Translate this page into:
Clear cell anaplastic large cell lymphoma in a young male: A rare lymphoma variant
Corresponding author: Dr. Tarun Narang, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India. narangtarun@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Sharma A, Chatterjee D, Prakash G, Bansal P, Narang T. Clear cell anaplastic large cell lymphoma in a young male: A rare lymphoma variant. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_964_2024
Dear Editor,
Clear cell anaplastic large cell lymphoma (ALCL) stands as a rare entity within the spectrum of lymphomas.1,2 A 22-year-old, previously healthy male presented with a gradually enlarging, painless, firm, erythematous nodulo-plaque lesion overlying the right chest wall [Figure 1a]. The lesion progressively enlarged over the next two months, and there was an evening rise in temperature for one week (100–101°F) without systemic symptoms such as loss of weight or appetite. After initial clinical evaluation, a diagnosis of scrofuloderma or cutaneous lymphoma was suggested. The lesion became an exophytic ulcerated lesion of size 5 × 11 cm within the next month [Figure 1b]. There was no concomitant lymphadenopathy or organomegaly. The chest X-ray was normal, and the Mantoux test and the interferon-gamma release assay came out negative. Histopathological examination revealed epidermis with hyperkeratosis and spongiosis. The superficial dermis showed mild to moderate perivascular inflammation composed of lymphocytes, plasma cells, neutrophils, and histiocytes. Deeper dermis showed sheets of atypical large lymphoid cells with pleomorphic hyperchromatic nuclei, irregular nuclear membrane, and moderate to abundant clear cytoplasm Figures 2a and 2b. On immunohistochemistry (IHC), the atypical lymphoid cells were diffusely positive for CD30 and CD45 [Figures 2c and 2d] and negative for CD3 [Supplementary Figure 1a], CD20 [Supplementary Figure 1b], desmin, CD68, S-100, CK (creatine kinase), melan A, HMB-45 (hydroxymethyl butyrate) and ALK (anaplastic lymphoma kinase) [Supplementary Figure 1c]. A final diagnosis of ALCL (clear cell variant) was made [Figure 2a-c]. Positron emission tomography showed an intense FDG (fluorodeoxyglucose)-avid exophytic ulceroproliferative soft tissue lesion on the right upper anterior chest wall (4.8 × 8.3 × 11.0 cm, SUVmax 39) infiltrating the underlying pectoralis major and minor muscles. The patient was subsequently started on a CHOEP (cyclophosphamide, doxorubicin, vincristine, etoposide, and prednisone) regimen,3 which led to significant improvement within a month [Supplementary Figure 1d]. The patient was subsequently followed up in the department of medical oncology and is currently doing well.

- Erythematous nodulo-plaque lesion overlying the right chest wall.

- Rapidly increase in size within a span of the next one month to become an exophytic ulcerated lesion.
