Translate this page into:
Childhood pemphigus vulgaris successfully treated with rituximab
2 Department of Dermatology, Kurume University School of Medicine, and Kurume University Institute of Cutaneous Cell Biology, 67 Asahimachi, Kurume, Fukuoka 830-0011, Japan
Correspondence Address:
Amrinder J Kanwar
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh-160 012
India
| How to cite this article: Kanwar AJ, Sawatkar GU, Vinay K, Hashimoto T. Childhood pemphigus vulgaris successfully treated with rituximab. Indian J Dermatol Venereol Leprol 2012;78:632-634 |
Abstract
Pemphigus is a potentially fatal autoimmune epidermal bullous disorder. Rituximab is a novel therapy for the treatment of refractory pemphigus. However, there is limited clinical data on safety and efficacy of rituximab in pediatric age group. Herein, we report an 11-year-old boy of childhood pemphigus vulgaris who failed to respond to dexamethasone pulse therapy and was subsequently treated with rituximab and achieved complete remission.Introduction
Pemphigus is a relatively common autoimmune mucocutaneous blistering disorder in India and is caused by antibodies directed against desmosomal cadherins known as desmogleins (Dsg). The 2 main types of pemphigus are pemphigus vulgaris (PV) and pemphigus foliaceus (PF). In India, pemphigus occurs in a younger age group, commonly found in 3 rd and 4 th decades. In a study from north India, 75% of the patients were aged less than 45 years, and children aged less than 15 years accounted for 3.7% of cases. [1] PV in children aged less than 12 years is known as childhood PV and in those aged between 12-18 years as juvenile PV. [2] The disease course of childhood pemphigus and treatment modalities are essentially the same as those in adults. [3] Although corticosteroids are the mainstay of therapy, adjuvant immunosuppressive drugs are often needed to control the disease. Some childhood pemphigus patients are refractory to conventional treatments and require additional therapies.
Case Report
An 11-year-old boy presented with a 4-month-history of painful oral ulcers and flaccid fluid-filled blisters predominantly on the face and upper trunk, which ruptured to form progressive erosions with crusting. Tzanck smear from the floor of the vesicle showed acantholytic cells, and skin biopsy specimens showed suprabasal acantholysis with tomb stone appearance of basal keratinocytes. The results of direct and indirect immunofluorescence studies were consistent with a diagnosis of PV. The patient was started on dexamethasone pulse therapy (100 mg dexamethasone in 250 ml of 5% dextrose for 3 consecutive days every 28 days) with oral prednisolone 1 mg/kg/day and azathioprine 1.5 mg/ kg/day during the intervening period. There was partial improvement and cutaneous erosions healed, although new lesions continued to occur. Three weeks after receiving the 4 th course of dexamethasone pulse therapy, patient developed severe disease flare with extensive cutaneous erosions and new blisters [Figure - 1]a, and had an Ikeda severity score [4] (ISS) of 10. Blood cultures grew Klebsiella pneumoniae and Acinetobacter baumannii on two separate occasions, and he was treated with appropriate antibiotics. ELISA of recombinant Dsg baculoproteins for IgG antibodies at this point showed a Dsg1 index value of 102.77 and Dsg3 index value of 194.58 (cut-off value > 20). Because of persistent disease activity and failure of former therapies, it was decided to treat the patient with rituximab. Five weeks after the 4 th dexamethasone pulse, 2 courses of rituximab were administered at a dose of 375 mg/m 2 body surface area at 15 days interval. He also received prednisolone at a dose of 1 mg/kg/day, while all other therapies were stopped. The patient showed dramatic response. New lesions stopped to appear, and 80% of the lesions healed within 3 weeks and ISS was 3 [Figure - 1]b. Corticosteroids were rapidly tapered during the next 6 weeks. Dsg1 and Dsg3 ELISA index values detected 1 month after rituximab infusion were 109.76 and 124.37, respectively. He was in clinical remission for 8 months follow-up period, and all treatments stopped. ELISA tests could not be repeated as his parents refused the investigation.
