Translate this page into:
Chromoblastomycosis in Nepal: A study of 13 cases
2 Department of Dermatology, Manipal College of Medical Science and Manipal Teaching Hospital, Pokhara, Nepal
Correspondence Address:
Seema V Pradhan
Department of Pathology, Manipal Teaching Hospital, Pokhara
Nepal
| How to cite this article: Pradhan SV, Talwar O P, Ghosh A, Swami RM, Shiva Raj K C, Gupta S. Chromoblastomycosis in Nepal: A study of 13 cases. Indian J Dermatol Venereol Leprol 2007;73:176-178 |
Abstract
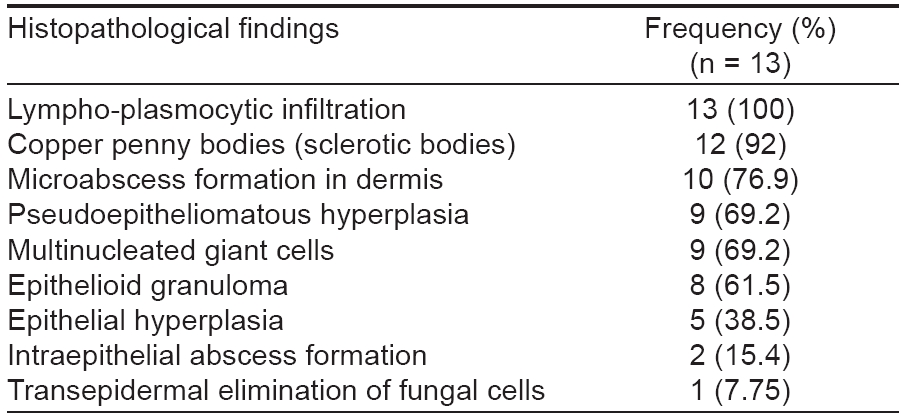
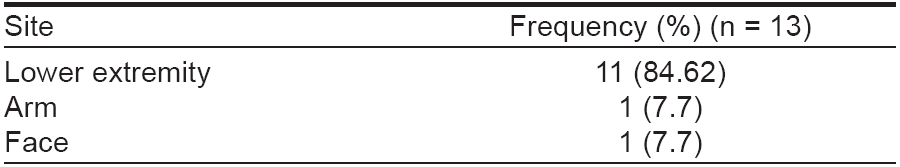
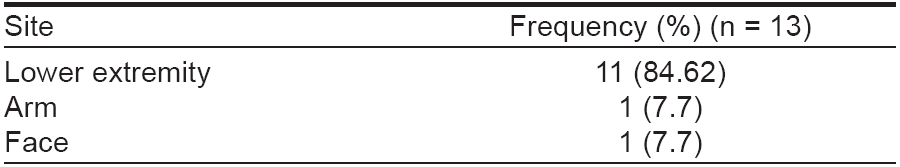
Background: Chromoblastomycosis is a chronic fungal infection caused by several pigmented fungi commonly seen in tropical and subtropical climates. Aim: To evaluate the epidemiologic, clinical and pathological characteristics of chromoblastomycosis in our patients. Methods: This retrospective and prospective study was conducted at the Manipal Teaching Hospital, Pokhara, Nepal. Clinical features and histopathology of all the cases diagnosed as chromoblastomycosis during