Translate this page into:
Clinicoepidemiological profile of 590 cases of beetle dermatitis in western Orissa
2 Department of Skin and VD, SCB Medical College, Cuttack, Orissa, India
Correspondence Address:
T Padhi
Department of Skin and VD, VSS Medical College, Burla, Orissa - 768 017
India
| How to cite this article: Padhi T, Mohanty P, Jena S, Sirka C S, Mishra S. Clinicoepidemiological profile of 590 cases of beetle dermatitis in western Orissa. Indian J Dermatol Venereol Leprol 2007;73:333-335 |
Abstract
Background: Beetle dermatitis is a very common condition in western Orissa. It is often misdiagnosed and causes significant morbidity among the rural population. Aim: This study was conducted to determine the epidemiological and clinical profile of beetle dermatitis in western Orissa. Methods: All clinically diagnosed cases of beetle dermatitis were included in the study. Detailed history was taken and thorough clinical examination was conducted in all the cases. One urban and three rural localities were visited regularly to detect the epidemiological trends of the disorder. Results: A total of 590 cases were studied: 486 males and 104 females. The age of the patients ranged from 2 to 65 years. Forty-four percent of the patients belonged to the pediatric age group. Majority of the cases (85%) presented during the months of March to July, indicating a distinct seasonal trend. The disorder was prevalent in the localities nearer to paddy and sugarcane fields and grasslands with stagnant water. The clinical lesions included papules, erosions, crusted lesions, urticarial plaques and vesiculobullous lesions. Distribution was mainly linear, but kissing lesions were also observed. Head, neck and upper extremities were the most commonly involved sites. Lymphadenopathy and systemic features such as fever and malaise were observed in 24% and 15% of the cases, respectively. Conclusion: Beetle dermatitis should be included in the differential diagnosis of the acute onset of vesiculobullous lesions in the endemic areas.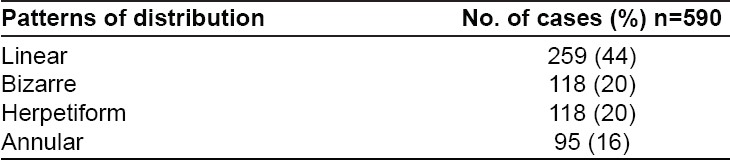
Introduction
Beetle dermatitis is a specific form of acute irritant contact dermatitis caused by a vesicant chemical present in the body fluid of the insects belonging to the order Coleoptera. [1] The disease is characterized by sudden onset of erythematous, vesiculobullous lesions on the exposed body parts associated with stinging or burning. The dermatitis is most frequently seen in regions with a warm, tropical climate. Most frequently, the contact between the skin and the body fluid occurs due to the crushing of the insect on the skin. [2]
This condition is fairly common in the western part of Orissa where paddy and sugarcane are the main agricultural products. However, there is a lack of knowledge regarding the cause of this dermatosis among general population as well as medical professionals. Occurrence of these painful skin lesions leads to significant morbidity and loss of working days among the agricultural workers. There have been frequent reports of outbreak of beetle dermatitis in the residential schools throughout this region. This motivated us to undertake this study for a better understanding of the clinical and epidemiological profile of beetle dermatitis.
Methods
All the clinically diagnosed cases of beetle dermatitis, i.e., the patients who attended the dermatology out-patient department of VSS Medical College, Burla, Orissa between February 2003 and January 2007 were included in the study. A detailed history was taken for all the cases, including age, sex, locality (rural or urban), occupation, family history of similar skin lesions, seasonal variation, past episodes, lighting used (fluorescent or incandescent) and proximity of residence to paddy or sugarcane field. Thorough clinical examination was done to determine the site of involvement, morphology of lesions (macule, papule, vesicle/bulla), pattern of lesion (linear, herpetiform, kissing), residual postinflammatory pigmentary changes (hypo- or hyperpigmentation), mucosal involvement and systemic features (fever or lymphadenopathy).
Repeated attempts were made to collect the specimens of insects near fluorescent lights in residential schools, hostels and other localities where this condition was particularly prevalent. Insect specimens were collected from the polythene bags that were tied to the light sources. Consultation was sought from the Department of Entomology, Institute of Agricultural Sciences, Banaras Hindu University regarding the identification of the species and specific preventive measures.
Results
A total of 590 clinically diagnosed cases of beetle dermatitis were studied: 486 males and 104 females. Age of the patients ranged from 2 to 65 years. 44% of the patients were in the pediatric age group. The rural-urban population ratio was 2.6:1. Majority of the cases (85%) were reported between the months of March and July. Almost all the rural patients (92%) and some of the urban patients (18%) gave a history of residing nearby the paddy or sugarcane fields. Fluorescent lights were used at night by 53% of the affected patients.
