Translate this page into:
Clinical difference between single subtype and mixed subtype chronic urticaria: A retrospective study
-
Received: ,
Accepted: ,
How to cite this article: Mao M, Yuan Y, Xiao Y, Peng C, Chen X, Li J. Clinical difference between single subtype and mixed subtype chronic urticaria: A retrospective study. Indian J Dermatol Venereol Leprol 2022;88:171-6.
Abstract
Background:
The subtypes of chronic urticaria share a common clinical expression, but may show differences phenotypically. Meanwhile, two or more different subtypes of chronic urticaria can coexist in any given patient which may involve different phenotypes.
Aims:
The study aims to compare the two phenotypes in terms of demographics, clinical profile and treatment response.
Methods:
In this retrospective study, 2678 chronic urticaria patients were divided into the single subtype chronic urticaria group and mixed subtype chronic urticaria group as was appropriate.The differences in the clinical features, possible causes, urticaria activity score of seven days, dermatology life quality index score, laboratory investigations and response to treatments were evaluated among the two groups.
Results:
An obvious female predominance was detected in chronic urticaria, especially in mixed subtype chronic urticaria patients. Of the 2678 chronic urticaria patients, there were 837(31.25%) mixed subtype chronic urticaria. Chronic spontaneous urticaria combined with symptomatic dermographism was the most common group in the mixed subtype chronic urticaria. Patients with mixed subtype chronic urticaria were more likely to have associated chest tightness/shortness of breath and showed greater urticaria activity. In patients with single subtype chronic urticaria, the positive rate of family history with allergic rhinitis, asthma or urticaria was lower. Based on evaluation of the treatment, control with second-generation antihistamines at licensed doses was achieved in only 38.83% of mixed subtype chronic urticaria patients, compared with 56.32% of patients with single subtype.
Limitations:
First, this study was a single-center design retrospective study. Second, omalizumab treatment was not included. Third, the differences between different subtypes of mixed subtype chronic urticaria were not discussed in detail.
Conclusion:
This study showed that mixed subtype chronic urticaria had some distinct features. Comprehensive knowledge about it may help us define effective therapeutic strategies and improve symptom control and the quality of life for chronic urticaria patients.
Keywords
Chronic inducible urticaria
chronic spontaneous urticaria
histamine H1 antagonists
Introduction
Urticaria is one of the most common skin diseases, and patients may present with a wide spectrum of symptoms, including sudden development of pruritic wheals and/or angioedema. Chronic urticaria is diagnosed when wheal has been continuously present for greater than or equal to six weeks.1 It has a significant impact on the patients’ quality of life due to the constant sensation of itching, regular recurrence and unknown etiology.2 Given this, the treatment of this skin disease is challenging and frustrating for both the patients and physicians.3,4
Chronic urticaria can be divided into chronic spontaneous urticaria and chronic inducible urticaria. More specifically, inducible urticaria includes symptomatic dermographism, cold urticaria, delayed pressure urticaria, heat urticaria, solar urticaria, vibratory angioedema, cholinergic urticaria, aquagenic urticaria and contact urticaria.1,5 Correct identification of chronic urticaria phenotypes has become a critical prerequisite for helping clinicians design effective therapeutic plans. When patients are diagnosed with chronic urticaria, they are often found to be involved with multiple subtypes, for example, a patient can suffer chronic spontaneous urticaria and symptomatic dermographism at the same time. This has also been mentioned in the EAACI/ GA(2)LEN/EDF/WAO guideline of urticaria 2013 and 2018,1,5 but no comprehensive study has been conducted about it. In this study, we named this group of chronic urticaria as mixed subtype chronic urticaria, while patients involving only one subtype as single subtype chronic urticaria.
