Translate this page into:
Clinical and immunological predictors of chronicity in erythema nodosum
Corresponding author: Dr. Sakir Ahmed, Department of Clinical Immunology and Rheumatology, Kalinga Institute of Medical Sciences, Bhubaneswar, India. sakir005@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jain K, Pradhan P, Kar HK, Behera D, Sukhija R, Bajoria S, et al. Clinical and immunological predictors of chronicity in erythema nodosum. Indian J Dermatol Venereol Leprol. 2025;91:S1-S7. doi: 10.25259/IJDVL_1626_2024
Abstract
Background
Erythema nodosum (EN) is a painful inflammatory disorder of the subcutaneous fat and the most common type of septal panniculitis. It often presents as erythematous, tender subcutaneous nodules, typically affecting the shins. EN is frequently a hypersensitivity reaction that can serve as a warning sign for an underlying systemic disorder, making it crucial to identify the cause. Though self-limiting in many cases, EN can sometimes become chronic, leading to significant discomfort. The pathogenesis of EN and the predictors of chronicity remain unclear, necessitating further investigation.
Aims
This study aimed to evaluate the various etiologies of EN and determine the clinical, laboratory, and immunohistochemical predictors of chronicity.
Methods
We conducted a prospective hospital-based study between July 2022 and June 2024 at a tertiary care centre in Eastern India. Clinical and histopathologically confirmed cases of EN presenting within 2-3 days of onset, without prior treatment, were enrolled. A detailed clinical examination and laboratory investigations were performed during the initial visit, including immunohistochemical analysis of skin biopsies. The total number of T cells (CD3+), helper T cells (CD4+), cytotoxic T cells (CD8+), CD4:CD8 ratio, and NK (natural killer) cells (CD56+) were quantified per skin biopsy specimen using a standardised technique. Patients were treated at the discretion of the treating physician. Patients were monitored monthly for three months and categorised as either having “Classic EN” (lesions resolving within three months) or “Chronic EN” (lesions persisting beyond three months). Data collected at the initial visit were correlated between the two groups to identify potential predictors of chronicity.
Results
Out of 63 suspected cases, EN was confirmed in 41 patients, who were predominantly females (65.85%), with a median age of 49 years (Q1 - Q3: 32 - 57). Pulmonary tuberculosis was the most frequent underlying condition (n = 15, 36.59%), followed by sarcoidosis (n = 8, 19.51%) and rheumatoid arthritis (n = 6, 14.63%). Chronic EN was observed in 36.59% of cases, with significantly elevated baseline C-reactive protein (CRP) levels (p = 0.003) and Mantoux test readings (p = 0.002). Immunohistochemistry revealed higher CD3, CD4, CD8, and CD56 levels in chronic EN cases (p < 0.05).
Limitations
The study’s limitations include a small sample size and short follow-up duration. Multivariable analysis could not be performed due to the small sample size.
Conclusion
This study identified clinical and immunohistochemical markers associated with the chronicity of EN and highlighted pulmonary tuberculosis as the most common underlying cause. Elevated CRP levels, positive Mantoux test results, and increased expression of CD3, CD4, CD8, and CD56 observed at baseline were linked to chronicity. The findings suggest the predominant role of T helper 1 (Th1) cell response and innate immunity in the pathogenesis of chronic EN lesions. Understanding these predictors and underlying aetiologies can help clinicians identify high-risk patients and tailor management accordingly.
Keywords
Erythema nodosum
aetiology
chronicity
predictors
immunohistochemistry
Introduction
Erythema nodosum (EN) is a painful skin disorder of the subcutaneous fat and the most common type of septal panniculitis. It manifests with acute onset tender, erythematous, subcutaneous nodules, typically affecting the pretibial regions and generally heal without ulceration, scarring, or atrophy.1
EN is generally considered a hypersensitivity reaction, often serving as an important warning sign for underlying systemic disease, making it crucial to identify the aetiology.2 EN can be associated with a wide range of conditions, including infections, medications, autoimmune diseases, malignancy, and even pregnancy.