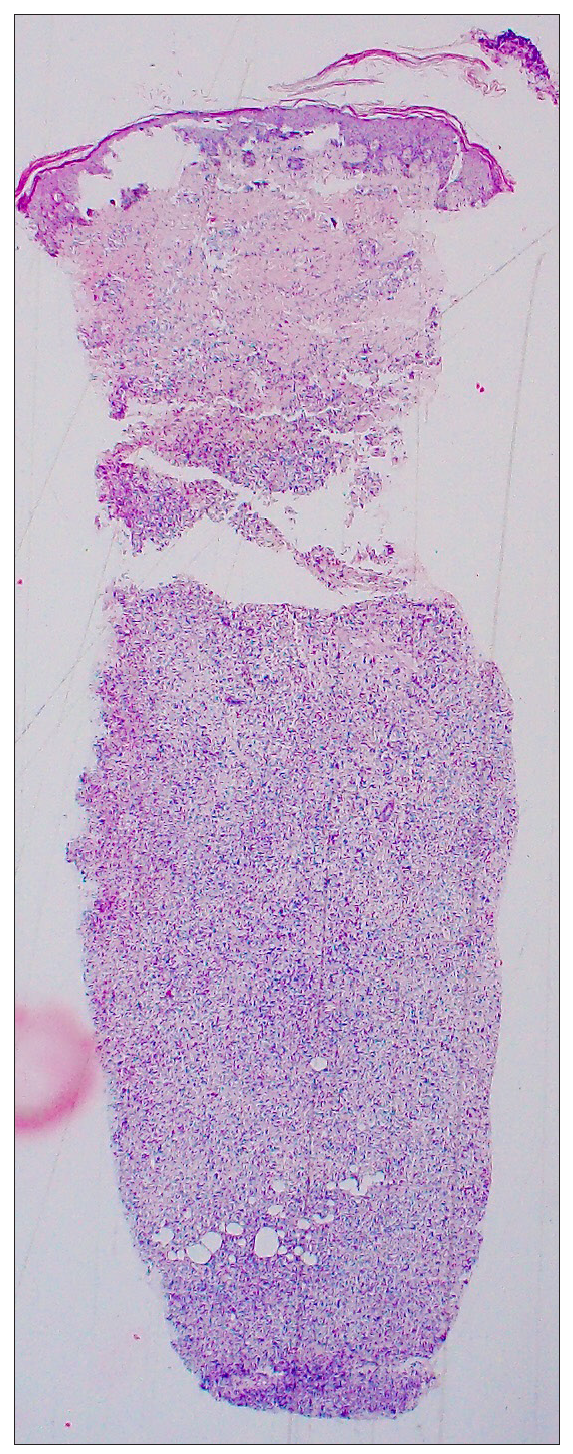
- The epidermis showed hyperkeratosis and spongiosis. The superficial dermis showed mild to moderate perivascular inflammation composed of lymphocytes, plasma cells, neutrophils, and histiocytes. The deeper dermis showed sheets of atypical large lymphoid cells (Haematoxylin and eosin, 40x).
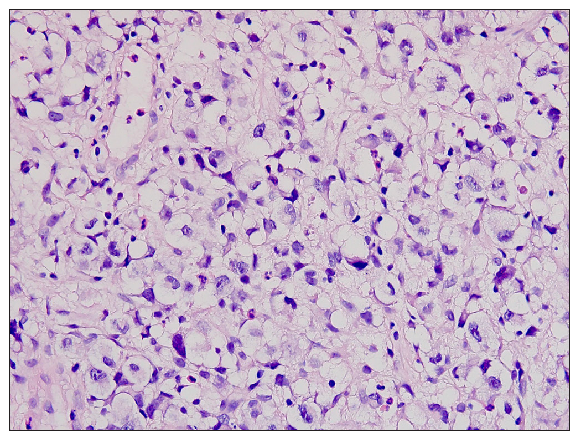
- On higher magnification, these cells were seen to have pleomorphic hyperchromatic nuclei with irregular nuclear membrane and moderate to abundant clear cytoplasm. Overall features were suggestive of anaplastic large cell lymphoma (clear cell variant) (Haematoxylin and eosin, 200x).
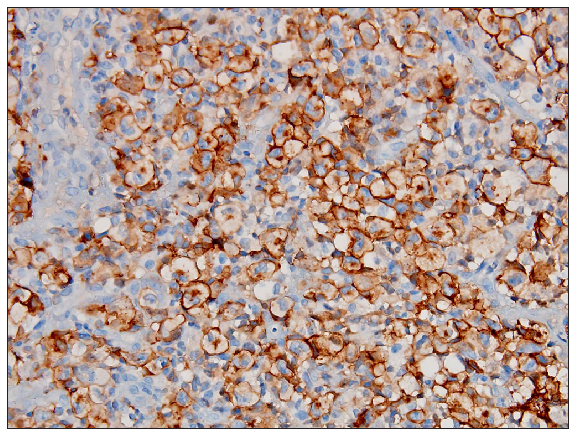
- Atypical lymphoid cells were diffusely positive for CD30 (membranous with golgi zone accentuation) (200x).
