Translate this page into:
Clown nose: A marker for lung carcinoma
Corresponding author: Dr. Sonali Gupta, Junior Resident, Department of Dermatology, STD & Leprosy, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India. sonaliagrwal31011997@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gupta S, Gupta P, Singh P, Asati DP. Clown nose: A marker for lung carcinoma. Indian J Dermatol Venereol Leprol 2023;89:792
Dear Editor,
Skin is an uncommon site for metastasis from solid primary tumours, accounting for 0.7% of all reported metastases. The site of primary tumor for cutaneous metastases correlates with the most common primary cancer in each gender. Cutaneous metastases are often a late sign of internal malignancy and are poor prognostic indicators. Lung malignancy metastasises to the skin in 1–12% of cases and these metastases may present prior to, or synchronously with, the diagnosis of the primary tumour.1 One rare morphology of such metastases is “clown nose-like lesions” and a literature search revealed 12 reported cases with clown nose-like lesions secondary to squamous cell carcinoma of the lung. Here, we report a similar presentation with cutaneous nasal tip metastasis from lung carcinoma.
A 55-year-old male, who used to smoke for a long time, was admitted to our hospital with complaints of persistent cough and white sputum for the past 2 months with few episodes of hemoptysis in last one week. This was associated with loss of weight and appetite. A referral was received for a single hyperpigmented crusted plaque over the tip of his nose of 1-year duration. He had no other significant medical or family history.
On admission, his vitals were stable and chest auscultation revealed reduced left sided air entry. A single well defined non-tender hyperpigmented crusted plaque of size around 3 × 2 cm with an erythematous periphery studded with pinpoint discrete pustules was seen over the tip of nose extending into the internal nares [Figure 1]. After the removal of adherent crusts [Figure 2a], dermoscopy was done, which showed yellow-white homogenous areas with patulous follicular openings in the centre, while the periphery of the lesion showed multiple glomerular vessels [Figure 2b].

- Well-defined non-tender hyperpigmented crusted plaque

- The image is on removal of crust before dermoscopy
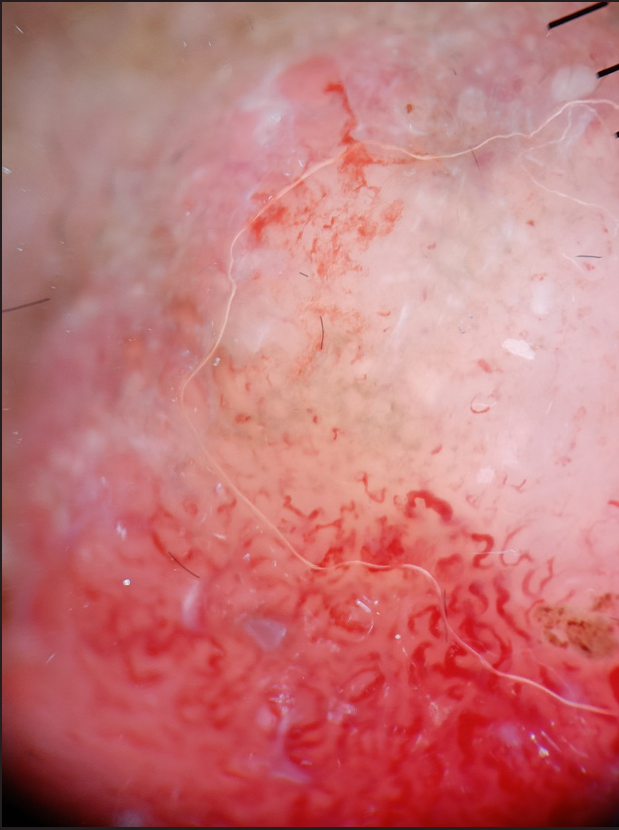
- With patulous follicular openings with multiple linear serpentine vessels
The laboratory investigations were normal apart from mild leucocytosis (12,280 cells/cumm). Chest X-ray revealed left-sided hydropneumothorax [Figure 3a], for which an intercostal drainage tube was placed. Pleural fluid analysis showed purulent effusion with total cells 3250 cells/cumm, 85% neutrophils and low adenosine deaminase (21.73 U/L). Pleural fluid cytology for malignant cells and sputum cartridge-based nucleic acid amplification test were negative. Bronchoscopy revealed a growth in the left main bronchus from which an endobronchial biopsy was taken, which showed non-small cell lung carcinoma, histologically favouring adenosquamous carcinoma.