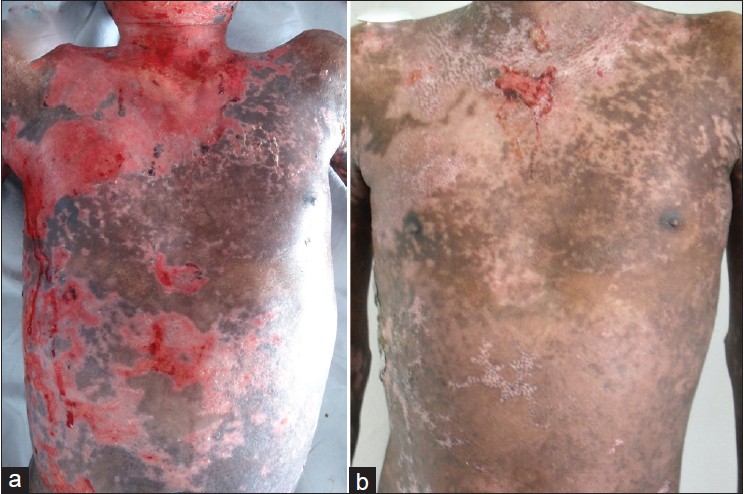 |
| Figure 1: Clinical features. (a) Prior to rituximab infusion, extensive erosions over the upper trunk were seen. (b) Three weeks after rituximab therapy, majority of the erosions healed |
Discussion
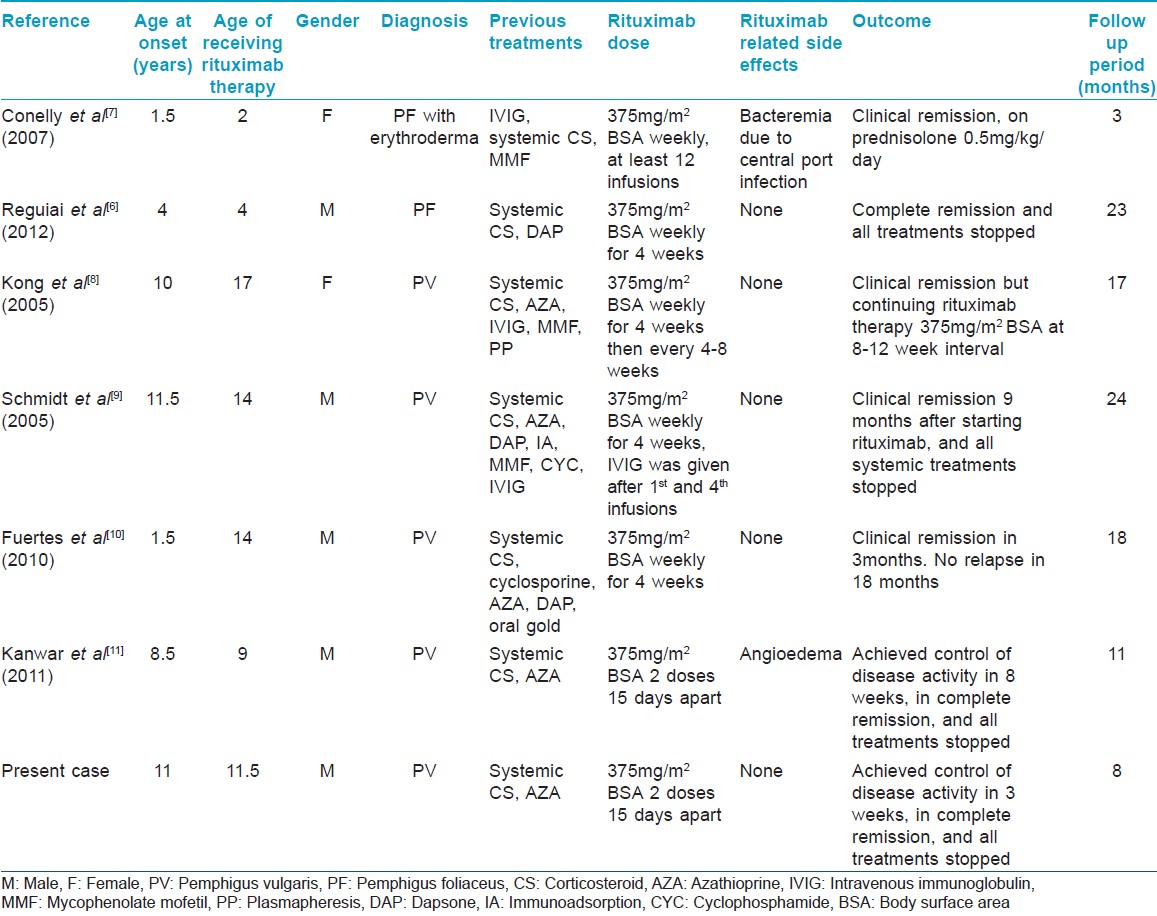
Rituximab, a chimeric anti-CD20 antibody, targets an integral membrane protein involved in B-cell activation and proliferation. Use of rituximab has been indicated in pemphigus patients who fail to respond to conventional treatment or when their use is contraindicated. [5] Recent studies have shown long term safety and efficacy of rituximab in pemphigus patients. [6] However, use of rituximab is not recommended in children, mainly because of limited clinical experience in this age group. [5] Our patient had severe flare of the disease and did not improve with the conventional treatment modalities. He also developed life-threatening sepsis because of the secondarily infected skin erosions. Therefore, balancing the potential benefit and risk of harm, it was decided to treat him with rituximab. On review of the literature, we came across only 6 cases of childhood pemphigus treated with rituximab [Table - 1]. [6],[7],[8],[9],[10],[11] Two of these cases were PF and 4 were PV. However, 3 of the 4 childhood PV cases actually received rituximab therapy in their adolescence, although diagnoses were made before the age of 12 years. All cases of childhood pemphigus were treated with conventional modalities before rituximab therapy. These cases were generally resistant to conventional treatments or had severe adverse effects with these therapies. Most of the cases were treated with multiple infusions of rituximab with or without IVIG. In contrast, our case achieved clinical remission after only 2 rituximab infusions. None of the 6 previous cases showed any serious long-term adverse effects, although acute infusion reactions and systemic infections were found in some cases. [7],[11]
In conclusion, rituximab can be a good alternative therapy in recalcitrant cases of childhood pemphigus. Long-term prospective studies of rituximab in childhood pemphigus with adequate sample size are required to determine its safety and efficacy.
| 1. |
Kanwar AJ, Ajith AC, Narang T. Pemphigus in North India. J Cutan Med Surg 2006;10:21-5.