The prevalence of chronic urticaria is estimated to be around 0.5% ~ 5%,4 but there is no specific information on the prevalence and clinic features of mixed subtype chronic urticaria. The clinical characteristics of chronic spontaneous urticaria, cholinergic urticaria, cold urticaria and symptomatic dermographism have beenreported.6-8 Nevertheless, there are no data regarding the characteristics of mixed subtype chronic urticaria. Therefore, we aimed to evaluate the socio demographic and clinical differences in the chronic urticaria subtype.
Methods
Study population
This retrospective study involved 2678 patients who were diagnosed with chronic urticaria between January 2016 and September 2019 from the urticaria cohort of a hospital. All enrolled subjects were active patients and were required to complete a specific survey containing questions regarding their general demographic characteristics, disease duration, frequency and duration of each episode, age of onset, accompanying symptoms, family history and laboratory tests. This study had been approved by the ethics committee (ethical approval number: 201311392) and was performed by the Declaration of Helsinki guidelines (registration number: ChiCTR-OCH-14004518). Written informed consent was obtained from each subject.
Definition of the chronic urticaria
Diagnosis of chronic urticaria was made by at least two dermatologists (members of the urticaria investigation group of the Chinese dermatology association) according to the EAACI/GA(2)LEN/EDF/WAO Guideline of Urticaria 2013.1 Single subtype chronic urticaria refers to the patient suffering only one subtype of chronic urticaria; by contrast, mixed subtype chronic urticaria refers to the patient suffering more than one subtype of chronic urticaria at the same time.
Laboratory investigations
Laboratory investigations included complete blood cell count, erythrocyte sedimentation rate, c-reactive protein level, thyroid-stimulating hormone, 25-hydroxy vitamin D levels and skin prick test. For the skin prick test, patients were treated with allergen reagent, and the test was carried out in duplicate on the flexor surface of the forearms, including a positive control with histamine (one milligram/milliliter) and a negative control with saline, as well as 20 types of inhalation allergen pricking solutions (i.e. dust mite; house dust mites; cockroach; acacia; mug wort; dog epithelium; cat epithelium; Cytospora; specific Penicillium; hay dust; cotton wool; beef; carp; shrimp; soybean; wheat flour; milk; eggs; red pepper and peanuts).Wheals with a mean diameter at least three millimeters or more than those of the negative control were considered positive reactions.9,10
Activity and quality of life of chronic urticaria
The seven days urticaria activity score (UAS7) was used to assess the patients’ disease activity.11 A table of dermatology life quality index was made to evaluate the patient’s quality of life. The UAS7 assesses the disease activity with two questions regarding wheals and itching over seven consecutive days which ranges from zero(no disease activity/ complete response to treatment) to 42 (highest possible disease activity).12The dermatology life quality index is a validated, dermatology-specific ten-item questionnaire covering six areas: symptoms and feelings; daily activities; leisure; work and school; personal relationships and effects of treatment on daily life. This score ranges from zero to 30.13
Treatment and efficacy
Treatment regimens refer to the 2013 EAACI/GA(2)LEN/ EDF/WAO guidelines1,12 and adopt a ladder approach. First of all, patients were treated with second-generation nonsedative antihistamines (desloratadine citrate 8.8mg or levocetirizine 5 mg). If symptoms persist after four weeks, the second-generation non-sedative antihistamines combination therapy would be given (desloratadine citrate 8.8mg/day and levocetirizine 5 mg/day). If symptoms persist after four weeks, cyclosporine A 2–3mg/kg/day or montelukast10mg/ day was added to the therapeutic regimen. Changes in UAS7 were used to assess therapeutic efficacy. According to our previous research, the responders were designated as those with UAS7 achieving 50% or more significant improvement as compared with the baseline before treatment. Nonresponders were defined as those patients who had a score that decreased below 50%.14,15
Statistical analysis
SPSS version 23.0 (IBM Co, Armonk, NY, USA) and GraphPad Prism v.5.04 for Windows were used. For all the subtypes of chronic urticaria, descriptive statistics were provided. Quantitative variables were described as means and standard deviations. The relationships between different parameters and chronic urticaria were determined by the Student’s t-test for continuous variables and by the Pearson’s χ2 test for dichotomous variables. For all statistical analyses: *P<0.05; **P< 0.01, ***P< 0.001 and P< 0.05 were considered statistically significant.
