Translate this page into:
Chronic paronychia with subungual purpura
2 Department of Pathology, Christian Medical College, Vellore, Tamil Nadu, India
Correspondence Address:
Balakrishnan Nirmal
Department of Dermatology, Christian Medical College, Vellore,Tamil Nadu
India
| How to cite this article: Nirmal B, George R, Bindra MS. Chronic paronychia with subungual purpura. Indian J Dermatol Venereol Leprol 2020;86:463-465 |
A 24-year-old man was apparently well till 4 years ago, when he developed sudden onset of breathlessness and was diagnosed to have bilateral pneumothorax. Six months after the episode, he developed skin lesions which started as itchy red papules and pustules on the scalp, axilla and perianal region. The nails were involved 1 year after the skin lesions. The affection started as painful swelling of nail folds associated with nail destruction [Figure - 1]. The nail changes including plate thickening, distal splitting, elkonyxis, onycholysis and subungual hemorrhage, were confined to the finger nails sparing the toe nails. The patient also had history of recurrent painful oral erosions of 2 years duration with loss of the lower teeth. He also had intermittent watery discharge from both ears. There was elbow and knee pain of 6 months duration. There was no history suggestive of bowel disturbances, weight loss, eye complaints or diabetes insipidus.
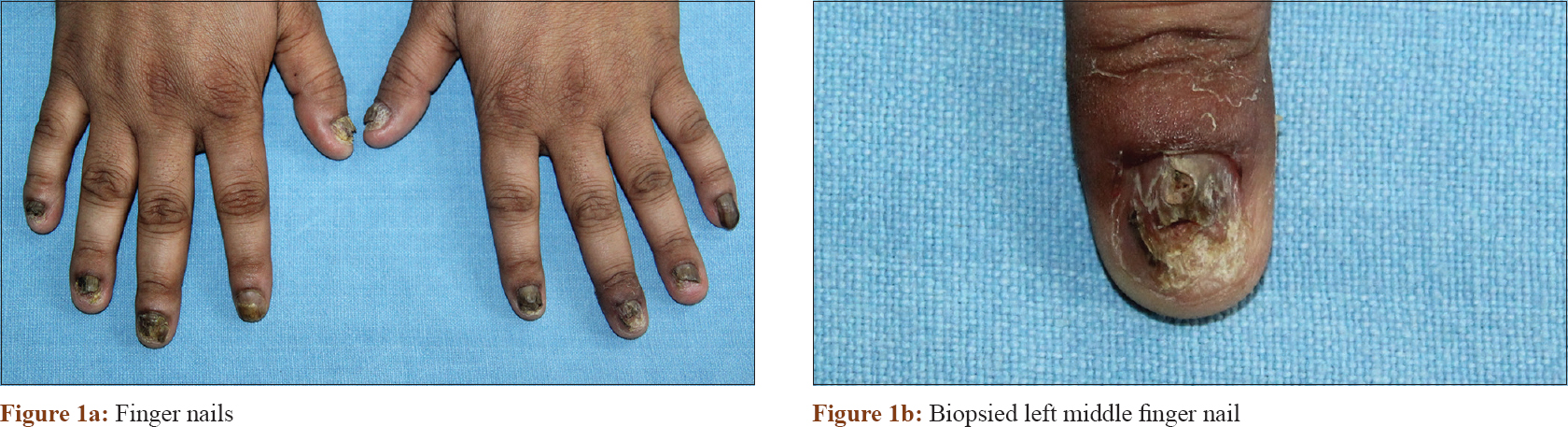 |
| Figure 1: |
Dermatoscopy was performed in all nail units using a handheld dermatoscope which gives a 10 × magnification (Dermlite DL3, 3Gen Inc., USA) in polarized mode using ultrasound gel as interface fluid and images were taken with a Sony Cybershot DSC-W800 20.1 MP digital camera. Subungual purpura [Figure - 2] was present only in the left middle finger along with the above nail findings. The left little finger showed nail plate thickening and elkonyxis. The rest of the nails showed subungual hemorrhages, onycholysis, distal splitting and longitudinal grooving [Figure - 3]. Nail matrix and nail bed biopsy was performed from the left middle finger nail unit which showed CD-1a positive clusters of large cells with indented reniform nuclei with eosinophilic cytoplasm along with lymphocytes and few plasma cells [Figure - 4].
