Translate this page into:
Clinico-dermoscopic and histopathological features of folliculitis decalvans of beard area
Corresponding author: Dr. Siddhartha Dash Department of Dermatology, Venereology, and Leprology, Srirama Chandra Bhanja Medical College & Hospital, Cuttack, Odisha, India. siddharth101990@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dash S, Samal SR, Mohanty P, Mohanty J, Kulnu AD, Nayak N. Clinico-dermoscopic and histopathological features of folliculitis decalvans of beard area. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1471_2024
Dear Editor,
Folliculitis decalvans (FD) is a chronic inflammatory disease of the hair follicle, leading to follicular destruction and cicatricial alopecia. It constitutes about 11% of primary cicatricial alopecias, predominantly affecting young to middle-aged men.1 Typically, FD manifests on the scalp, especially the vertex, with single or grouped follicular pustules that expand centrifugally. Rarely, it may involve other hairy regions. Exclusive beard involvement is uncommon and has been reported only once before.1 We report two more cases of FD with exclusive beard involvement.
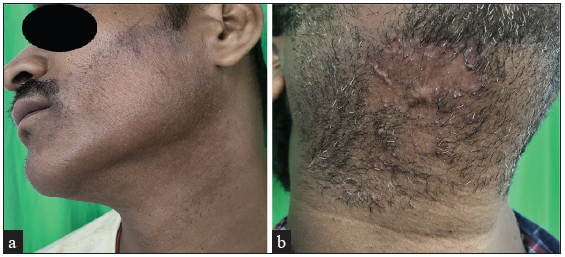
Two men aged 30 and 40 years presented with alopecic patches in the beard area for 6 and 18 months, respectively. There was no history of hair loss from the scalp or other body areas. There was no cervical lymphadenopathy. Cutaneous examination revealed diffuse scarring alopecic patches on both sides of the beard in the first patient and a solitary shiny erythematous patch of cicatricial alopecia below the right mandibular angle in the second [Figure 1a and 1b]. Discrete pustules were present along the lesion peripheries. Perifollicular scales/crusts, perifollicular starburst pattern, white and milky red areas, perifollicular erythema, vessels, follicular pustules, vellus hairs, and haemorrhagic crusts were seen on trichoscopy in both the cases [Figures 2a-2d]. Gram staining of the pustules revealed neutrophils, but no bacteria, and potassium hydroxide (KOH) mount was negative for dermatophytes. The bacterial and fungal culture of the pus showed no growth. Differential diagnosis of FD, sycosis barbae, and tinea barbae was considered. Histopathology showed a dense perifollicular neutrophilic and lymphoplasmacytic infiltration, decreased follicular density, loss of sebaceous glands, and vague concentric fibrosis around hair follicles [Figures 3a and 3b]. Clinico-trichoscopic-histopathological findings confirmed a diagnosis of FD. Both patients were treated with oral doxycycline (200 mg) and low-dose oral prednisolone (30 mg) daily. Oral prednisolone was rapidly tapered over six weeks and stopped. After six weeks, there were no new pustules or any extension of scarring [Figure 4a and 4b].
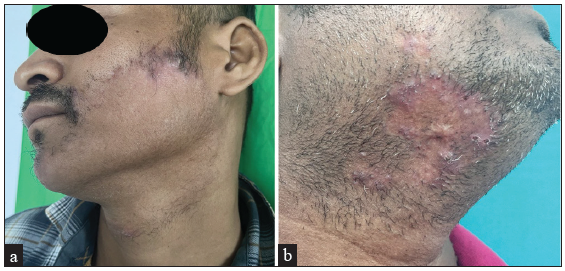
- (a-b) Both cases showing diffuse cicatricial alopecic patches on the beard area with follicular pustules and scaling/crusting in the peripheral spreading margin.