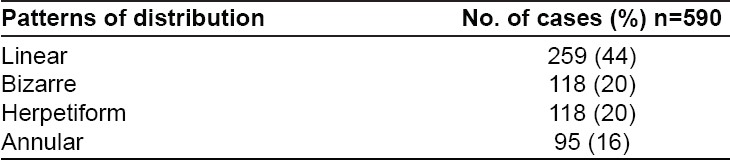
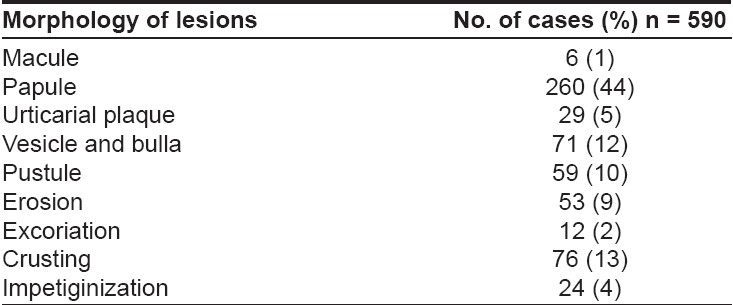
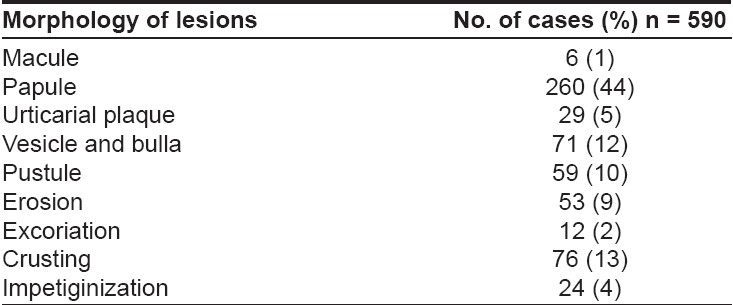
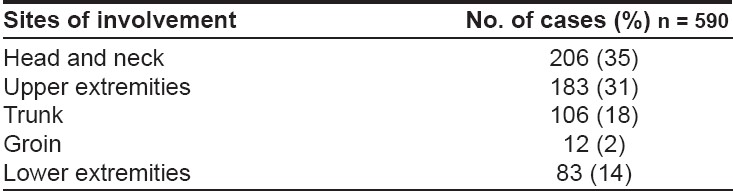
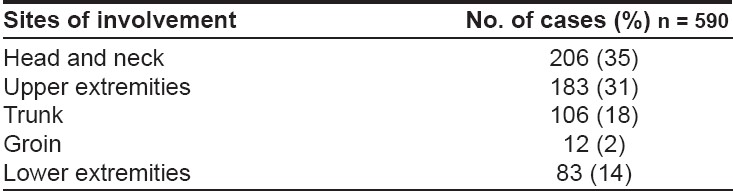
Head and neck were the most commonly affected sites [Table - 1]. There are various morphological patterns [Table - 2] and distributions of skin lesions of beetle dermatitis [Table - 3]. Kissing lesions were observed in 22% of the cases. Burning (68%) and itching (28%) were the major presenting symptoms. The average duration of symptoms was 11 days. Postinflammatory hyperpigmentation was observed in half of the cases (51%) and some of the lesions healed with hypopigmentation (18%). Mucosal involvement in the form of keratoconjunctivitis and balanitis was observed very rarely (5 cases each). Lymphadenopathy and systemic features such as fever and malaise were observed in 24% and 15% cases, respectively.
In almost all the cases, skin lesions were noticed by the patients in the morning. They began as a linear or irregular area of erythema associated with variable degree of itching and burning sensations. Within a day, vesicles appeared over the erythematous area, ruptured within few days forming erosions or crusting or developing secondary infection. We could not identify a single species consistently from the specimen of insects collected. However, in majority of the samples, the Mylabris species ( Mylabris phalerata and Mylabris pustulata ) were identified.
Discussion
Beetles are a group of insects belonging to the order Coleoptera . There are three families, e.g., Oedemeridae , Meloidae and Staphylinidae , with more than 370,000 species. [3] The dermatitis is caused by a vesicant chemical contained in the body fluids of the beetles. The chemical in the body of both Oedemeridae and Meloidae is cantharidin. [3] The third group of blister beetles belongs to the genus Paederus (family Staphylinidae ). This genus contains a different vesicant chemical, pederin. [3] Hence, the clinicopathological picture produced by this group of beetles is different. If the causative species is Dermestes , allergic contact-dermatitis-like features may be present. The irritant properties of the larval hairs of this species cause the so-called "carpet beetle dermatitis." [4]
Clinically, this condition mimics a host of other dermatoses: herpes simplex, herpes zoster, phytophotodermatitis, contact dermatitis and impetigo. There is no definitive test to confirm the diagnosis; however, a thorough history and clinical examination is nearly always helpful. Various geographic and climatic factors such as deforestation and El-Nino can result in outbreaks. [5]
Beetle dermatitis may affect any age group as was true for our series of patients. The male preponderance observed in this study could be related to the occupational exposure and gender-based variation in the health-seeking behavior among the Indian population. Most of the patients had come from rural areas that can be related to the natural habitat of these insects, i.e., close to farm lands and moist areas. [2] Although controversial, these beetles may also feed on agricultural pests. However, the results of the study by Handa et al. [6] were contradictory to this postulation. The seasonal variation observed in our study is in accordance with other studies in India and Turkey; [6],[7] however, the peak time for the occurrence of beetle dermatitis in Iran and Guinea is in the month of September. Habitat specificity and rainfall pattern could be responsible for this variation. [5] Beetles are attracted towards neon and fluorescent light sources, and this finding has been corroborated in the study by Zargari et al . [8]
The clinical picture is very characteristic. The lesions are linear or superimposed (kissing lesions) vesicles on adjacent surfaces such as the flexor aspects of knee or elbow. The acute vesicular lesions undergo crusting within a few days and heal completely in 10-12 days, with a transient postinflammatory hypo- or hyperpigmentation.
