Translate this page into:
Comparative efficacy of continuous and pulse dose terbinafine regimes in toenail dermatophytosis: A randomized double-blind trial
2 Department of Microbiology, University College of Medical Sciences and GTB Hospital, University of Delhi, Delhi, India
Correspondence Address:
Archana Singal
B-14, Law Apartments, Karkardooma, Delhi - 110 092
India
| How to cite this article: Yadav P, Singal A, Pandhi D, Das S. Comparative efficacy of continuous and pulse dose terbinafine regimes in toenail dermatophytosis: A randomized double-blind trial. Indian J Dermatol Venereol Leprol 2015;81:363-369 |
Abstract
Introduction: Dermatophytes are the most frequently implicated agents in toenail onychomycosis and oral terbinafine has shown the best cure rates in this condition. The pharmacokinetics of terbinafine favors its efficacy in pulse dosing. Objectives: To compare the efficacy of terbinafine in continuous and pulse dosing schedules in the treatment of toenail dermatophytosis. Methods: Seventy-six patients of potassium hydroxide (KOH) and culture positive dermatophyte toenail onychomycosis were randomly allocated to two treatment groups receiving either continuous terbinafine 250 mg daily for 12 weeks or 3 pulses of terbinafine (each of 500mg daily for a week) repeated every 4 weeks. Patients were followed up at 4, 8 and12 weeks during treatment and post-treatment at 24 weeks. At each visit, a KOH mount and culture were performed. In each patient, improvement in a target nail was assessed using a clinical score; total scores for all nails and global assessments by physician and patient were also recorded. Mycological, clinical and complete cure rates, clinical effectivity and treatment failure rates were then compared. Results: The declines in target nail and total scores from baseline were significant at each follow-up visit in both the treatment groups. However, the inter-group difference was statistically insignificant. The same was true for global assessment indices, clinical effectivity as well as clinical, mycological, and complete cure rates. Limitations: The short follow-up in our study may have led to lower cure rates being recorded. Conclusion: Terbinafine in pulse dosing is as effective as continuous dosing in the treatment of dermatophyte toenail onychomycosis.INTRODUCTION
The term onychomycosis refers to nail infection by dermatophyte fungi, non-dermatophyte fungi or yeast. It is the most common nail disease accounting for 50% of all onychopathies. [1] The reported prevalence of onychomycosis varies from 2% to 8% [2] worldwide and from 0.5% to 5% in India. [3] Dermatophytes are the most frequently implicated causative agents with Trichophyton rubrum and Trichophyton mentagrophytes var. interdigitale being responsible for nearly 90% of toenail and at least 50% of fingernail onychomycosis. [4]
Onychomycosis needs to be treated because of long-term morbidity and for aesthetic reasons, but treatment is challenging. Topical treatments such as ciclopirox nail lacquer have a limited role, mainly as adjuvants. Nail avulsion has significant morbidity. Older systemic medications like griseofulvin and ketoconazole are associated with low cure rates and prolonged treatment durations, and a potential for side effects and drug interactions. [5] On the other hand, newer oral antifungals such as itraconazole and terbinafine have higher cure rates, shorter treatment periods and fever adverse reactions. [5]
Studies have concluded that the fungicidal allylamine, terbinafine is the most effective medication for dermatophyte toenail onychomycosis with cure rates of 87-88% [5],[6],[7] and low relapse rates. The drug is concentrated in hair, nails and skin leading to a reservoir effect. It is safe in children, the elderly [8],[9] as well as in high-risk populations including diabetics, [10] HIV and other immunocompromised patients. [11]
Terbinafine in a continuous schedule of 250 mg/day for 12 weeks for toenail infection, and 6 weeks for fingernail infection has been considered the regimen of choice, but this is expensive. Oral terbinafine in a pulse regimen (500 mg/day for 1 week every month) for 3 months halves the cost of medication and has shown promising results in some studies, with mycological cure rates of 74-80%. [12],[13],[14] However, only a few studies have compared daily and pulse terbinafine in the treatment of toenail onychomycosis, finding similar response rates with one study pointing to the contrary. [15]
METHODS
The study was conducted at the departments of dermatology and STD and microbiology of the University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi and was approved by the institutional ethical committee.
