Translate this page into:
Clinical outcome of collodion baby: A retrospective review
2 Department of Pediatric Dermatology, Indira Gandhi Institute of Child Health, Bangalore, India
Correspondence Address:
Sahana M Srinivas
No 874,14th cross, Mahalakshmi layout, Bangalore
India
| How to cite this article: Aradhya SS, Srinivas SM, Hiremagalore R, Shanmukappa AG. Clinical outcome of collodion baby: A retrospective review. Indian J Dermatol Venereol Leprol 2013;79:553 |
Sir,
Collodion baby refers to a newborn with a parchment-like membrane covering the entire body surface. The collodion baby is not a disease entity but phenotype common to several disorders. A total of 60%-80% of children born with a collodion membrane eventually develop ichthyosis either nonbullous ichthyosiform erythroderma or lamellar ichthyosis. Around 10%-20% eventually develop normal skin, referred to as self-healing collodion baby. [1] The derivation of the study is well-known. There are few published reports studying the eventual clinical outcome of collodion baby. There are no reports regarding this in this part of the globe; hence, the present study was undertaken.
The work comprised retrospective study of 22 cases of collodion baby that presented to us over a period of 1 year 8 months from January 2011 to October 2012. The study was conducted at Dermatology outpatient department at Victoria hospital and Indira Gandhi Institute of Child Health, Bangalore. Retrospective diagnosis of collodion baby was based either on case note review or recall bias. This was the limitation factor in our study. New cases of collodion baby were also included and were followed-up to the end of study period.
Of these 22 children, 12 (54.5%) were males and 10 (45.45%) were females. The male to female ratio was 1.2:1. The study patient′s age ranged from 1 day to 12 years. Among them six were neonates who presented with collodion membrane. Follow-up of these neonates varied from 4 to 7 months. The median age of presentation in neonates was 3.6 days (1-9 days). Fifteen children were born out of consanguineous parents (68.18%). Two children were born preterm. The clinical characteristics of study patients are summarized in [Table - 1]. Ectropion and/or eclabium were present in 16 children born as collodion baby at the time of birth. In two children, ectropion was persisting up to age of 12 years. These two children had bathing suit ichthyosis. Shedding of the collodion membrane occurred between 7 and 26 days (average of 17.1days) of age. Two children with lamellar ichthyosis had rickets. There were two sets of siblings (twins). One set of twins were 12 years old, had developed bathing suit ichthyosis, and another set of twins were 3 months old, had developed nonbullous ichthyosiform erythroderma.
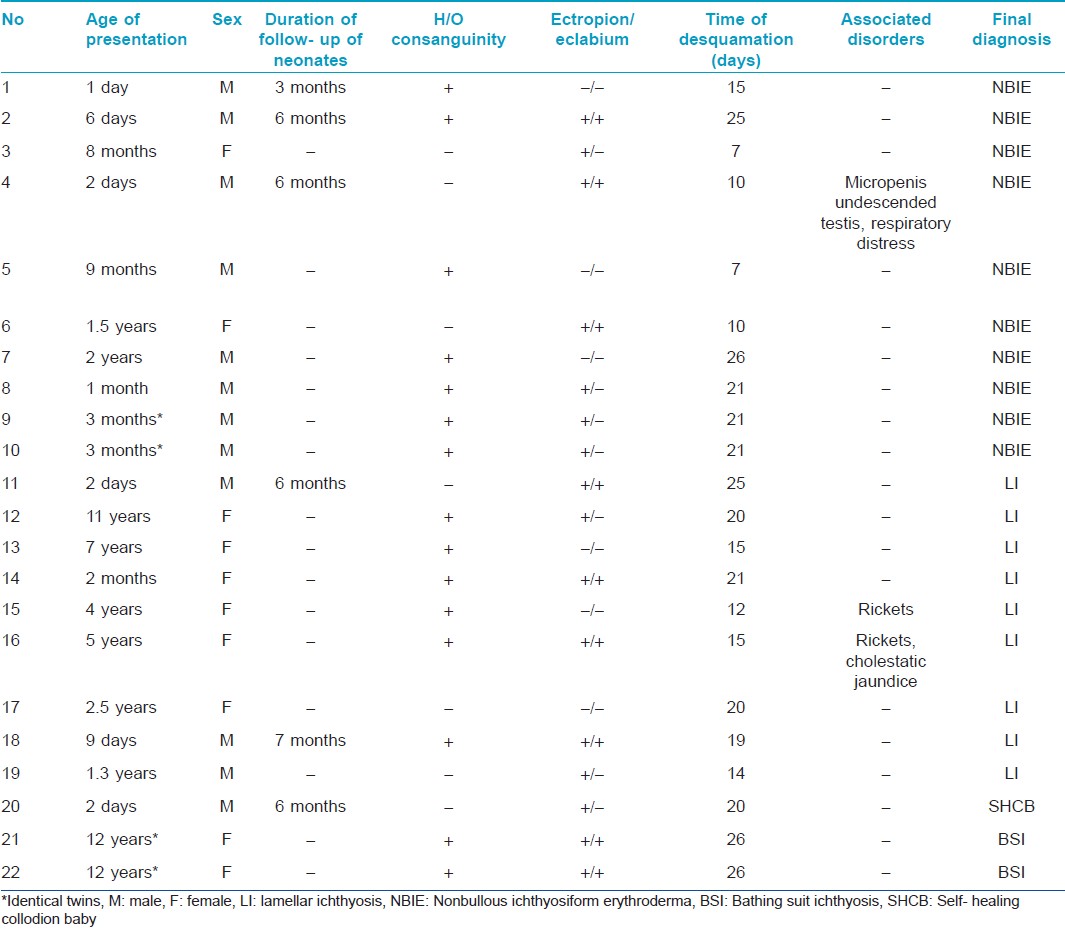
The final diagnosis in this cohort, based on clinical features and histology, was nonbullous ichthyosiform erythroderma in 10 children (NBIE, 45.45%), lamellar ichthyosis in nine children ( LI, 40.09%), two children (9.09%) who were identical twins had bathing suit ichthyosis and one child (4.54%) showed normal skin called as self healing collodion baby.