The exposed body parts such as head, neck and upper extremities are the most commonly affected sites as observed in our study. Other Indian studies and those from Iran and Peru also had similar findings. [5],[6],[8],[9] Very few workers have studied systemic associations of this condition. Todd et al . [10] reported a series of patients with beetle dermatitis, and from these patients, four had to be hospitalized for extensive ulcerations and exfoliative dermatitis. There are reports of vasculitis like eruptions, cervical lymphadenopathy and nodular interstitial infiltration of the lungs in association with this condition. [11]
In the present study, we failed to identify a single species consistently as the causative agent. However, most of the species isolated were Mylabris phalerata and Mylabris pustulata . The other species of beetles collected were of no dermatological significance. This is in sharp contrast with the findings of other Indian studies where beetles belonging to genus Paederus were the main causative agents. This could be due to the difference in the habitat of the beetles, as Mylabris is specifically found in eastern India.
Although rarely fatal, an outbreak of beetle dermatitis has often forced groups of people to migrate to safer areas. [10] Various preventive measures have been discussed by Singh and Ali. [2] In addition, simple measures such as changing the light source (fluorescent to incandescent), using kerosene or petrol to kill the larvae in stagnant water, and spraying appropriate pesticides particularly in the breeding season are often helpful. General physicians in the endemic areas should be made aware of this condition and its management.
Acknowledgements
We offer our sincere thanks to Dr. Harsh Nath Singh, Emeritus Scientist and Ajit Kumar Research Scholar, Department of Entomology, Institute of Agricultural Sciences, Banaras Hindu University, Banaras, India
| 1. |
Banney LA, Wood DJ, Francis GD. Whiplash rove beetle dermatitis in central Queensland. Australas J Dermatol 2000;41:162-7.
[Google Scholar]
|
| 2. |
Singh G, Yusuf Ali S. Paedrus Dermatitis. Indian J Dermatol Venereol Leprol 2007;73:13-5.
[Google Scholar]
|
| 3. |
Nicholls DS, Christmas TI, Greig DE. Oedemerid blister beetle dermatosis: A review. J Am Acad Dermatol 1990;22:815-9.
[Google Scholar]
|
| 4. |
Southcott RV. Injuries from Coleoptera . Med J Aust 1989;151:654-9.
[Google Scholar]
|
| 5. |
Alva-Davalos V, Laguna-Torres VA, Huaman A, Olivos R, Chavez M, Garcia C, et al . Epidemic dermatitis by Paederus irritans in Piura, Peru at 1999, related to El Nino phenomenon. Rev Soc Bras Med Trop 2002;35:23-8.
[Google Scholar]
|
| 6. |
Handa F, Sharma P, Gupta S. Beetle Dermatitis in Punjab (a study of 77 cases). Indian J Dermatol Venereol Leprol 1985;51:208-12.
[Google Scholar]
|
| 7. |
Uslular C, Kavukcu H, Alptekin D, Acar MA, Denli YG, Memisioglu HR, et al . An epidemicity of Paederus species in Cukurova region. Cutis 2002;69:277-9.
[Google Scholar]
|
| 8. |
Zargari O, Kimyai-Asadi A, Fathalikhani F, Panahi M. Paederus dermatitis in northern Iran: A report of 156 cases. Int J Dermatol 2003;42:608-12.
[Google Scholar]
|
| 9. |
Kalla G, Batra A. Blister beetle dermatitis. Indian J Dermatol Venereol Leprol 1996;62:267-8.
[Google Scholar]
|
| 10. |
Todd RE, Guthridge SL, Montgomery BL. Evacuation of an Aboriginal community in response to an outbreak of blistering dermatitis induced by a beetle ( Paederus australis ). Med J Aust 1996;164:238-40.
[Google Scholar]
|
| 11. |
Ramachandran S, Hern J, Almeyda J, Main J, Patel KS. Contact dermatitis with cervical lymphadenopathy following exposure to the hide beetle, Dermestes peruvianus. Br J Dermatol 1997;136:943-5.
[Google Scholar]
|
Fulltext Views
2,848
PDF downloads
2,693