Despite its common prevalence, the exact pathogenesis of EN remains unclear. The presence of circulating immune complexes in early lesions suggests a type III hypersensitivity reaction, yet cases lacking these complexes propose a type IV delayed hypersensitivity mechanism. This dual possibility reflects the complex immunological underpinnings of the disease.3
The clinical course of EN can vary significantly. Some cases resolve spontaneously or with minimal treatment, while others persist and evolve into chronic or recurrent disease, resulting in persistent discomfort and skin discolouration.4 A recent analysis by Shah et al. indicated that approximately 50% of EN patients experience chronic or recurrent episodes.5 The rising incidence of chronic EN has increased morbidity, making it essential to identify the predictors of chronicity and tailor treatment strategies to improve patient outcomes.
This study aimed to evaluate the clinical and immunohistochemical markers associated with chronic EN and investigate the underlying etiologies.
Methods
This hospital-based prospective study was conducted from July 2022 to June 2024 in dermatology, rheumatology, and pathology departments at a tertiary care centre in eastern India. Histopathologically confirmed cases of EN presenting within 2-3 days of onset, without prior treatment, were included after obtaining informed consent. The research protocol was reviewed by the Institutional Review Board (IRB) and approved by the ethics committee (Ref. No.: KIIT/KIMS/IEC/934/2022).
A detailed general and systemic examination was conducted for all participants. Skin lesions were examined for their morphology, distribution, tenderness, induration, and any signs of ulceration.
Routine laboratory investigations included a complete blood count, renal function test, liver function test, CRP, urine and stool microscopy/culture, fasting/postprandial blood sugar and thyroid-stimulating hormone levels. In addition, specialised tests were performed to identify potential underlying systemic causes. These included the Mantoux test, rheumatoid factor level, chest radiograph, ultrasound, anti-double-stranded DNA, anti-nuclear antibody profile, slit skin smear for acid-fast bacillus, anti-streptolysin O titre, angiotensin-converting enzyme levels, serum calcium levels, and screening for HIV, Hepatitis B and C.
Based on the clinical and laboratory findings, a diagnosis was established for each patient.
A deep skin biopsy from one of the nodules was sent from all patients for histopathological examination and immunohistochemistry. The pathologist examined the prepared slides under a light microscope at 10x and 40x magnifications. The observations were documented, and histopathologically confirmed cases of EN underwent further immunohistochemical analysis. Immunohistochemical staining was performed using ready-to-use, prediluted antibodies for the following markers- CD3 (Pan T cells, Clone: QR004); CD4 (Helper T cells, Clone: QR032); CD8 (Cytotoxic T cells, Clone: QR068); CD56 (Natural Killer cells, Clone: QR044). All antibodies were prediluted in TRIS buffer (pH 7.4) with <0.1% sodium azide, and no additional dilution was required.
The counts were done at sites with the highest concentration of cells, taking 5 different high-power fields (40x). The mean was calculated and represented as mean count/ High power field (HPF)/biopsy using a standardised protocol.6,7
Patients were treated at the physician’s discretion, following a basic protocol. Rest and non-steroidal anti-inflammatory drugs (NSAIDs) served as first-line treatment for all cases. Anti-tubercular therapy (ATT) was initiated for confirmed tuberculosis cases, while antimicrobial treatment was provided for infective etiologies. Immunosuppressants were prescribed based on the underlying aetiology, including prednisolone and steroid-sparing drugs such as methotrexate, colchicine, hydroxychloroquine, azathioprine, or dapsone.
Patients were monitored monthly for three months and categorised based on their follow-up outcomes as either “Classic EN” for cases that experienced resolution of lesions within three months or “Chronic EN” for cases developing new lesions and requiring treatment beyond three months.
The clinical, laboratory, and immunohistochemistry data collected during the initial visit were subsequently correlated between the two groups to identify potential predictors.
The collected data was analysed using STATA version 15.1. Due to the non-normal distribution of the data, Spearman’s correlation test and the Mann-Whitney U test were employed for comparison. Frequencies, medians, and interquartile ranges were tabulated and examined. A p-value of less than 0.05 was considered statistically significant.
Results
Among the 63 patients clinically suspected of having EN, biopsy results confirmed the diagnosis in 41 patients [Figure 1].

- Section shows septolobular panniculitis without evidence of vasculitis, consistent with EN. (Haematoxylin & eosin, 10x).