Results
Differences between the single subtype and the mixed subtype chronic urticaria in demographic characteristics
Among the 2678 patients with chronic urticaria, 1841(68.7%) patients belonged to single subtype, and the remaining 837 (31.3%) patients belonged to mixed subtype[Figure 1a]. Chronic spontaneous urticaria was the most common type of singlesubtype group [Figure 1b]. The patients with chronic spontaneous urticaria combined with symptomatic dermographism account for 638 (76.2%) of mixed subtype, the highest share in this group [Figure 1c].
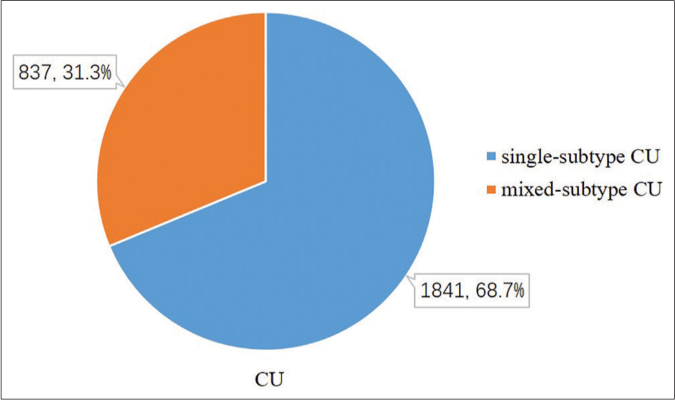
- Among the 2678 patients with chronic urticaria, 1841(68.7%) patients belonged to single-subtype and 837 (31.3%) patients belonged to mixed-subtype.
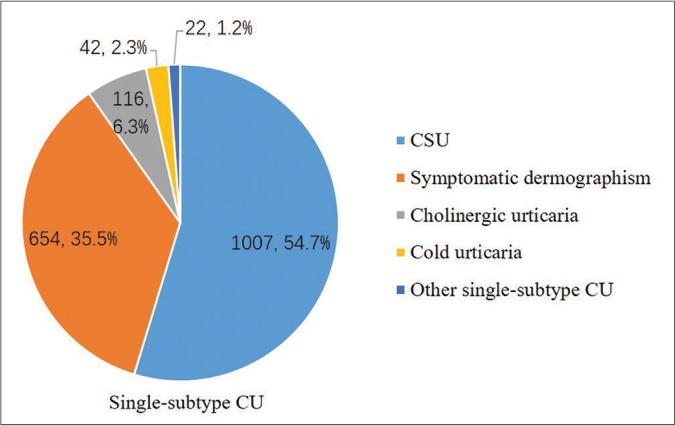
- Single-subtype chronic urticaria patients were divided into 5 groups, including 1007(54.7%) chronic spontaneous urticaria, 654(35.5%) symptomatic dermographism, 116(6.3%) cholinergic urticaria, 42(2.3%) cold urticaria and 22(1.2%) other single-subtype chronic urticaria. Other single-subtype chronic urticaria, including 4 delayed pressure urticaria, 4 solar urticaria, and 14 contact urticaria.