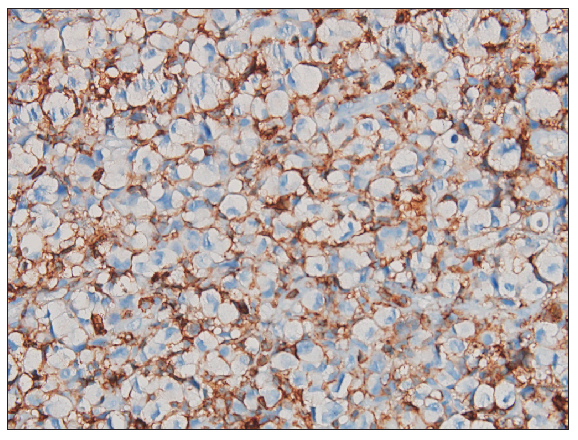
- On immunohistochemistry, the atypical lymphoid cells were diffusely positive for CD45 (200x).
Clear cell ALCL is a rare subtype of ALCL, predominantly affecting young adults.
Primary cutaneous ALCL is generally ALK-negative while systemic ALCL can be positive or negative for ALK. Aberrations in the ALK gene have been implicated in a subset of ALCL cases. The detection of ALK expression through IHC serves as a diagnostic marker and a potential therapeutic target, as ALK inhibitors like crizotinib have shown efficacy in ALK-positive ALCL. Targeted therapy options are limited in ALK-negative cases, and subtyping of ALK-negative ALCL based on DUSP22 rearrangement and p63 expression provides prognostic information.4 The inflammatory background in ALCL can occur in ulcerated lesions. A subset of DLBCL exhibiting CD30 positivity is an additional entity to consider. Histopathological differentials to be considered have been summarised in Table 1. While CD30-positive DLBCL often have a centroblastic appearance, they can occasionally have an anaplastic shape; the detection of ALK-negative and B-cell marker positivity (CD20, CD79) in the neoplastic cells is essential.5 The management of ALK-negative ALCL necessitates a multidisciplinary approach, which may involve surgical excision, systemic chemotherapy, and radiation therapy.
| CD30-positive peripheral T-cell lymphoma not otherwise specified (PTCL-NOS) | PTCL-NOS exhibits distinct characteristics from ALK-negative ALCL, including a more varied cytology, a more varied and typically lower expression of CD30, and a higher frequency of positive for CD2 and CD3. |
| Classic Hodgkin’s lymphoma | Rich in Reed Sternberg (RS) cells with less mixed inflammatory background, and PAX5 expression is a helpful tool for this differential diagnosis. |
| Others |
Clear cell porocarcinoma, Clear cell sarcoma, Balloon cell melanoma and Clear cell squamous cell carcinoma. |
ALK: Anaplastic lymphoma kinase; ALCL: Anapastic large cell lymphoma
Through meticulous histopathological evaluation and comprehensive molecular profiling for ALK-negative CCALCL, accurate diagnosis, and tailored therapeutic strategies can be formulated, optimising patient outcomes in managing this rare lymphoma variant.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Primary cutaneous anaplastic large cell lymphoma. J Cutan Pathol. 2017;44:570-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clear cell primary cutaneous anaplastic large cell lymphoma. Am J Dermatopathol. 2019;41:e111-5.
- [CrossRef] [PubMed] [Google Scholar]
- ALK-negative anaplastic large cell lymphoma: Features and outcomes of 235 patients from the International T-Cell Project. Blood Adv.. 2021;5:640-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- ALK-negative anaplastic large cell lymphoma (ALCL): Prognostic implications of molecular subtyping and JAK-STAT pathway. Appl Immunohistochem Mol Morphol. 2021;29:648-56.
- [CrossRef] [PubMed] [Google Scholar]
- ALK-positive anaplastic large cell lymphoma mimicking nodular sclerosis Hodgkin’s lymphoma: Report of 10 cases. Am J Surg Pathol.. 2006;30:223-9.
- [CrossRef] [PubMed] [Google Scholar]