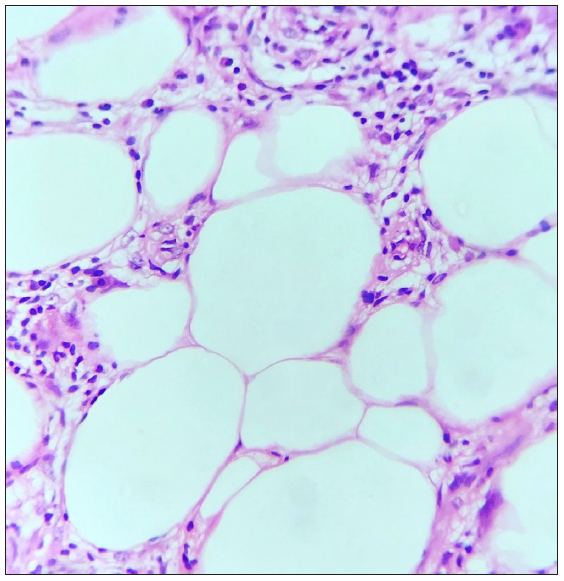
- Section shows dense lymphocytic septolobular panniculitis, consistent with EN. (Haematoxylin & eosin, 40x).
Study population
The cohort predominantly consisted of females (n=27, 65.85%) with a median age of 49 years (Q1 – Q3: 32 - 57).
Aetiology
The most frequent underlying condition associated with EN was pulmonary tuberculosis (PTB), accounting for 36.59% (n = 15) of cases, followed by sarcoidosis (19.51%, n = 8) and rheumatoid arthritis (14.63%, n = 6) [Figure 2]. Other causes included post-streptococcal infections (7.30%, n = 3), systemic lupus erythematosus (9.80%, n = 4), and behcet’s disease (4.90%, n = 2). A small proportion of cases remained idiopathic (7.30%, n = 3).

- Chronic EN with multiple subcutaneous nodules on the flexural aspects of the forearms in a case of rheumatoid arthritis, with characteristic hand deformities.

- Follow-up image showing only partial resolution of lesions despite 3 months of treatment.
Clinical presentation
The typical presentation of EN, characterised by erythematous, subcutaneous nodules primarily located on the shins, was observed in 82.93% (n = 34) of cases [Figure 3]. In contrast, 17.07% (n = 7) of cases presented with nodules located on the face or upper limbs, classified as atypical EN [Figure 4].
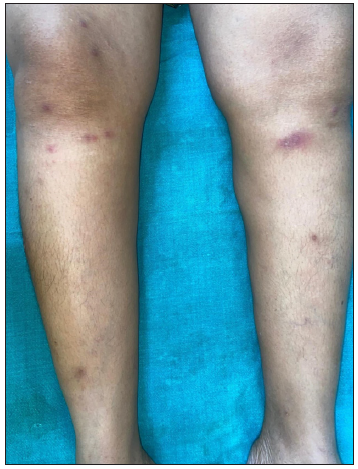
- Classic EN with erythematous, tender subcutaneous nodules on bilateral shins.

- Atypical EN with erythematous subcutaneous nodule on the face.

- Atypical EN with erythematous subcutaneous nodule on the right upper limb.
Of the total 41 cases, 63.41% (n = 26) resolved within 4-6 weeks of treatment (classic EN), while 36.59% (n = 15) persisted and required treatment beyond three months (chronic EN) [Figure 5].
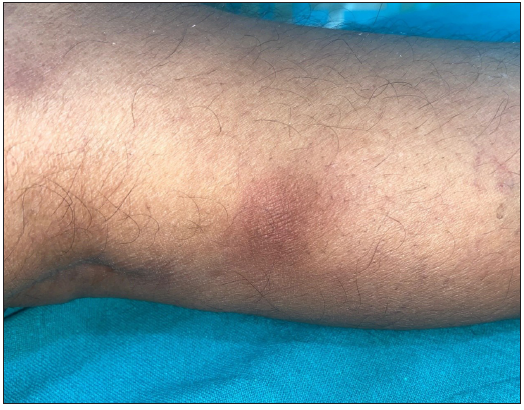
- Chronic EN lesion over the lateral aspect of right leg.