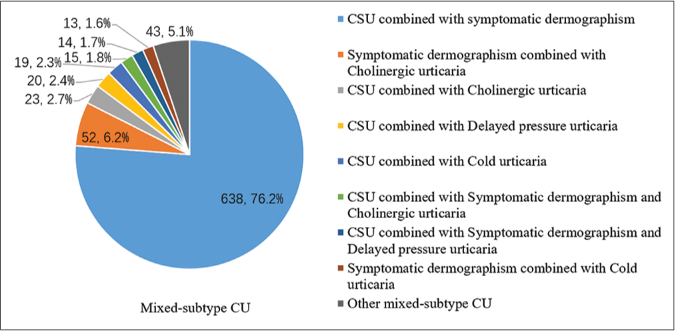
- The mixed-subtype chronic urticaria was divided into 9 groups, including 638(76.2%) chronic spontaneous urticaria combined with symptomatic dermographism, 52(6.2%) symptomatic dermographism combined with cholinergic urticaria, 23(2.7%) chronic spontaneous urticaria combined with cholinergic urticaria, 20(2.4%) chronic spontaneous urticaria combined with delayed pressure urticaria, 19(2.3%) chronic spontaneous urticaria combined with cold urticaria, 15(1.8%) chronic spontaneous urticaria combined with symptomatic dermographism and cholinergic urticaria,14(1.7%) chronic spontaneous urticaria combined with symptomatic dermographism and delayed pressure urticaria, 13(1.6%) symptomatic dermographism with cold urticaria and 43(5.1%) other mixed-subtype chronic urticaria. Other mixed-subtype chronic urticaria including 3 symptomatic dermographism combined with heat contact urticaria, 2 symptomatic dermographism combined with aquagenic urticaria, 5 symptomatic dermographism combined with solar urticaria, 7 chronic spontaneous urticaria combined with heat contact urticaria, 3 chronic spontaneous urticaria combined with solar urticaria, 1 cholinergic urticaria combined with cold urticaria, 4 cholinergic urticaria combined with solar urticaria, 2 cholinergic urticaria combined with heat contact urticaria, 6 chronic spontaneous urticaria symptomatic dermographism and cold urticaria and 10 chronic spontaneous urticaria symptomatic dermographism and cholinergic urticaria.
The demographic characteristics of patients included in this study are summarized in Table 1. An obvious female predominance was detected, and the mixed subtype group had a statistically significantly higher percentage of female subjects than the single subtype (549[65.6%] vs.1127[61.2%], P=0.03). There was no difference between the two groups with regard to average age, course, occupation and education level [Table 1].
| Parameter | Single subtype (n[%]/Mean±standard deviations) | Mixed subtype (n[%]) | P- value |
|---|---|---|---|
| Sex | |||
| Female | 1127 (61.2) | 549(65.6) | 0.03 |
| Male | 714 (38.8) | 288 (34.4) | 0.03 |
| Age(year) | 35.6±14.9 | 34.8±14.7 | 0.37 |
| Average course (month) | 26.3±47.1 | 25.6±48.8 | 0.14 |
| Education | |||
| Junior college or above | 602 (32.7) | 290 (34.6) | 0.34 |
| Vocational/high school | 982 (53.3) | 434 (51.8) | 0.50 |