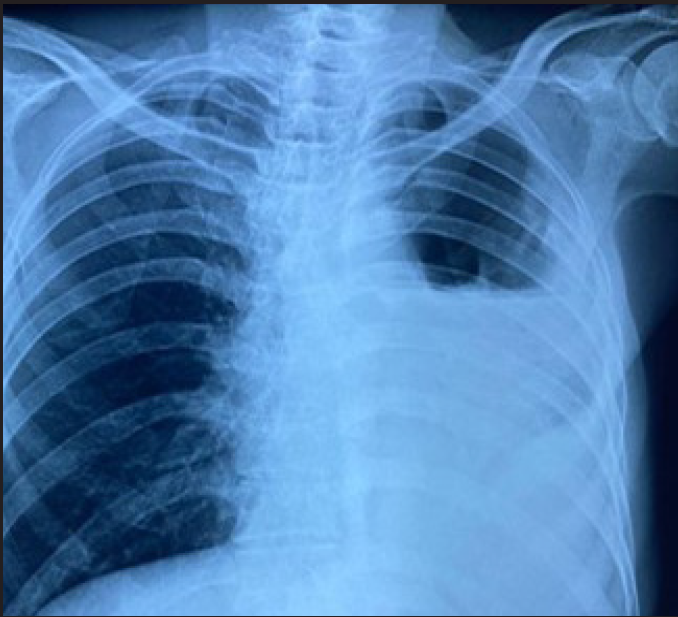
- Chest radiograph showing left-sided hydropneumothorax
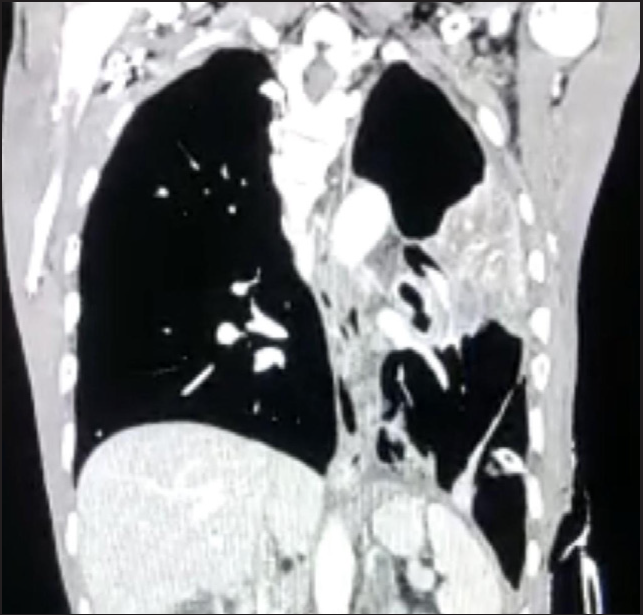
- Chest radiograph showing ill-defined heterogeneously enhancing infiltrative soft tissue lesion in the left peri-hilar region
Contrast-enhanced computed tomography (CECT) of the chest and abdomen [Figure 3b] showed a heterogeneously enhancing infiltrative lesion in the left peri-hilar region with collapsed left upper lobe and contralateral metastasis to the right upper lobe. Mediastinal lymphadenopathy with skeletal and bilateral adrenal metastases was present.
A punch biopsy from the plaque over the tip of the nose showed irregular acanthosis with underlying reticular dermis infiltrated with invasive tumour-arranged nests, cords and trabeculae [Figure 4a–4c]. Tumour cells were polygonal in shape with moderate nuclear pleomorphism, hyperchromatic nuclei, prominent nucleoli and moderate cell keratinisation. Tumour cells showed Ber-Ep4 membranous positivity. These findings were consistent with squamous cell carcinoma.
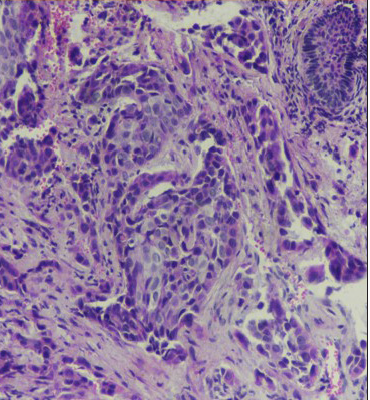
- Tumour cells with focal keratinization in the dermis (H & E stain, ×100)
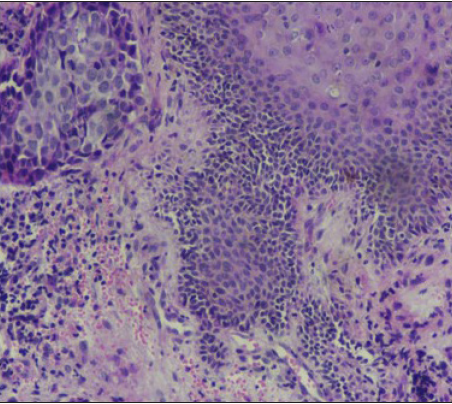
- Tumour not extending into the overlying dermis (H & E stain, ×100)
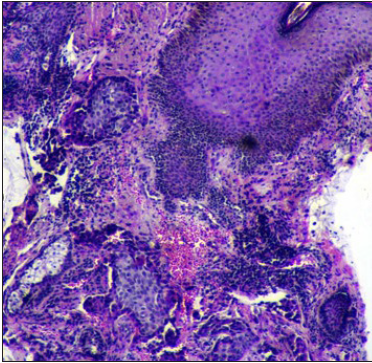
- Tumour cells and islands in dermis (H & E stain, ×40)
The patient was diagnosed to have non-small cell carcinoma stage IVB (T4N3M1c) and was planned for chemotherapy with paclitaxel and carboplatin. Patient received first cycle with no adverse events and is being followed up regularly.