To determine sample size, the cure rates from the study of Pavlotsky et al[14] were considered for the outcome measure (complete cure rates of 34% in the continuous treatment group vs. 47% in the pulse group). Taking the level of significance as 5% and the power of the study as 80%, the minimum sample size required in each arm was 23. However, since the post-treatment follow-up was to be for 3 months, 38 patients were included in each arm to compensate for the expected loss to follow-up. Patients of untreated toenail onychomycosis with positive potassium hydroxide (KOH) preparations and cultures were recruited between January 2010 and July 2011. Patients were excluded if they had taken oral antifungal therapy in the previous 3 months or used topical antifungals in the previous 1 month. Other exclusion criteria were: severe systemic disease, pregnancy or lactation and nail disease attributable to other dermatoses. Informed consent was obtained from all patients prior to their enrolment.
Details of duration and progression of the disease, treatment taken, occupation, history of trauma and any co-morbidities were obtained in all patients, and general physical and systemic examinations were carried out. The skin and fingernails were also examined for evidence of fungal infection. The number of nails involved and the type and extent of involvement were recorded. The most affected toenail (preferably of the great, 2 nd or 3 rd toes) was selected as the target nail. The length of the healthy part of the target nail was measured in millimeters. Severity of nail involvement was assessed on a 4-point scale (0, 1, 2 and 3) on each of three parameters: onycholysis, subungual hyperkeratosis, and paronychial inflammation. The three scores of the target nail were added to get a clinical assessment score (CAS) (maximum score, 9 per nail). A similar scoring was done for all the toenails except for the 5 th toenails (maximum, 8 toenails and score of 72) and added to get a total clinical assessment score. Baseline investigations including complete blood counts, livers and kidney function tests were done in all patients. Photographic documentation was done at baseline and at every follow up visit.
Eligible patients were randomized using computer-generated random numbers into 2 groups. Patients in one group received oral terbinafine, 250 mg daily for 12 weeks (continuous treatment group) while those in the other group received terbinafine 250 mg twice daily for one week, to be repeated every 4 weeks for 12 weeks (pulse treatment group). To achieve blinding, patients in the continuous treatment group received an additional placebo tablet daily for the first week of every 4 weeks and patients in the pulse treatment group received a daily placebo tablet after this first week. The placebo was a multivitamin tablet identical to the terbinafine tablet in shape, size and color. Drugs were dispensed by a trained nurse for 4 weeks at a time, in precoded identical containers that had two tablets per day for the first week and a single daily tablet for the next 3 weeks. Neither investigator nor patient was aware of the regimen being administered.
Patients were followed up at 4, 8 and 12 weeks during treatment and once post-treatment, at 24 weeks. Target nail and total scores were recorded at each visit. Overall clinical improvement was also graded at every visit on a 4-point scale (global assessment index) both by the patient and physician as follows: <25% improvement: poor, 26-50%: average, 51-75%: good, and >75% improvement: excellent. Efficacy of treatment was assessed on the following parameters at 12 and 24 weeks:
- Clinical cure: Completely normal-appearing nail with no visible residual changes
- Mycological cure: Negative KOH microscopy and negative culture
- Complete cure: Both clinical and mycological cure
- Clinical effectivity: Increase in the length of normal nail of >3 mm or a >50% improvement in the global physician assessment index for the target nail at the end of treatment i.e. at 12 weeks. We used this as an additional parameter to determine early response since the relatively short follow-up period in our study could have led to lower cure rates than expected
- Treatment failure: Persistence of positive KOH/and/or culture, no clinical improvement (i.e. no increase in the length of normal nail) or clinical worsening at 12 and 24 weeks
- Relapse: Positive KOH preparation or culture, or clinical worsening at least 4 weeks after a negative KOH/culture or clinical improvement/cure had been achieved.
Compliance with treatment as well as tolerability and side effects of the drug were also assessed at each visit.
Statistical analysis
Intention-to-treat analysis was carried out with missing values calculated by the multiple computation method. Repeated measures analysis of variance (ANOVA) was done, followed by Tukey′s test at a 5% level of significance to compare the scores at different points of time within each group and also between the groups. Chi square/Fischer test was applied to compare the rates of clinical cure, mycological cure, complete cure and failure rates between the groups. A P < 0.05 was taken as significant. SSPS Version 17 statistical software was used for data analysis.