| Junior middle school | 153 (8.3) | 77 (9.2) | 0.49 |
| Elementary school or below | 103 (5.6) | 36 (4.4) | 0.19 |
| Occupation | |||
| Commerce or service personnel | 305 (16.6) | 153 (18.3) | 0.30 |
| Workers | 86 (4.7) | 36 (4.4) | 0.74 |
| Farmers and fishers | 79 (4.3) | 41 (5.0) | 0.19 |
| Professional and technical personnel | 166 (9.0) | 85 (10.2) | 0.39 |
| Managers | 145 (7.9) | 59 (7.0) | 0.50 |
| Clerical and education people | 68 (3.7) | 24 (2.9) | 0.38 |
| Students | 344 (18.8) | 171 (20.5) | 0.31 |
| Retired people | 145 (7.9) | 64 (7.8) | 0.89 |
| Domestic worker | 218 (11.8) | 97 (11.7) | 0.90 |
| Others | 284 (15.5) | 122 (14.6) | 0.61 |
Differences according to clinical features between the single subtype and the mixed subtype chronic urticarial
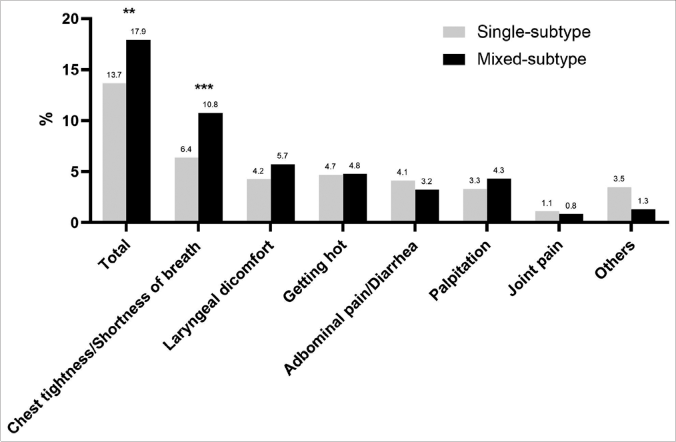
Self-reported accompanying symptoms were present in 252(13.7%) single subtype group patients and 150(17.9%) mixed subtype group. Moreover, the mixed subtype group is more likely to have accompanied symptoms (P=0.004). Chest tightness/shortness of breath was the most frequent concomitant symptom in both groups, and its incidence in the mixed subtype group was significantly higher than that in the single subtype group (P< 0.001). It is noteworthy that some patients reported two or more concomitant symptoms [Figure 2a].
- Comparison of concomitant symptoms between single subtype and mixed subtype chronic urticaria (n[%])
In the single subtype group, 222 subjects (12.1%) had a family history of allergic rhinitis and asthma, and 309 patients (16.8%) had a family history (first- and second-degree relatives) of chronic urticaria. While in the mixed subtype group, patients with allergic rhinitis and asthma family history accounted for 186(22.2%) and patients with a family history of urticaria accounted for 230(27.5%), all of which were higher than those in the single subtype group (P<0.001 and P <0.001) [Figure 2b].
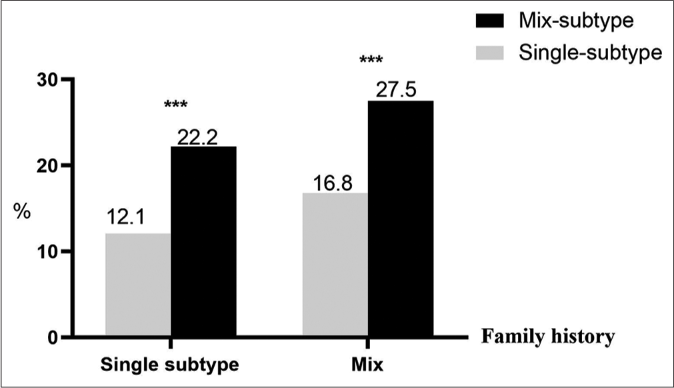
- Comparison of individual history and family history of chronic urticaria with single subtype and mixed subtype
Besides, the UAS7 and the dermatology life quality index were used to assess the patients’ disease activity and quality of life. Mixed subtype chronic urticaria tends to have a higher UAS7 (22.3vs. 24.0, P=0.002) and a UAS7 (5.1 vs. 5.6, P=0.009) [Figures 2c and 2d].