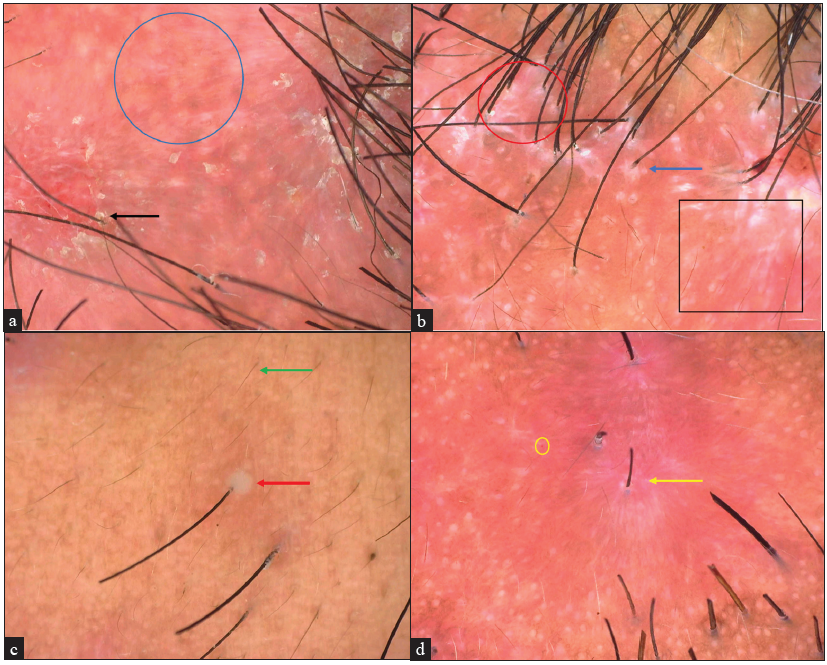
- Dermoscopic examination using Dinolite edge (AM7515MZT) with 62x magnification under polarised mode of both cases showing (a) lack of follicular ostia (blue circle), perifollicular scales/crusts (black arrow) (b) perifollicular starburst pattern (blue arrow), white and milky red areas (black square), interfollicular keloid like areas (red circle) and (c) follicular pustules (red arrow), vellus hairs (green arrow), and haemorrhagic crusts (d) perifollicular erythema (yellow arrow), dotted vessels (yellow circle).
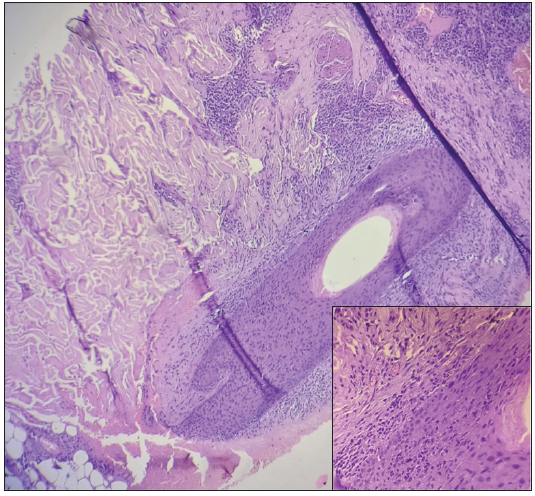
- Intrafollicular and perifollicular infiltration of lymphocytes and neutrophils in the first case (Haematoxylin and eosin, 100x, inset 400x).
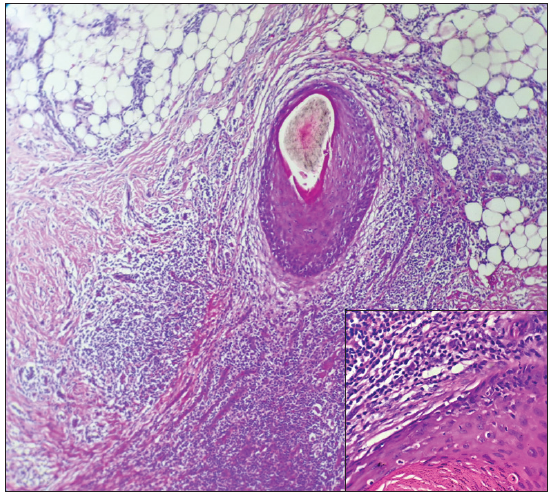
- Intrafollicular and perifollicular infiltration of mixed inflammatory infiltrate (predominantly neutrophils and lymphocytes) in the second case (Hematoxylin and eosin, 100x, inset 400x).
- Subsidence of lesions with scarring after six weeks of treatment in both cases.
The aetiology of FD remains unclear. However, the interaction between Staphylococcus aureus infection and the host has been suggested, given its isolation from follicular pustules. Other proposed factors include immune response impairments, leucokyte dysfunction, and structural follicular abnormalities.2 Clinically, FD is a scarring alopecia having follicular pustules, perifollicular scaling/crusting, and tufted hairs associated with pruritus and trichodynia, mostly over the scalp.2 Beard involvement, especially without scalp involvement, is uncommon. A previous report by Senatore et al. described a similar presentation, which responded to oral doxycycline.1 Both our cases presented with classical clinical findings except tufted hairs.