the last eight years were studied. Results: A total of 13 cases of chromoblastomycosis were diagnosed during the period of 1999 - 2006. The disease was seen predominantly in middle-aged male farmers and those from rural areas. The lesions commonly involved the lower extremity and were single or multiple in number. They clinically presented as verrucous or nodular growths. Out of these 13 cases, three were diagnosed clinically as squamous cell carcinoma and one as psoriasis. The histopathological features included sclerotic bodies in 12 cases (92%), microabscess formation in 10 cases (76.9%), pseudoepitheliomatous hyperplasia in nine cases (69.2%) and granuloma in eight cases (61.5%). Conclusion: Farming is the commonest occupation in patients with chromoblastomycosis. Early histological diagnosis helps in effective management of the condition.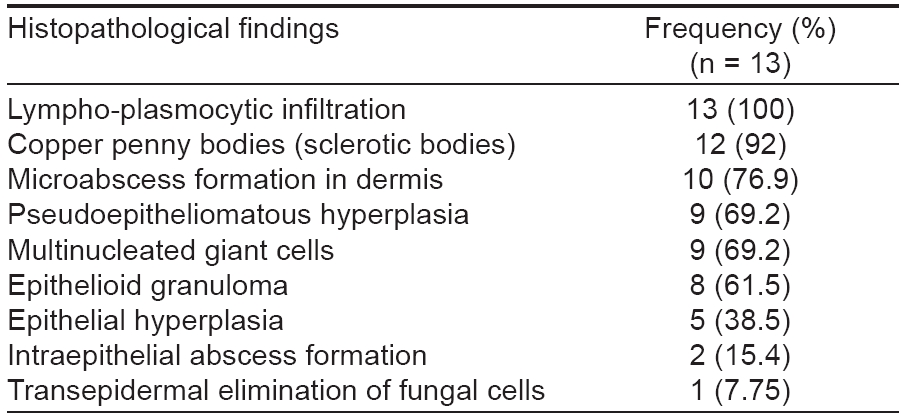
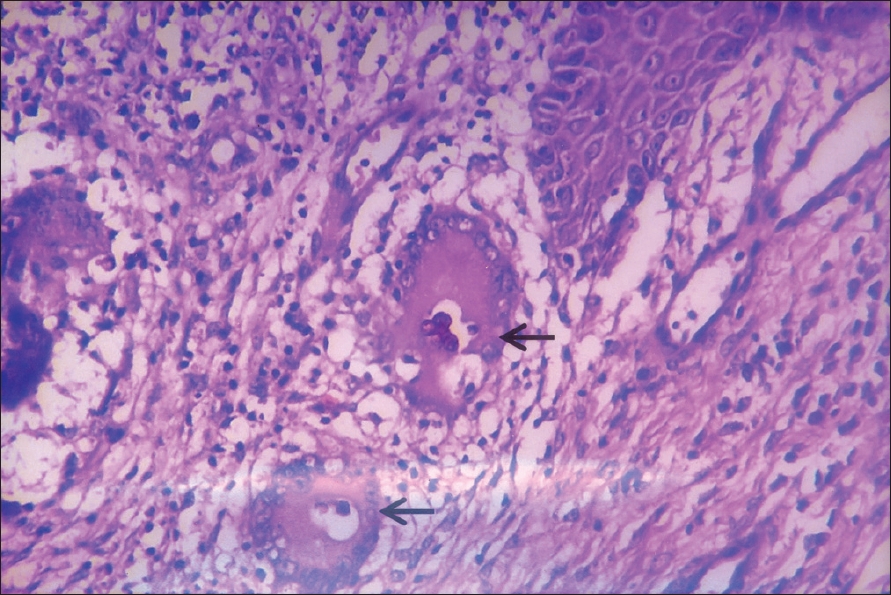 |
| Figure 3: Sclerotic bodies (arrow) within granuloma (H and E stain, x400) |
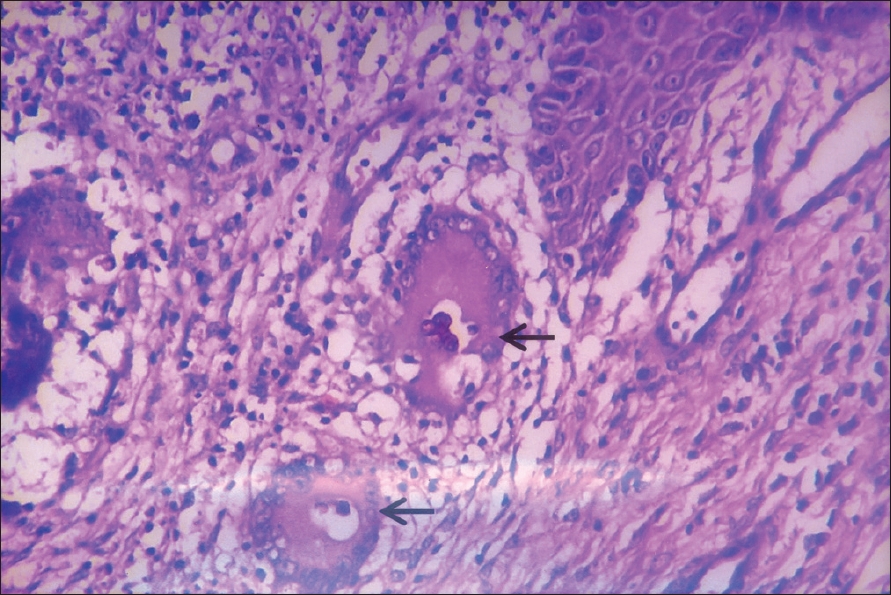 |