Clinical predictors of chronicity
Both classic EN and chronic EN groups exhibited similar age distributions and a higher proportion of females [Table 1]. Notably, only one case of chronic EN presented with atypical lesions; the remaining cases displayed typical lesions (p = 0.232). PTB was the leading cause in both classic (n = 10) and chronic (n = 5) EN. Remarkably, all three idiopathic EN cases progressed to chronicity (p = 0.217) [Table 2].
| Variable | Classic EN | Chronic EN | Mann Whitney U | Spearman’s Rho | ||
|---|---|---|---|---|---|---|
| (n=26) | (n=15) | p-value | Corr. Coef. | |||
| Median | Q1 - Q3 | Median | Q1 - Q3 | |||
| Age | 48 | 35 - 56 | 51 | 30 - 58 | 0.583 | 0.088 |
Tests are adjusted for pairwise comparison using the Benjamini-Hochberg correction.
| Variable | Classic EN | Chronic EN | p-value | Chi- Square/ Fisher’s Exact Test | |
|---|---|---|---|---|---|
| (n=26) | (n=15) | ||||
| Sex | Female | 15 | 12 | 0.186 | 2.105 |
| Male | 11 | 3 | |||
| Clinical features | Atypical EN | 6 | 1 | 0.232 | 1.806 |
| Typical EN | 20 | 14 | |||
| Clinical diagnosis | Behcets Disease | 1 | 1 | 0.217 | 7.724 |
| Idiopathic | 0 | 3 | |||
| PTB | 10 | 5 | |||
| Post streptococcal inf. | 3 | 0 | |||
| RA | 5 | 1 | |||
| SLE | 2 | 2 | |||
| Sarcoidosis | 5 | 3 | |||
Tests are adjusted for all pairwise comparisons using the Benjamini-Hochberg correction, RA: Rheumatoid arthritis.
Laboratory predictors of chronicity
Laboratory markers revealed significantly elevated baseline CRP levels (p-value = 0.003) and Mantoux test readings (p-value = 0.002) in the chronic group, with a positive correlation for both CRP levels (Spearman’s Rho = 0.450) and Mantoux test readings (Spearman’s Rho = 0.740) with chronicity [Table 3].
| Variable | Classic EN | Chronic EN | Mann Whitney U | Spearman’s Rho | ||
|---|---|---|---|---|---|---|
| (n=26) | (n=15) | p-value | Corr. Coef. | |||
| Median | Q1 - Q3 | Median | Q1 - Q3 | |||
| CRP (mg/L) | 25 | 15 - 30 | 35 | 30 - 95 | 0.003* | 0.450* |
| Mantoux Test (mm) | 14 | 13 - 15 | 22 | 17 - 22 | 0.002* | 0.740* |
Tests are adjusted for all pairwise comparisons using the Benjamini-Hochberg correction, Bold signifies that these values are statistically significant.
Immunological predictors of chronicity
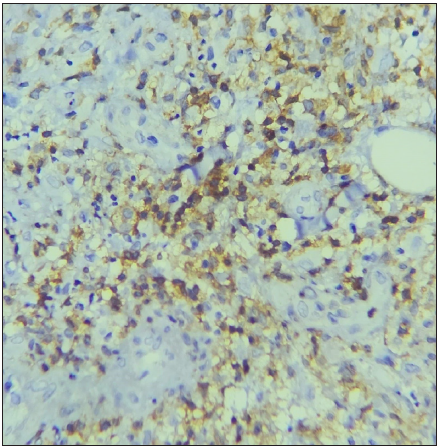
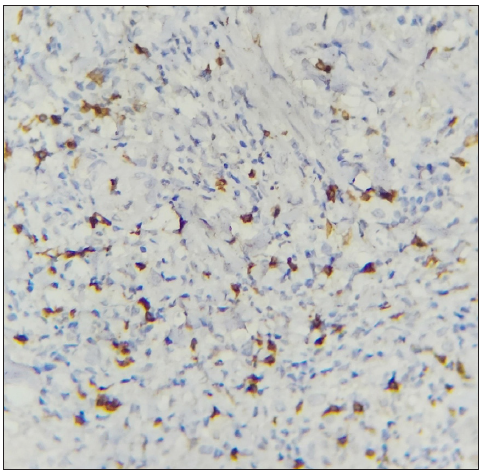
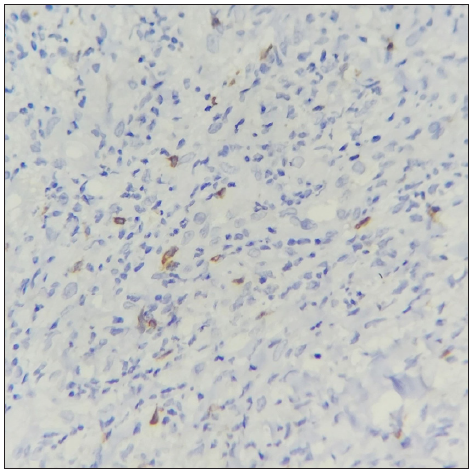
Immunohistochemical analysis demonstrated significantly higher levels of CD3, CD4, CD8, and CD56 at the biopsy site in chronic cases compared to classic EN cases (p-value <0.05), with positive correlation observed for all markers. The CD4:CD8 ratio showed no significant difference between the two groups (p-value = 0.784, Spearman’s Rho = 0.051) [Table 4; Figures 6 and 7].