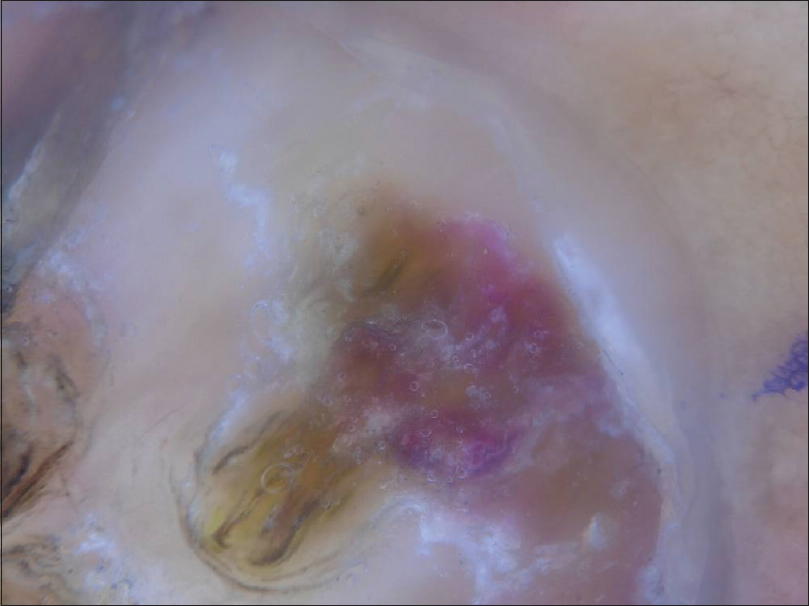 |
| Figure 2: Dermatoscopy of left middle finger nail unit showing subungual purpura (polarized, ×10) |
 |
| Figure 3: Dermatoscopy of nail unit showing onychodystrophy, nail plate discoloration and longitudinal ridging(polarized, ×10) |
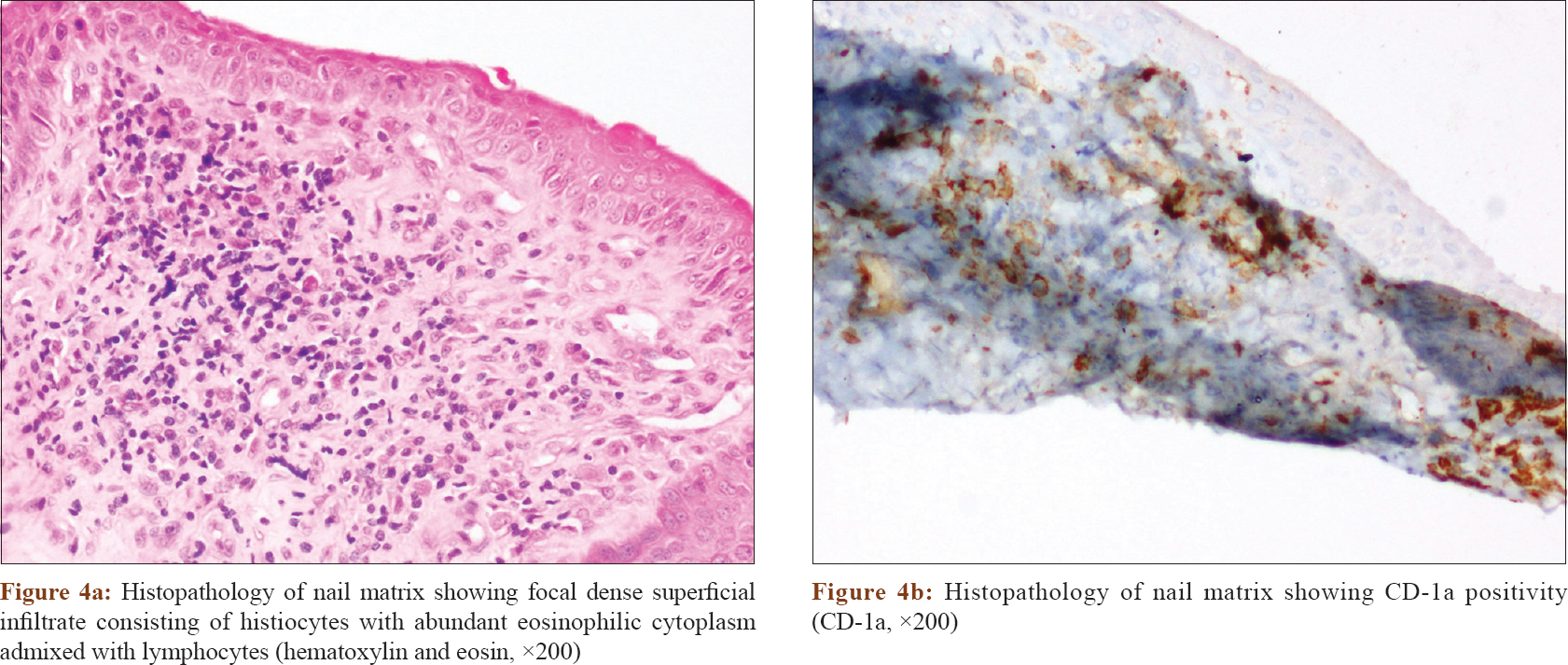 |
| Figure 4: |
What is Your Diagnosis?
Declaration of patient consentThe authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Alsina MM, Zamora E, Ferrando J, Mascaro J, Conget JI. Nail changes in histiocytosis X. Arch Dermatol 1991;127:1741.
[Google Scholar]
|
| 2. |
Mataix J, Betlloch I, Lucas-Costa A, Pérez-Crespo M, Moscardó-Guilleme C. Nail changes in Langerhans cell histiocytosis: A possible marker of multisystem disease. Pediatr Dermatol 2008;25:247-51.
[Google Scholar]
|
| 3. |
Holzberg M. The nail in systemic disease. In: Baran R, editor. Diseases of the Nails and their Management. 4th ed.. West Sussex: Wiley-Blackwell; 2012. p. 381-2.
[Google Scholar]
|
| 4. |
Figueras-Nart I, Vicente A, Sánchez-Schmidt J, Jou-Muñoz C, Bordas-Orpinell X, Celis-Passini VP,et al. Langerhans cell histiocytosis presenting as fingernail changes. JAAD Case Reports. 2016;2:485-7.
[Google Scholar]
|
Fulltext Views
3,691
PDF downloads
2,704