| Figure 3: Sclerotic bodies (arrow) within granuloma (H and E stain, x400) |
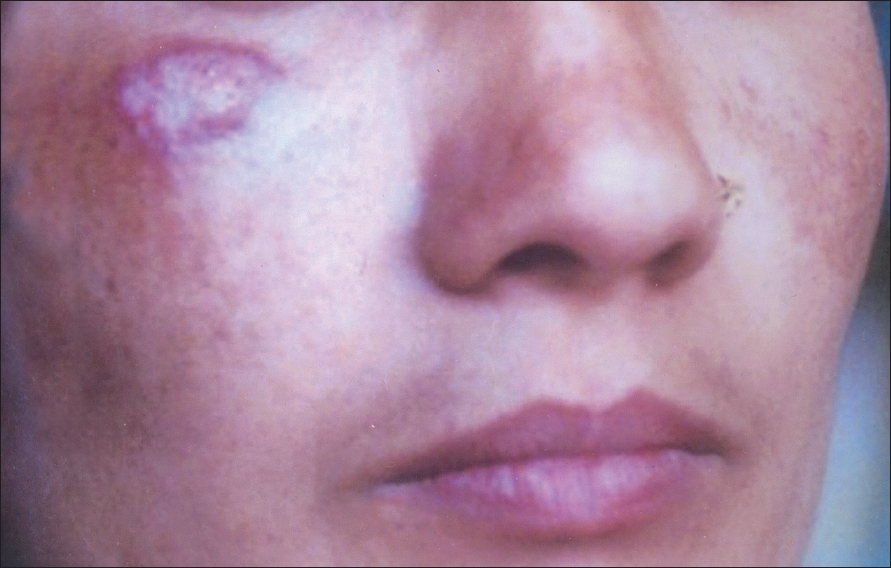 |
| Figure 2: Erythematous lesion on the face |
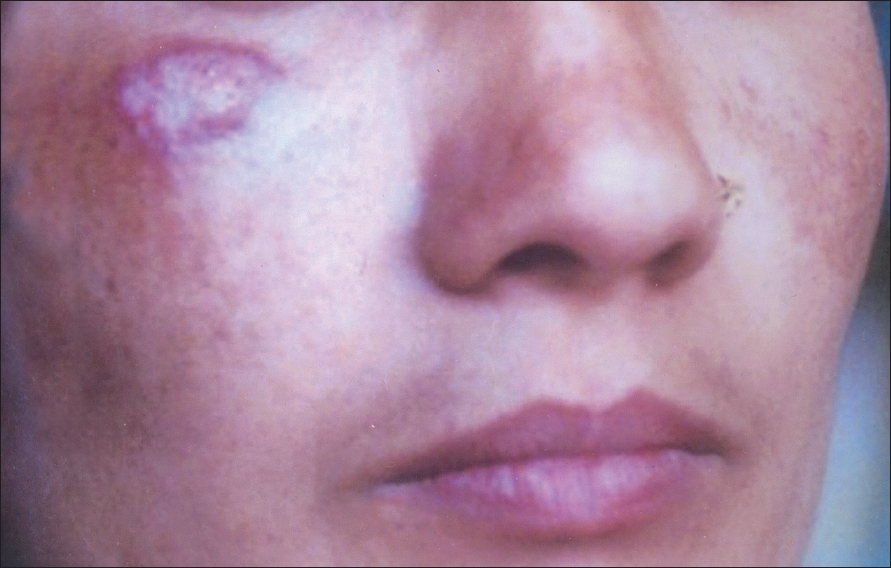 |
| Figure 2: Erythematous lesion on the face |
 |
| Figure 1: Erythematous plaque lesion with scaling on thigh |
 |
| Figure 1: Erythematous plaque lesion with scaling on thigh |
Introduction
Chromoblastomycosis is a chronic fungal infection of the skin and subcutaneous tissue, first described by Max Rudolph in 1914. The prevalence is higher in rural populations and in countries with a tropical or subtropical climate. The infection results from inoculation of fungi after penetrating cutaneous injury. It usually affects the lower and upper limbs. The lesion presents as a slow-growing, verrucous nodule. The prognosis of chromoblastomycosis is very good for small lesions. Severe cases are difficult to cure, although the prognosis is still quite good. [1],[2],[3]
The purpose of this article is to study the epidemiological, clinical and pathological characteristics of chromoblastomycosis in our patients.