| Variable | Classic EN | Chronic EN | Mann Whitney U | Spearman’s Rho | ||
|---|---|---|---|---|---|---|
| (n=26) | (n=15) | p-value | Corr. Coef. | |||
| Median | Q1 - Q3 | Median | Q1 - Q3 | |||
| CD3 | 36.2 | 22.6 - 52.4 | 52.4 | 38.6 - 58.4 | 0.025* | 0.387* |
| CD4 | 22.6 | 19.2 - 29.4 | 39.2 | 33 - 46.4 | 0.001* | 0.574* |
| CD8 | 17.8 | 12 - 29.6 | 25.4 | 23 - 29.8 | 0.033* | 0.368* |
| CD4:CD8 | 1.23 | 0.77 - 2.18 | 1.38 | 1.18 - 1.77 | 0.784 | 0.051 |
| CD56 | 0 | 0 - 0.4 | 3.4 | 0 - 6.7 | 0.001* | 0.589* |
Tests are adjusted for all pairwise comparisons using the Benjamini-Hochberg correction, Bold signifies that these values are statistically significant.
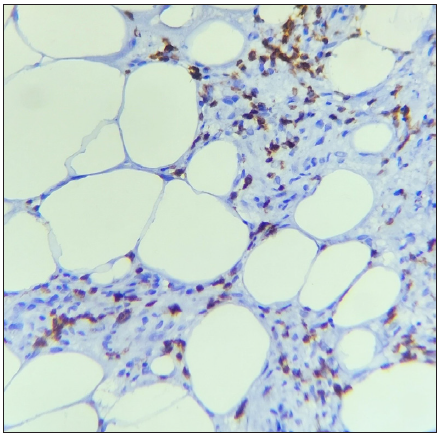
- The section shows scattered CD3+ T cells. (IHC with DAB staining: 40x, Classic EN).
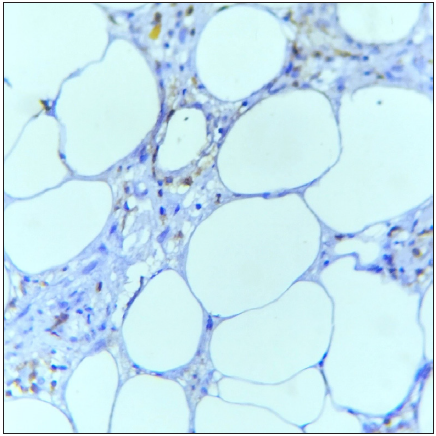
- The section shows few CD4+ T cells. (IHC with DAB staining: 40x, Classic EN).
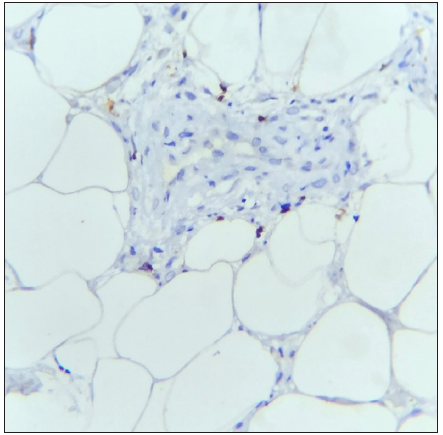
- The section shows few CD8+ T cells. (IHC with DAB staining: 40x, Classic EN).