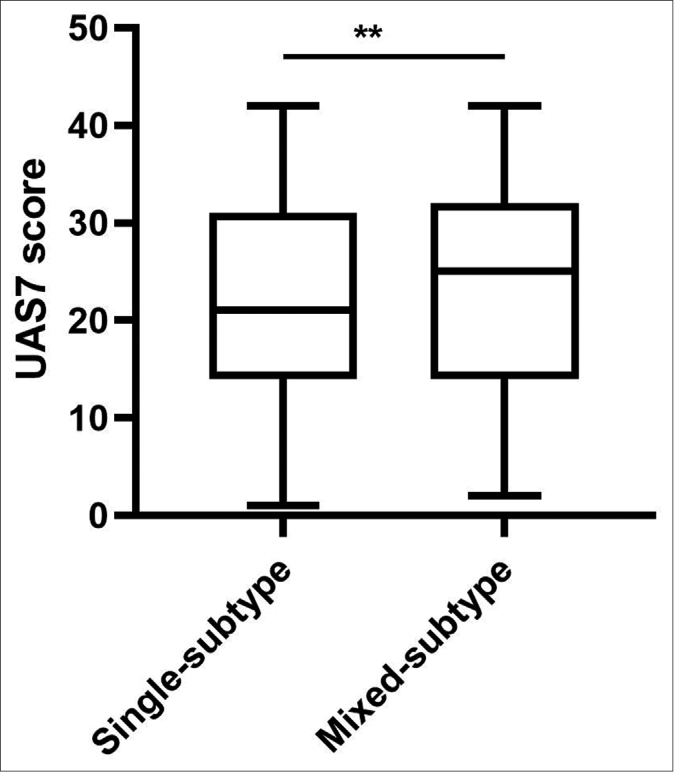
- Comparison of UAS7 score between single subtype and mixed subtype chronic urticaria
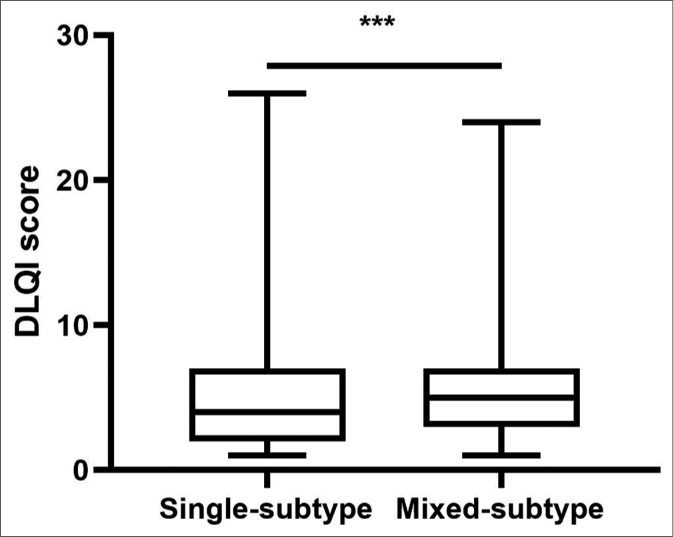
- Comparison of DLQI score between single subtype and mixed subtype chronic urticaria. *P<0.05, **P<0.01, ***<0.001
Laboratory examination and response to treatment of the single subtype and the mixed subtype chronic urticaria
In the present study, the single subtype group had a higher percentage of elevated white blood cell (111[6.0%] vs. 32[3.8%], P=0.019) and platelet (190[10.3%]vs. 44[5.3%], P<0.001), while the mixed subtype group had a higher percentage of elevated erythrocyte sedimentation rate (221 [26.4%] vs. 330[17.9%], P<0.001) and skin prick test positive (126 [15.1%] vs. 150[8.2%], P<0.001).
An episode of urticaria was controlled using a first-line treatment (desloratadine citrate 8.8mg or levocetirizine 5mg) in only 325(38.8%) patients of the mixed subtype group, in contrast to 1037(56.3%) patients of the single subtype group (P<0.001). Meanwhile, the mixed subtype group reacted worse to the treatment with the second-line (desloratadine citrate 8.8mg/day and levocetirizine 5milligram/day, P<0.001) and third-line treatment(cyclosporin A 2–3mg/kg/day or montelukast 10milligram/day, P<0.001). Comparatively, the mixed subtype group chronic urticaria was much harder to control [Table 2].
