Translate this page into:
Combined biological therapy with dupilumab and secukinumab for coexisting bullous pemphigoid and psoriasis
Corresponding author: Dr. Furen Zhang, Department of Dermatology, Hospital for Skin Diseases, Shandong First Medical University, Shandong Province, Jinan, Shandong, China. zhangfuren@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Cao S, Yang B, Liu Y, Liu H, Zhang F. Combined biological therapy with dupilumab and secukinumab for coexisting bullous pemphigoid and psoriasis. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1291_2024
Dear Editor,
Bullous pemphigoid (BP) is an autoimmune bullous disease that predominantly affects the elderly. It is characterised by pruritic erythema and blisters. Studies have shown that dupilumab may be an effective and safe alternative for patients with BP1 which is the most common type of autoimmune bullous disease (AIBD) associated with psoriasis.2 However, optimal management strategies for patients with coexisting BP and psoriasis are limited. Here, we report a case of a male patient with confirmed coexisting BP and psoriasis who was successfully treated using a combination of dupilumab and secukinumab.
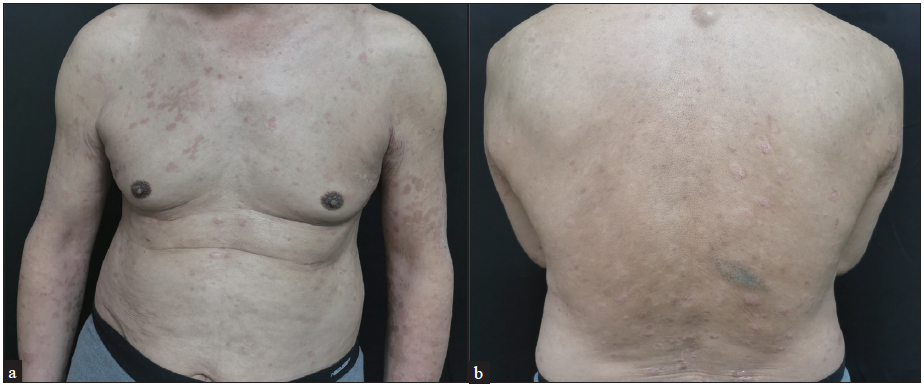
A 75-year-old man presented with a history of scaly plaques noticed since one month and blistering since 15 days. Physical examination revealed tense blisters on his chest and limbs, as well as scaly red papules and plaques on his chest and back [Figures 1a and 1b]. He was previously diagnosed with coronary heart disease and hypertension. The patient was treated with apremilast at a daily dose of 60 mg for 2-weeks due to the initial suspicion of psoriasis. However, the efficacy of the said treatment was poor. Laboratory abnormalities included the elevation of eosinophil levels (1.73×109/L), an elevated C-reactive protein level of 31.53 mg/L and an IgE level of 180 kU/L. Enzyme-linked immunosorbent assay (ELISA) testing yielded a positive result for BP180 with a value of 121.78 IU/mL. The skin biopsy from a representative psoriatic lesion demonstrated epidermal hyperkeratosis, neutrophilic infiltration, thinning of the granular layer and regular thickening of the spiny layer [Figure 2a]. A skin biopsy of the blister lesion showed subepidermal blisters with neutrophils and eosinophils infiltrating the blister area [Figure 2b]. Direct immunofluorescence studies from the blister lesion revealed IgG and C3 deposits along the basement membrane zone [Figure 2c]. The coexistence of BP and psoriasis was confirmed.
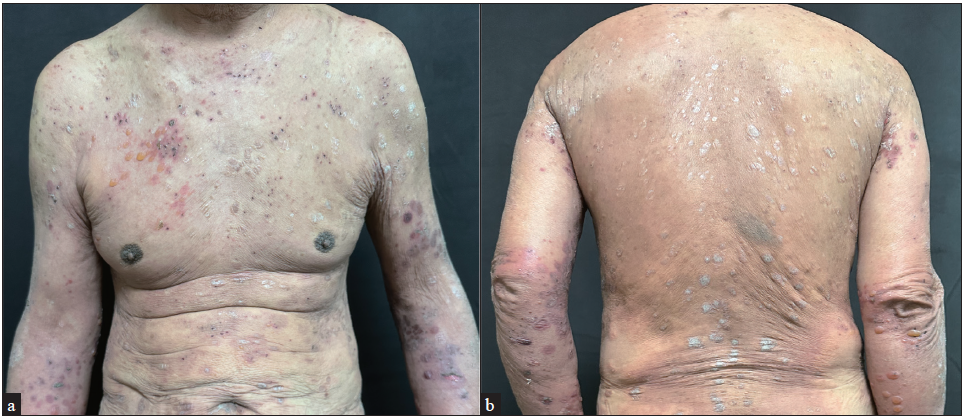
- Tense blisters and erythematous scaly lesions over trunk and back.
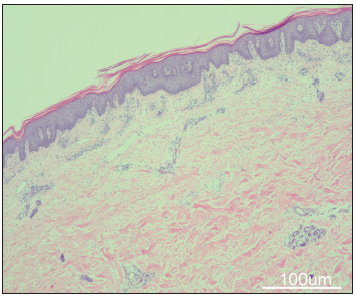
- Skin biopsy of a psoriatic lesion showed epidermal hyperkeratosis, neutrophilic infiltration, thinning of the granular layer and regular thickening of the spiny layer (Haematoxylin-eosin, 100x, scale bar, 100 µm).