The classical dermoscopic features of FD have been described in Table 1.3 Our cases exhibited characteristic dermoscopic features except tufted hairs emerging from the same ostium. Both patients responded well to oral doxycycline and oral corticosteroids. The differential diagnosis of FD of the beard area includes lupoid sycosis barbae, tinea barbae, and pseudofolliculitis barbae, with distinguishing clinical, dermoscopic, and histopathologic features [Table 1].1,3,4,5 Lupoid sycosis looks clinically exactly similar to our cases, but both our FD cases were differentiated on the basis of histopathology. Histopathology of FD is predominated by perifollicular neutrophilic and lymphocytic infiltration, and the histopathology of lupoid sycosis barbae is predominated by epithelioid cell granulomas and perifollicular mononuclear cell infiltration.5 However, we believe that both FD and lupoid sycosis of the beard area could be similar entities. The reasons include a paucity of reports on lupoid sycosis, the similar clinical presentation of both entities, the inability to isolate bacteria from lupoid sycosis pustules, the disease mimicking histopathological features of late-stage FD and being refractory and responsive to antibiotic and anti-inflammatory drugs, respectively.5 Mild cases of FD can be treated with topical and intralesional corticosteroids, tacrolimus, and topical antibiotics, Severe cases may require oral antibiotics, oral corticosteroids, and isotretinoin. Adalimumab has been reported to be effective in treating resistant cases.6
| Clinical entity | Clinical features | Dermoscopic features | Histopathologic features |
|---|---|---|---|
| Folliculitis decalvans | Follicular pustules surrounding central cicatricial alopecic patch | Lack of follicular ostia, tufted hairs emerging from the same ostium, yellowish serous crusts, reddish haemorrhagic crusts, perifollicular scales, white and milky red areas, interfollicular keloid-like areas, perifollicular starburst pattern, perifollicular erythema, follicular pustules, broken hairs, vellus hairs, and keratotic plugs | Intrafollicular andperifollicular neutrophilic infiltration initially, later developing into mixed inflammatory infiltration consisting of neutrophils, lymphocytes, and plasmacytes with inflammatory granulomas |
| Lupoid sycosis (rare cicatricial form of chronic folliculitis) | Central circinate scarring surrounded by papules and pustules, giving the appearance of lupus vulgaris | NA | Epithelioid cell granulomas without central necrosis and a dense inflammatory infiltrate of mononuclear cells around blood vessel walls and hair follicles |
| Sycosis barbae | Follicular pustules with perilesional erythema, which may lead to scarring in long-standing forms | Central round pustule with peripheral sparse dotted vessels | Follicular neutrophilic and bacterial infiltration in the epidermis and mild-moderate mixed-type infiltrate in the papillary and middle dermis |
| Tinea barbae (Kerion) | Red boggy swelling with pustules and crusting | Broken hairs, corkscrew hairs, black dots, zigzag hairs, and morse-code hairs | Superficial and deep mixed perifollicular infiltrate with positive PAS staining. |
| Pseudofolliculitis barbae | Follicular papules, pustules with post inflammatory hyperpigmentation | U-shaped in-growing hair | Epidermal penetration of the shaft forms neutrophilic micro-abscess. Dermal penetration leads to a more severe foreign body granulomatous type of inflammatory reaction |
NA: Not available, PAS: Periodic acid schiff
This report highlights the uncommon presentation of FD confined to the beard area. We have also described the dermoscopic features of FD of the beard area and discussed the dermoscopic features of various differentials of FD of the beard area.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Folliculitis decalvans with exclusive beard involvement. Indian J Dermatol Venereol Leprol. 2021;87:569-71.
- [CrossRef] [PubMed] [Google Scholar]
- Folliculitis decalvans: A multicentre review of 82 patients. Acad Dermatol Venereol. 2015;29:1750-7.
- [Google Scholar]
- Histopathologic and dermoscopic features of 42 cases of folliculitis decalvans: A case series. J Am Acad Dermatol. 2021;85:1185-93.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of viral folliculitis of the beard: Report of two cases. Dermatol Pract Concept. 2022;12:e2022055.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Beard alopecia: An updated and comprehensive review of etiologies, presentation and treatment. J Clin Med. 2023;12:4793.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