| Single subtype(n[%]) | Mixed subtype(n[%]) | P- value | |
|---|---|---|---|
| Complementary tests/laboratory analyses | |||
| Elevated WBC | 111(6.0) | 32(3.8) | 0.019 |
| Elevated PLT | 190(10.3) | 44(5.3) | ₛ 0.001 |
| Elevated ESR | 330(17.9) | 221(26.4) | ₛ 0.001 |
| Elevated CRP | 67(3.6) | 22(2.6) | 0.22 |
| Abnormal TSH | 193(10.5) | 69(8.2) | 0.082 |
| Declined 25-OH-VD | 1593(86.5) | 726(86.7) | 0.931 |
| Positive of the skin prick test | 150(8.2) | 126(15.1) | ₛ 0.001 |
| Controlling the episode | 1700(92.3) | 725(86.6) | ₛ 0.001 |
| 1stline anti-H1 | 1037(56.3) | 325(38.8) | ₛ 0.001 |
| 2ndline anti-H1 | 550(29.9) | 330(39.4) | ₛ 0.001 |
| 3rdline | 113(6.1) | 87(10.4) | ₛ 0.001 |
WBC: White blood cell, PLT:Platelet, ESR:Erythrocyte sedimentation rate, CRP:C-reactive protein, TSH:Thyroid-stimulating hormone. 1stline anti-H1: Second-generation non-sedative antihistamines, licensed doses. 2ndline anti-H1: Second-generation non-sedative antihistamines combination. 3rdline: CSA or montelukast
Discussion
Chronic urticaria is a common skin disease, in which identifying the clinical characteristics of different types is important for predicting prognosis and therapeutic behavior. However, we were unable to find any previous reports of the clinical features and laboratory differences within these two groups of chronic urticaria.
Chronic urticaria is one of the skin diseases that exhibit a significant female preponderance with an average female-to-male ratio of nearly 1.2–2:1.16,17 It was also found in our study especially in the mixed subtype group. More than 50% of the patients had a vocational/high school level of education in both groups which is above the average percentage in China (15.0%) or in Hunan Province (16.7%), according to the 6th national population census conducted in 2010 (http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm). There are several possible reasons for this: First, the present study is a tertiary referral hospital-based survey. Second, most of the patients to the hospital have better economic conditions and medical insurance. Third, the sample size of this study is relatively small.
Available evidence indicates that all forms of chronic urticaria can substantially affect patients’ quality of life, ability to perform daily tasks,18,19 and was correlated with disease activity, notably so in daily activity and sleep interference domains. Particularly in patients with a UAS7 of 16 or greater, the overall impact of chronic urticaria on usual activities represents a significant burden to themselves and to society.3 The best method for assessing activity is UAS7 since this instrument evaluates the seven days before the consultation, evaluating more broadly a disease that has a fluctuating course.20 In this study, the mixed subtype group had higher UAS7 scores and dermatology life quality index scores which indicated that mixed subtype chronic urticaria has a significant negative impact on the quality of life in chronic urticaria patients.
Interestingly, compared with single subtype chronic urticaria, the licensed doses of the first-line antihistamine were only useful for 325(38.8%) patients with mixed subtype chronic urticaria. Meanwhile, a higher percentage of the patients with mixed subtype patients required a combination of two antihistamines or third-line treatment, and 112(13.4%) of the mixed subtype patients did not respond. Based on a comprehensive analysis of the results, above differences in clinical features and disease progression were observed between single subtype and mixed subtype patients which may indicate a need for special consideration of these phenotypes in the future regarding guidelines of urticaria management.
Limitations
Limitations applied to this research should be highlighted. First, as a single-center design retrospective study, the clinical characteristics of chronic urticaria in this study may vary from region to region. The data would be more convincing if a multicountry or multicenter study could be conducted. Second, omalizumab and other new therapeutic regimentation have not been popularized across all regions of China, so omalizumab treatment was not included in this study. In addition, the differences between different subtypes of mixed subtype chronic urticaria were not discussed in detail, and more comprehensive research should be conducted in the future.