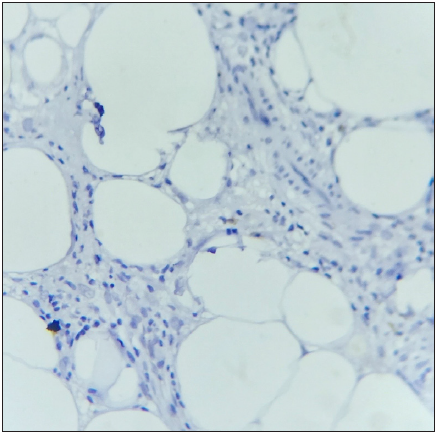
- The section shows absence of CD56+ NK cells. (IHC with DAB staining: 40x, Classic EN).
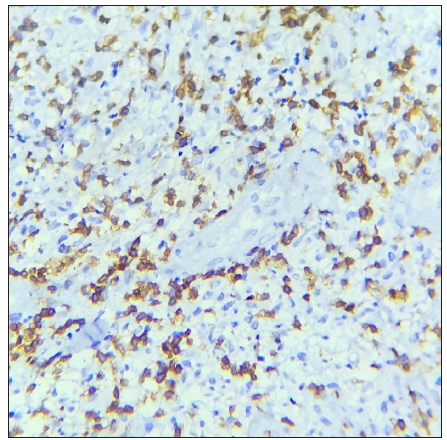
- The section shows marked presence of CD3+ T cells. (IHC with DAB staining: 40x, Chronic EN)
- The section shows an increased density of CD4+ T cells. (IHC with DAB staining: 40x, Chronic EN)
- The section shows notable presence of CD8+ T cells. (IHC with DAB staining: 40x, Chronic EN)
- The section shows scattered CD56+ NK cells. (IHC with DAB staining: 40x, Chronic EN)
Discussion
In our study of 41 biopsy-confirmed EN cases, we observed a predominance of females (65.85%), consistent with trends reported in various studies.8,9
PTB was the leading cause of EN in our cohort, accounting for 36.6% of all cases. This percentage is notably higher than in other studies. For instance, Mert et al.10 (2007) reported PTB-associated EN in 10% of cases, while Varas et al.11 (2016) found it in only 6.6%. This high prevalence likely reflects the local burden of tuberculosis, underscoring the need for comprehensive tuberculosis screening in EN patients. Additionally, the consistent presence of sarcoidosis across various studies, including ours, highlights the importance of ruling it out in all EN cases.9,11
While EN typically has a favourable prognosis, a subset of patients (36.59%) in our study experienced chronic or prolonged episodes. Notably, EN associated with idiopathic causes exclusively manifested as chronic EN, suggesting a possible link between undiagnosed systemic conditions and disease persistence. Among the idiopathic cases, two were associated with uncontrolled diabetes mellitus and one with hypothyroidism. In contrast, cases related to post-streptococcal infections resolved entirely after appropriate antibiotic therapy, indicating a favourable outcome in these cases. However, no statistically significant association was found between specific clinical diagnoses and the chronicity of EN lesions (p = 0.217).
Most cases (82.93%) presented with typical EN lesions, characterised by erythematous subcutaneous nodules on the shins. Similarly, Limtong et al.8 reported that 68% of patients exhibited typical shin lesions. However, our study observed a lower incidence of atypical presentations (17.07%) compared to Meienberger et al.,12 where 33% of patients displayed atypical EN. Although chronic cases in our study were more likely to have typical shin lesions (93.3%), this difference was not statistically significant (p = 0.232), aligning with the general understanding of EN’s unpredictable nature.
Immunohistochemical analysis on skin biopsy samples revealed that chronic EN cases exhibited significantly higher levels of CD3, CD4, CD8, and CD56 compared to classic EN. Although the CD4 to CD8 ratio did not show a statistically significant difference between the two groups, the higher levels of CD4+ T cells across all EN cases suggest a shift towards helper T cell response. This aligns with findings from Cao et al.13, who demonstrated higher CD4+ T cells and an increased CD4: CD8 ratio in EN patients compared to healthy controls using flow cytometry on peripheral blood samples, suggesting a prominent role of CD4+ T cells in the pathogenesis of EN.