Collodion membrane at birth is gradually shed over 2 to 4 weeks usually revealing an ichthyosis phenotype [Figure - 1] and [Figure - 2]. Rarer forms of congenital ichthyosis including trichothiodystrophy, gauchers disease, neutral lipid storage disease, Conradi-Hunermann disease, Sjogren- Larsson syndrome, and isolated palmoplantar keratoderma may be preceded by a collodion membrane. [2]
 |
| Figure 1: One-day-old male child with collodion membrane at birth |
 |
| Figure 2: Follow-up of the child after 2 months showing lamellar ichthyosis |
In our study, two children with lamellar ichthyosis also had rickets. Vitamin D deficiency is a well-recognized complication of ichthyosis possibly due to reduced exposure to sunshine, poor penetration of ultraviolet rays through thickened skin and alterations in epidermal cholesterol metabolism. [3]
The diagnosis of collodion baby is made clinically and skin histology in the first few weeks of life is unhelpful. The nature of scaling and intensity of erythroderma are important clinical features that distinguish between NBIE and LI. Histologically, parakeratosis and inflammatory cell infiltration are seen more frequently in NBIE than in LI and the stratum corneum is usually thicker in LI than in NBIE. However, neither histopathological findings nor ultrastructural features seem to help clearly distinguish between NBCIE and LI. [4] Electron microscopy has been reported to be helpful in predicting whether a baby will ultimately have normal skin or ichthyosis. Ultrastructural features at first and 15 days of life in self-healing collodion baby show normal epidermal structure as compared to dysplastic stratum corneum seen in those who developed erythrodermic ichthyosis. [2]
Mutations in the genes TGM1, ALOXE3, and ALOX12B are implicated in most cases of collodion baby. Collodion baby should be placed in humidified incubators to maintain body temperature and prevent dehydration with regular monitoring of vitals, blood counts, and electrolytes. Skin care includes frequent application of emollients. [5]
Identifying the cause of collodion membrane includes good history, clinical examination, and investigations like skin biopsies and mutational analysis. Parents should be advised that the diagnosis will emerge after weeks or months of follow-up.
| 1. |
Williams ML, Elias PM. Heterogeneity in autosomal recessive ichthyosis. Clinical and biochemical differentiation of lamellar ichthyosis and non bullous congenital ichthyosiform erythroderma. Arch Dermatol 1985;121:477-88.
[Google Scholar]
|
| 2. |
Van Gysel D, Lijnen RL, Moekti SS, de Laat PC, Oranje AP. Collodion baby: A follow up study of 17 cases. J Eur Acad Dermatol Venereol 2002;16:472-5.
[Google Scholar]
|
| 3. |
Chouhan K, Sethuraman G, Gupta N, Sharma VK, Kabra M, Khaitan BK, et al. Vitamin D deficiency and rickets in children and adolescents with ichthyosiform erythroderma in type IV and V skin. Br J Dermatol 2012;166:608-15.
[Google Scholar]
|
| 4. |
Akiyama M, Sawamura D, Shimizu H. The clinical spectrum of nonbullous congenital ichthyosiform erythroderma and lamellar ichthyosis. Clin Exp Dermatol 2003;28:235-40.
[Google Scholar]
|
| 5. |
Prado R, Ellis LZ, Gamble R, Funk T, Arbuckle HA, Bruckner AL. Collodion baby: An update with a focus on practical management. J Am Acad Dermatol 2012;67:1362-74.
[Google Scholar]
|
Fulltext Views
4,774
PDF downloads
1,663