Methods
This study included all the cases diagnosed as chromoblastomycosis during a period of eight years (1999-2006) in the Manipal Teaching Hospital, Pokhara, Nepal. Detailed history and examination were conducted to note clinical patterns of presentation and demographic parameters. The biopsy specimens were processed and stained with hematoxylin and eosin (H and E) stain. The data was summarized in tables.
Results
A total of 13 cases of chromoblastomycosis were diagnosed during the period of 8 years. The majority of the patients were males with male to female ratio of 1.6: 1. The ages ranged from 14-71 years, with a mean age of 41.9 years. Most of the patients belonged to the 21-40 years (5, 38.5%) and 41-60 years (5, 38.5%) age groups.
Out of the 13 cases seven were farmers, three housewives, two students and one laborer. However, all gave history of working in the fields. The duration of symptoms varied from three months to 35 years with a mean duration of 12.4 years.
The site of affection was lower extremity in the majority of cases (11, 84.62%, [Table - 1]). The lesion was limited to the foot in three cases (23.07%), affected the leg in six cases (46.15%) and in one case it affected the heel and the popliteal fossa. There was involvement of the arm and face in one case each. The majority of the lesions were single - 69% (n = 9) and the remaining had multiple lesions, involving the whole of the leg in four cases.
The clinical presentation was seen either as nodular lesion with verrucous surface in nine cases (69.35%) or as a plaque in the remaining four patients (30.65%). In one case each the plaque-like lesion was psoriasiform (erythematous and scaly) and cicatrizing (erythematous plaque with scarring) [Figure - 1]. The remaining two cases had plaques with verrucous surface resembling the nodules.
The salient histopathological features of these cases are summarized in [Table - 2]. Classical copper penny bodies with brown pigmentation (sclerotic bodies) were present in 12 cases [Figure - 2]. Only microabscesses and granuloma were seen in one case whose diagnosis was made on the basis of positive KOH mount for the fungus [Figure - 3].
Discussion
Chromoblastomycosis is a chronic localized infection of the skin and subcutaneous tissue. The disease takes its common name from the fact that most of the etiologic agents are dark-walled. The causative agents live in soil, woods and plant debris. [1-5] We studied the clinicopathological features of chromoblastomycosis in the western region of Nepal. Ordinarily, the infection occurs commonly in the age group of 20-40 years with male predominance. [1] However, in our series the infection was seen in a relatively older population with the mean age being 41.9 years, which may be partly explained by late presentation of the disease in our patients. Similar findings were noted in the study done by Minotto. [4]
Reports from other parts of Nepal, India, Sri Lanka and also from Central and South America show common involvement of the lower extremity as was the case with our study. [4],[6] This may be due to frequent trauma to the lower legs during agricultural work. Chromoblastomycosis rarely involves the face, but we had one female patient who presented with face affection. The lesions develop slowly following implantation at the site of trauma. Initially, it usually produces a warty nodule with or without ulceration. [1] The lesion may be flat sometimes but is commonly raised by 1-3 cm and is limited to the skin and the subcutaneous tissue. The lesion grows centripetally, sometimes with central healing leaving behind ivory-colored scars. Satellite lesions may develop following autoinoculation and by lymphatic spread to adjacent areas. [1],[3],[6]
The common clinical presentation in our study was as verrucous and nodular lesions. The clinical diagnosis was accurate in nine (69%) cases. One case was diagnosed clinically as psoriasis and three cases with verrucous lesions were diagnosed clinically as squamous cell carcinoma (SCC). In one case there was coexisting SCC with chromoblastomycosis. Round brown sclerotic bodies of varying sizes ranging from 5-10 µm in diameter are found in the vicinity of granuloma or inside the giant cells. [3],[7]
There are various reports stating about 40 reported cases from India since 1957. The majority were from the sub-Himalayan belt. The disease was more prevalent among males and also among farmers as seen in our cases. [8],[9],[10],[11],[12],[13] Two cases of chromoblastomycosis have been reported in Nepal, by Agarwalla et al , in the year 2002. Both were farmers with disease duration of more than 25 years. [6] However, we suspect that there are many more undiagnosed and unreported cases in different parts of Nepal.