De Simone et al.’s14 analysis of cytokine profiles in the serum and lesional skin of five patients with EN, three of whom had recurrent and persistent disease, revealed high levels of innate immunity cytokines (TNF-α, IL-6, IL-8), elevated Th1 cytokines (IFN-ℽ, IL-12), and low levels of Th2 cytokines. This suggests innate immune activation and a strong Th1 adaptive immune response in EN. These findings align with our observation of elevated CD56 levels, a marker for NK cells, and a significant increase in CD4 and CD8 T cell levels in chronic EN cases, indicating a dynamic interaction between innate immunity and Th1 adaptive response in the pathogenesis and chronicity of EN.
Our study also found significantly elevated baseline CRP levels and Mantoux test readings in chronic EN cases, indicating a stronger initial inflammatory response. This is consistent with findings from studies such as Cao et al.13, who reported significantly higher CRP and ESR levels in EN patients than healthy controls (p < 0.05) and Ioannou et al.15, who evaluated 138 EN patients and observed that relapsing cases were more likely to have a positive tuberculin test, suggesting a potential link.
Overall, our findings highlight the importance of monitoring inflammatory and immunological markers in patients with EN to identify those at risk for chronic disease progression. This approach may help identify individuals who require more intensive management and follow-up, potentially improving patient outcomes. These insights also suggest that therapies targeting both innate and adaptive immune responses could be beneficial in preventing disease chronicity.
Limitations
The study limitations include a small sample size and short follow-up duration. Further studies with larger cohorts and extended follow-up periods are recommended to validate these findings and enhance their generalisability. Multivariable analysis could not be performed due to the small sample size.
Conclusion
In summary, our study contributes to the existing evidence on EN by emphasising the role of tuberculosis as a predominant cause in regions with a high TB burden and the significance of immunological factors, such as T cell response, in disease chronicity. Further research is needed to explore the underlying mechanisms of EN progression and to develop targeted interventions for chronic cases.
Ethical approval
The research/study was approved by the Institutional Review Board at Kalinga Institute of Medical Sciences, number KIIT/KIMS/IEC/934/2022, dated 18.07.2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Funded by the IADVL PG Thesis Grant Fund and post-graduate student research grant of the university.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
References
- Panniculitis. Part I. Mostly septal panniculitis. J AmAcad Dermatol. 2001;45:163-83. quiz 184-6
- [CrossRef] [Google Scholar]
- Erythema nodosum: A sign of systemic disease. Am Fam Physician. 2007;75:695-700.
- [PubMed] [Google Scholar]
- Erythema nodosum: A practical approach and diagnostic algorithm. Am J Clin Dermatol. 2021;22:367-78.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical characteristics of erythema nodosum and associations with chronicity and recurrence. JAMA Dermatol. 2024;160:229-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- T-regulatory cells in erythema nodosum leprosum: An immunohistochemical and image morphometric study. Am J Dermatopathol. 2021;43:e149-57.
- [CrossRef] [PubMed] [Google Scholar]
- Image morphometric analysis of B cells and plasma cells in erythema nodosum leprosum with clinicopathological correlation. Am J Dermatopathol. 2021;43:700-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathological characteristics related to etiologies of erythema nodosum: A 10-year retrospective study. Clin Cosmet Investig Dermatol. 2021;14:1819-29.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Erythema nodosum: Etiologic and predictive factors in a defined population. Arthritis Rheum. 2000;43:584-92.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema nodosum: An evaluation of 100 cases. Clin Exp Rheumatol. 2007;25:563-70.
- [PubMed] [Google Scholar]
- [Erythema nodosum: Analysis of 91 hospitalized patients] Rev Med Chil. 2016;144:162-8.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical and typical presentation of erythema nodosum: Clinical differences in treatment and outcome. Dermatology. 2024;240:226-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Immunological profile of erythema nodosum and their relationship of C-reactive protein level and erythrocyte sedimentation rate: A retrospective analysis of 61 patients. Cell Mol Biol (Noisy-le-grand). 2022;68:136-40.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical, histopathological, and immunological evaluation of a series of patients with erythema nodosum. Int J Dermatol. 2016;55:e289-94.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical characteristics of patients with erythema nodosum and risk of relapse - a 17-year study. Maedica (Bucur). 2022;17:259-63.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