Conclusion
In the present study, we studied a large group of mixed subtype chronic urticaria which has distinct features. The importance and uniqueness of mixed subtype chronic urticaria have long been neglected. Despite several limitations to this study, our data emphasize the usefulness of analyzing clinical differences between chronic urticaria subtypes. Clear-cut differences were detected among different subtypes that might directly affect the treatment response. In this sense, the comprehensive evaluation may help in designing a rational therapeutic strategy for subsequently reducing the disease burden.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The EAACI/GA(2) LEN/EDF/WAO guideline for the definition, classification, diagnosis, and management of urticaria: The 2013 revision and update. Allergy. 2014;69:868-87.
- [CrossRef] [Google Scholar]
- Epidemiology of urticaria: A representative cross-sectional population survey. Clin Exp Dermatol. 2010;35:869-73.
- [CrossRef] [Google Scholar]
- The burden of chronic spontaneous urticaria is substantial: Real-world evidence from ASSURE-CSU. Allergy. 2017;72:2005-16.
- [CrossRef] [Google Scholar]
- EAACI/GA(2)LEN/EDF/ WAO guideline: Management of urticaria. Allergy. 2009;64:1427-43.
- [CrossRef] [Google Scholar]
- The EAACI/GA2LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy. 2018;73:1393-414.
- [CrossRef] [Google Scholar]
- Cold urticaria: A 20-year follow-up study. J Eur Acad Dermatol Venereol. 2016;30:2066-71.
- [CrossRef] [Google Scholar]
- Cholinergic urticaria: More than a simple inducible urticaria. Aust J Dermatol. 2017;58:e193-8.
- [CrossRef] [Google Scholar]
- Chronic spontaneous urticaria: Etiology and pathogenesis. Immunol Allergy Clin North Am. 2014;34:33-52.
- [CrossRef] [Google Scholar]
- The significance of allergic contact urticaria to milk in children with cow's milk allergy. Pediatr Allergy Immunol. 2015;26:218-22.
- [CrossRef] [Google Scholar]
- Skin tests for immediate, Type I, allergic reactions. Proc R Soc Med. 1972;65:271-2.
- [CrossRef] [Google Scholar]
- How to assess disease activity in patients with chronic urticaria? Allergy. 2008;63:777-80.
- [CrossRef] [Google Scholar]
- Chronic urticaria: Tools to aid the diagnosis and assessment of disease status in daily practice. J Eur Acad Dermatol Venereol. 2015;29:38-44.
- [CrossRef] [Google Scholar]
- Dermatology life quality index (DLQI)--a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-6.
- [CrossRef] [Google Scholar]
- Association of ORAI1 gene polymorphisms with chronic spontaneous urticaria and the efficacy of the nonsedating H1 antihistamine desloratadine. J Allergy Clin Immunol. 2017;139:1386-8.e9.
- [CrossRef] [Google Scholar]
- Plasma adenosine is linked to disease activity and response to treatment in patients with chronic spontaneous urticaria. Allergy. 2020;76:571-3.
- [CrossRef] [Google Scholar]
- Gender-related differences in chronic urticaria. G Ital Dermatol Venereol. 2016;151:544-52.
- [Google Scholar]
- Chronic urticaria in Chinese population: A hospital-based multicenter epidemiological study. Allergy. 2014;69:359-64.
- [CrossRef] [Google Scholar]
- Impact of chronic urticaria on quality of life and work in Japan: Results of a real-world study. J Dermatol. 2018;45:963-70.
- [CrossRef] [Google Scholar]
- Analysis of disease activity categories in chronic spontaneous/ idiopathic urticaria. Br J Dermatol. 2017;177:1093-101.
- [CrossRef] [Google Scholar]
- The impact of chronic idiopathic urticaria on quality of life in korean patients. Ann Dermatol. 2009;21:226-9.
- [CrossRef] [Google Scholar]






