Translate this page into:
Classic Kaposi sarcoma in Eastern India
Corresponding author: Dr. Ivoreen Darung, Senior Resident, Department of Dermatology, Venereology and Leprosy, Tomo Riba Institute of Health and Medical Sciences, Naharlagun, Arunachal Pradesh, India. ivoreendarung@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Darung I, Shah N, Ghosh A, Kamgo L, Kavishwar V. Classic Kaposi sarcoma in Eastern India. Indian J Dermatol Venereol Leprol doi: 10.25259/IJDVL_942_2021
Sir,
Kaposi Sarcoma is a multifocal low-grade vascular tumour caused by the human herpes virus-8. There are four types of Kaposi sarcoma: classic, African (endemic), iatrogenic and acquired immunodeficiency syndrome-associated Kaposi sarcoma.1 Classic Kaposi sarcoma is extremely rare in India.2 It is more prevalent in the Mediterranean and eastern European regions, predominantly in men between the fifth and seventh decade of life, presenting as indolent lesions predominantly in extremities.1
An 82-year-old immunocompetent heterosexual married man from the north-eastern region of India presented with swelling of the right leg with overlying multiple painless, reddish-brown raised lesions for two years. On examination, there were multiple non-tender discrete and coalescing reddish-brown to violaceous macules and papulonodules over the medial and posterior aspect of the right foot associated with ipsilateral non-pitting oedema [Figure 1]. A few reddish-brown macules and small papules were also present over the medial aspect of the left foot. General and systemic examination was normal. There was no lymphadenopathy. The mucosa was uninvolved. All routine laboratory and radiological investigations were normal. Hepatitis B, C and human immunodeficiency virus tests were negative.

- Multiple discrete and coalescing reddish-brown macules and papulonodules over medial aspect of right foot (non-healing ulcer at the site of incisional biopsy)
Clinically, differential diagnoses considered were angiosarcoma, acro-angiodermatitis and cutaneous B-cell lymphoma. Biopsy taken from one of the papules showed expansion of the dermis by the relatively circumscribed proliferation of bland spindle cells arranged in fascicles with multiple slit-like spaces and numerous extravasated erythrocytes [Figure 2]. Immunohistochemical staining was positive for CD34 [Figure 3a], CD31 and human herpes virus-8 [Figure 3b]. Based on the above findings, a diagnosis of classic Kaposi sarcoma was made and the patient was referred to the oncology department for further management.
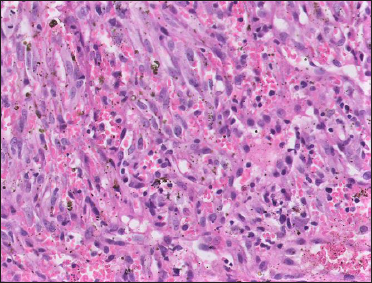
- Fascicles of relatively monomorphic spindled cells, with slit-like vascular channels containing erythrocytes (H & E, ×40)
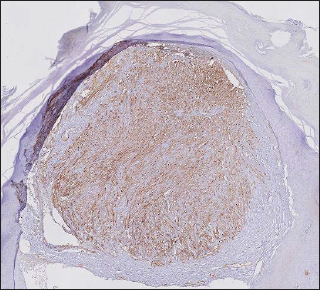
- Immunohistochemistry for CD34 (× 10) showing diffuse nuclear positivity
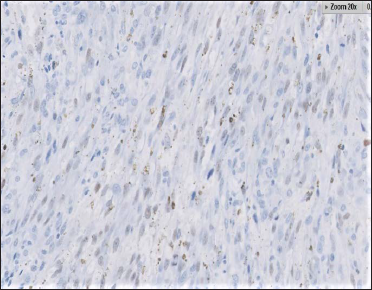
- Immunohistochemistry for human herpes virus-8: Nuclei of tumour cells showing immunoreactivity ( × 40)
Treatment of this disease depends on the clinical presentation, extent of involvement and associated comorbidities. In local diseases, radiation is widely used. Other options are photodynamic therapy, intralesional vinblastine, topical alitretinoin gel, cryotherapy, curettage and electrodesiccation. For extensive disease, a combination of surgery, chemotherapy (liposomal anthracyclines and taxanes) and radiation is advocated. Other treatment modalities such as interferon α, thalidomide, anti-herpes therapy, imatinib and matrix metalloproteinase inhibitors are also being tried.1,2 In our case, the patient did not return for follow-up. In angiosarcoma, lesions usually appear over the face and scalp, sites of irradiation and chronic lymphedema. Histopathology shows numerous vascular spaces lined by flattened endothelial cells with cellular atypia and intracytoplasmic vacuoles. Immunohistochemical staining is positive for CD31 and CD34 similar to Kaposi sarcoma.3 Acroangiodermatitis also known as pseudo-Kaposi sarcoma occurs due to chronic venous insufficiency and other vascular abnormalities. Immunohistochemical staining is negative for CD35.4
Classic Kaposi sarcoma is extremely rare in India and, till now, only less than 30 cases have been reported. The risk factors include reduced haemoglobin, reduction in the number of CD4 and CD8 lymphocytes and increased monocytes.5 Due to its rarity, the diagnosis of Kaposi sarcoma may be overlooked both clinically and histopathologically and a hence a very high degree of suspicion is required to undertake immunohistochemistry tests, considering the financial constraints of the majority of patients in our country.
Declaration of patient consent
Patient’s consent not required as patient's identity is not disclosed or compromised.
Conflict of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Kaposi sarcoma presenting as dermal nodule. BMJ Case Rep. 2011;2011 bcr0120113789
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated Kaposi’s sarcoma in a human immunodeficiency virus-infected homosexual Indian man. Indian J Dermatol Venereol Leprol. 2017;83:78-83.
- [CrossRef] [PubMed] [Google Scholar]
- Kaposi sarcoma and cutaneous angiosarcoma: Guidelines for diagnosis and treatment. Actas Dermosifiliogr. 2018;109:878-87.
- [CrossRef] [PubMed] [Google Scholar]
- Acroangiodermatitis (Pseudo-Kaposi sarcoma) Indian Dermatol Online J. 2014;5:323-5.
- [CrossRef] [PubMed] [Google Scholar]
- Classic Kaposi sarcoma from North-East India: A case report. IP Indian J Clin Exp Dermatol. 2020;6:291-3.
- [CrossRef] [Google Scholar]