Skin remains an uncommon site of metastatic disease, with an incidence of 0.7% of all patients with cancer. Cutaneous dissemination of visceral malignancies usually occurs in the later stages of the disease. However, occasionally they may be the first indication of clinically silent visceral malignancies. Melanoma has been reported to be the most common cancer to metastasize to the skin in men (32% of all cases), whereas breast cancer is the commonest in women (69% of all cases).
Compared to other internal malignancies, lung cancer is the earliest to develop skin metastases after the initial diagnosis. Cutaneous metastases secondary to lung cancers are relatively common in men, with an incidence of 1% of cases. All histologic types of lung cancer have been associated with the development of skin metastases. It is debatable whether adenocarcinoma or large cell carcinoma has a greater tendency to metastasise to cutaneous sites. However, small cell carcinoma of the lung rarely extends to the skin.
A number of cancers demonstrate a localization preference to the region of skin affected eg. lung cancer to the supradiaphragmatic (mostly chest) and colorectal cancers to the infra-diaphragmatic (abdominal) skin regions.2 In addition, cancer of the upper lobes of the lungs has a greater tendency to metastasize to the skin.3 These findings may be especially relevant and useful in patients where skin metastasis is the first indication of malignancy. Cutaneous metastases in the facial regions are reported to occur in less than 0.5% of patients with metastatic cancer4 and are often overlooked.
Clinical presentations of skin metastases are highly variable, nonspecific, and subtle and are easily misdiagnosed. Typical features include single or multiple variably sized painless nodules of firm, hard or elastic consistency that develop within a short time. Solitary or multiple lesions with ulcerative or exudative features have also been described. They may rarely appear as solitary or grouped papules, plaque-like, zosteriform, erysipelas-like or as cicatricial alopecia on the scalp.
Clown nose is an uncommon presentation of skin metastasis to the tip of the nose. It presents as a firm to rubbery blue-to-red bulge with or without ulceration, resembling the red nose of a clown. Nasal tip metastases were reported in around 20 cases secondary to internal malignancies and rhabdomyosarcoma, out of which 12 were from malignancies of the lung. Other internal malignancies included carcinomas of the thyroid, hypopharynx, oesophagus, chordoma and leukaemia. Most of the patients were elderly males with an average age of around 50 years. The lesion lasted from several weeks to one year with a mean duration of 3 months. Baston suggested that tumour cells could be transported to the nose by the pulmonary vascular and lymphatic circulation and the valveless vertebral venous plexus. Clown nose-like lesions appear for a very short period of time prior to or synchronously with malignancy. As the nose is the most noticeable area of the face, patients usually present to dermatologists with or without systemic symptoms and may be misdiagnosed as primary skin diseases including rosacea. Detailed history, histopathology and systemic examination are necessary, especially in the elderly individuals.
Recently the term clown nose-like lesion was described as a clue for genetic syndromes, such as tricho-rhino-phalangeal syndrome, Hernandez syndrome, tuberous sclerosis, familial trichoepitheliomas etc. Such patients develop nasal manifestations at a younger age with a slight female predilection. A high index of suspicion for such syndromes must be kept in patients with intellectual disabilities, sparse hair and a predisposition for malignancies. Some of the primary nasal diseases that can present as clown nose include leishmaniasis, rosacea, blastomycosis, superficial and deep skin mycoses and keratoacanthoma.
Skin metastases are usually indicative of an aggressive and poorly differentiated cancer and thus are associated with a poor prognosis and short survival. Reports suggest that the median survival time after the appearance of skin metastasis is about 8 months.5
A high index of suspicion is thus necessary for early detection of skin metastasis. Close inspection of skin lesions and histopathological evaluation is necessary in patients with a history of malignancy presenting with atypical cutaneous lesions. This could allow early initiation of treatment before widespread visceral metastases occur.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Tumor type-specific and skin region-selective metastasis of human cancers: Another example of the “seed and soil” hypothesis. Cancer metastasis reviews.. 2013;32
- [CrossRef] [PubMed] [Google Scholar]
- Facial skin metastasis due to small-cell lung cancer: a case report. J Med Case Rep.. 2009;3:32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous metastases from solid neoplasms in the 21st century: a retrospective study from a Portuguese tertiary care center. J Eur Acad Dermatol Venereol.. 2020;34:1218-1224.
- [CrossRef] [PubMed] [Google Scholar]