[Google Scholar]
|
| 2. |
Gorsky M, Raviv M, Raviv E. Pemphigus vulgaris in adolescence. A case presentation and review of the literature. Oral Surg Oral Med Oral Pathol 1994;77:620-2.
[Google Scholar]
|
| 3. |
Kanwar AJ, Dhar S, Kaur S. Further experience with pemphigus in children. Pediatr Dermatol 1994;11:107-11.
[Google Scholar]
|
| 4. |
Ikeda S, Imamura S, Hashimoto I, Morioka S, Sakuma M, Ogawa H. History of the establishment and revision of diagnostic criteria, severity index and therapeutic guidelines for pemphigus in Japan. Arch Dermatol Res 2003;295 Suppl 1:S12-6.
[Google Scholar]
|
| 5. |
Hertl M, Zillikens D, Borradori L, Bruckner-Tuderman L, Burckhard H, Eming R, et al. Recommendations for the use of rituximab (anti-CD20 antibody) in the treatment of autoimmune bullous skin diseases. J Dtsch Dermatol Ges 2008;6:366-73.
[Google Scholar]
|
| 6. |
Reguiai Z, Tabary T, Maizieres M, Bernard P. Rituximab treatment of severe pemphigus: Long-term results including immunologic follow-up. J Am Acad Dermatol Forthcoming 2012 Jan 18. doi: 10.1016/j.jaad.2011.12.019.
[Google Scholar]
|
| 7. |
Connelly EA, Aber C, Kleiner G, Nousari C, Charles C, Schachner LA. Generalized erythrodermic pemphigus foliaceus in a child and its successful response to rituximab treatment. Pediatr Dermatol 2007;24:172-6.
[Google Scholar]
|
| 8. |
Kong HH, Prose NS, Ware RE, Hall RP 3rd. Successful treatment of refractory childhood pemphgus vulgaris with anti-CD20 monoclonal antibody (rituximab). Pediatr Dermatol 2005;22:461-4.
[Google Scholar]
|
| 9. |
Schmidt E, Herzog S, Brocker EB, Zillikens D, Goebeler M. Long-standing remission of recalcitrant juvenile pemphigus vulgaris after adjuvant therapy with rituximab. Br J Dermatol 2005;153:449-51.
[Google Scholar]
|
| 10. |
Fuertes I, Guilabert A, Mascaro JM Jr., Iranzo P. Rituximab in childhood pemphigus vulgaris: A long-term follow-up case and review of the literature. Dermatology 2010;221:13-6.
[Google Scholar]
|
| 11. |
Kanwar AJ, Tsuruta D, Vinay K, Koga H, Ishii N, Dainichi T, et al. Efficacy and safety of rituximab treatment in Indian pemphigus patients. J Eur Acad Dermatol Venereol Forthcoming 2011. [In Press]
[Google Scholar]
|
Fulltext Views
4,927
PDF downloads
3,330