The treatment for chromoblastomycosis is cryosurgery for small lesions; itraconazole for large ones; and in some cases, a combination of both. [14] All our patients were put on itraconazole and they responded well except for one case. Chromoblastomycosis evolves slowly and affects the quality of life. Moreover, there are reports of failure of medical treatment, recurrences and potential for SCC in affected regions. [11],[15] We recommend further studies to assess the extent of this problem in Nepal and evolve strategies for control of the infection.
| 1. |
Longley BJ. Fungal diseases. In : Elder D, Elenitsas R, Jaworsky C, Johnson B, editors. Lever's Histopathology of the skin. 8 th ed. New York: Lippincott-Raven publishers; 1997. p. 517-52.
th ed. New York: Lippincott-Raven publishers; 1997. p. 517-52. '>[Google Scholar]
|
| 2. |
Tang WK. Chromoblastomycosis. Hong Kong Dermatology and Venereology Bulletin 2002;10:76-9.
[Google Scholar]
|
| 3. |
Maize JC, Burgdorf WHC, Hurt MA, LeBoit PE, Metcalf JS, Smith T, et al . Chromomycosis, In : Cutaneous pathology. USA: Churchill Livingstone; 1998; p. 229-30.
[Google Scholar]
|
| 4. |
Minotto R. Chromoblastomycosis: A review of 100 cases in the state of Rio Grande do Sul, Brazil. J Am Acad Dermatol 2001;44:585-92.
[Google Scholar]
|
| 5. |
Bonifaz A, Carrasco E, Saul A. Chromoblastomycosis: Clinical and mycologic experience of 51 cases. Mycosis 2001;44:1-7.
[Google Scholar]
|
| 6. |
Agarwalla A, Khanal B, Garg VK, Agrawal S, Jacob M, Rani S et al . Chromoblastomycosis: Report of two cases from Nepal. J Dermatol 2002;29:315-9.
[Google Scholar]
|
| 7. |
Hamza SH, Mercado PJ, Skeleton HG, Smith KJ. An unusual dematiaceous fungal infection of the skin caused by Fonsecacea pedrosoi : A case report and review of literature. J Cutan Pathol 2003;30:340-3.
[Google Scholar]
|
| 8. |
Mohanty L, Mohanty P, Padhi T, Samantray S. Verrucous growth on leg. Indian J Dermatol Venereol Leprol 2006;72:399-400.
[Google Scholar]
|
| 9. |
Muhammed K, Nandakumar G, Asokan KK, Vimi P. Lymphangitic chromoblastomycosis. Indian J Dermatol Venereol Leprol 2006;72:443-5.
[Google Scholar]
|
| 10. |
Harshan V. Chromoblastomycosis due to Phialophora verrucosa . Indian J Dermatol Venereol Leprol 1994;60:95-6.
[Google Scholar]
|
| 11. |
Mary J, Rachel M, Prasad PVS, Bhaktaviziam A. Chromoblastomycosis with squamous cell carcinoma 1988;54:314-7.
[Google Scholar]
|
| 12. |
Sharma N, Sharma R, Grover P, Gupta M, Sharma A, Mahajan V. Chromoblastomycosis in India. Int J Dermatol 1999;38: 846-51.
[Google Scholar]
|
| 13. |
Kumar B. Chromoblastomycosis in India: two more cases. Int J Dermatol 2000;39:795-800.
[Google Scholar]
|
| 14. |
Poirriez J, Breuillard F, Francois N, Fruit J, Sendid B, Gross S, et al . A case of chromomycosis treated by a combination of cryotherapy, shaving, oral 5-fluorocytosine and oral amphotericin. Am J Trop Med Hyg 2000;63:61-3.
[Google Scholar]
|
| 15. |
Castro LG, Scwartz RA, Baran E. Chromoblastomycosis. Available from: http://www.emedicine.com/derm/topic855.htm/.Last updated: 2006 September 25.
[Google Scholar]
|
Fulltext Views
3,307
PDF downloads
2,863