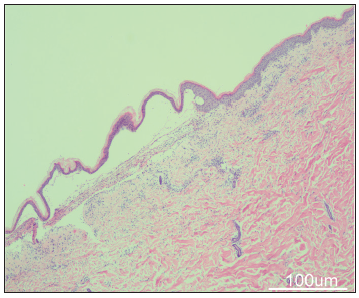
- Skin biopsy of blister lesions showed subepidermal blisters with neutrophils and eosinophils infiltrating the blister area (Haematoxylin-eosin, 40x, scale bar, 100 µm).
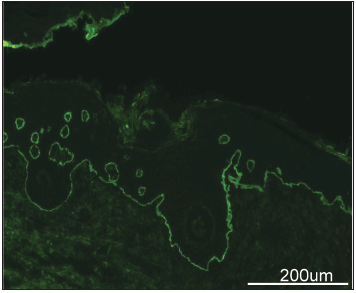
- Direct immunofluorescence imaging of blister lesions showed IgG and C3 deposits along the basement membrane zone (200x, scale bar, 200 µm).
Considering the efficacy and safety of dupilumab for treating BP, dupilumab monotherapy was initiated with a first dose of 600 mg, followed by 300 mg every 2 weeks due to the severity of BP. The blisters improved by more than 50% after 1 week. Secukinumab (300 mg weekly) was also administered for the treatment of psoriasis 1 week after the dupilumab injection. The lesions improved after 2 weeks [Figures 3a and 3b] and were almost completely resolved after 6 weeks [Figures 3c and 3d]. Both BP and psoriasis were well controlled at a 5-month follow-up visit and no side effects had occurred during the treatment.

- Partial improvement in skin lesions of the trunk and back after 2 weeks of treatment.
- Complete resolution of skin lesions of the trunk and back after 6-weeks of treatment.
Coexisting BP and psoriasis, two immune-related skin diseases, was first described in 1976.2 BP is the most common type of AIBD found in association with psoriasis. In a combined analysis of four case-control studies, a notably higher incidence of psoriasis was observed among individuals with BP compared to that in the control group (2.6% vs. 1.1%, odds ratio: 2.5).2 Generally, the onset of BP in individuals with psoriasis occurs after psoriasis treatment, especially phototherapy. The mechanism underlying the concurrence of BP and psoriasis remains unclear. It is postulated that chronic disruption of the basement membrane layer in psoriasis may lead to altered antigenicity and subsequent autoantibody production which explains why most cases of BP occur after psoriasis.3 Recently, it was suggested that BP and psoriasis may share a common pathogenetic pathway based on the elevated interleukin (IL)-23 and IL-17 levels in lesional skin and serum of BP patients.3
A bidirectional association exists between BP and psoriasis. However, opinions on managing their coexistence, especially in the elderly, lack consensus. For mild cases, topical corticosteroids are considered safe and effective. For severe cases, immunosuppressants, such as methotrexate, remain the preferred choice, followed by cyclosporine and azathioprine. Novel biologics, such as IL-17A inhibitors show promise in treating both conditions. There are reports documenting the efficacy of secukinumab therapy in the concurrent treatment of psoriasis and BP.4.5 However, paradoxical reactions have also been reported, where some BP patients have experienced relapses after using IL-17A inhibitors for psoriasis.5,6 Further investigations are warranted to clarify the correlation between IL-17 inhibitors and BP. Although some researchers have reported that treatment with janus kinase inhibitors is effective, its use in the elderly is limited due to side effects.7 According to the current reports, there have been no studies investigating the prognosis of BP in combination with psoriasis. However, the prognosis for most patients is favourable, as their condition can be quickly controlled with treatment. It is recommended that the first step for treating patients with BP with co-existent psoriasis should involve identifying and eliminating the underlying triggers. Concurrently, it is essential to assess the severity of the condition and select an appropriate therapeutic regimen accordingly. Regardless of the chosen treatment approach, caution should be exercised to prevent the recurrence of both BP and psoriasis.
To the best of our knowledge, there have been no reports of successful BP treatments in patients with psoriasis using a combination of dupilumab and secukinumab. The present case demonstrates the potential clinical efficacy and safety of this combination therapy for treating coexisting BP and psoriasis. Further high-quality studies are needed to establish new treatment strategies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Evaluation of dupilumab in patients with bullous pemphigoid. JAMA Dermatol. 2023;159(9)::953-60.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association between bullous pemphigoid and psoriasis: systematicSystematic review and meta-analysis of case-control studies. Australas J Dermatol. 2019;60:23-8.
- [CrossRef] [PubMed] [Google Scholar]
- A successful treatment with ustekinumab in a case of relapsing bullous pemphigoid associated with psoriasis. J Eur Acad Dermatol Venereol. 2017;31(5)::e228-e230.
- [CrossRef] [PubMed] [Google Scholar]
- Successful secukinumab treatment of active bullous pemphigoid and chronic severe psoriasis: a case report. Australas J Dermatol. 2022;63(2)::e155-8.
- [CrossRef] [PubMed] [Google Scholar]
- Secukinumab decreased circulating anti-BP180-NC16a autoantibodies in a patient with coexisting psoriasis vulgaris and bullous pemphigoid. J Dermatol. 2019;46(6)::e216-7.
- [CrossRef] [PubMed] [Google Scholar]
- Two cases with bullous pemphigoid relapsed after using interleukin-17A inhibitors for psoriasis: A paradoxical reaction. J Dermatol. 2023;50(7)::956-9.
- [CrossRef] [PubMed] [Google Scholar]
- Concurrent bullous pemphigoid and plaque psoriasis successfully treated with Janus kinase inhibitor baricitinib. Dermatol Ther. 2022;35(10)::e15754.
- [CrossRef] [PubMed] [Google Scholar]





