1,092