RESULTS
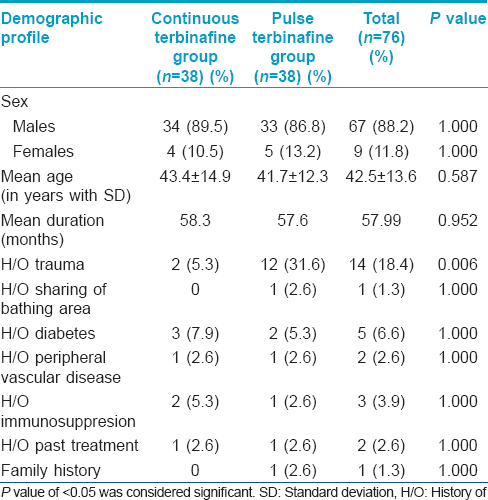
Seventy-six eligible patients (67 males and 9 females, mean age 42.51 ± 13.60 years) were included. The flow of participants in the study was as in [Figure - 1]. Baseline characteristics of the patients were similar in the two groups [Table - 1].
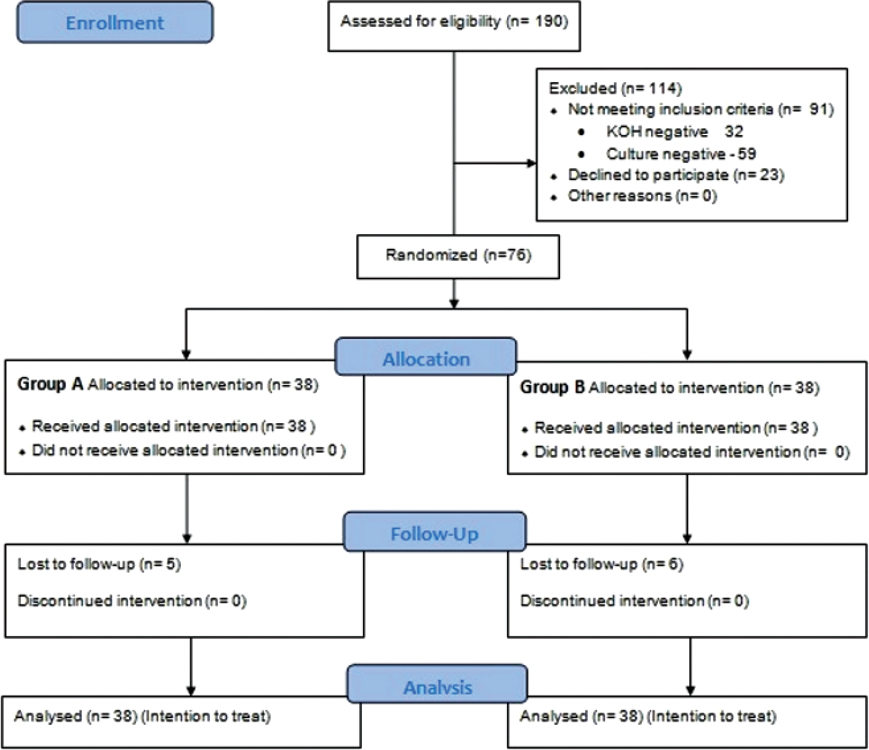 |
| Figure 1: Flow of patients through the study |
The mean clinical assessment score of the target nail in both the treatment groups declined at each follow-up visit [Table - 2]. In both groups, the mean declines from baseline in target nail and total scores were statistically significant and the scores had declined further at 24 weeks. However, there were no statistically significant differences in scores between the two groups at any follow-up visit. Fourteen (36.8%) and 10 (26.3%) patients in the continuous treatment and pulse groups respectively had global physician assessment index scores of good to excellent (>50% improvement) at 12 weeks with the difference not being statistically significant (P = 0.324). On the other hand, a statistically significant difference was observed in global patient assessment index score reductions, with 12 (31.6%) patients reportinga good to excellent response in the continuous treatment group as compared to 4 (10.5%) in the pulse group at 12 weeks (P = 0.024).

Clinical effectivity was achieved in 33 (86.8%) patients on continuous treatment as compared to 27 (71.1%) in the pulse group; this difference too was statistically not significant (P = 0.280) [Figure - 2] and [Figure - 3].
 |
| Figure 2: Pre-treatment and 12 weeks' post-treatment photograph of a patient from pulse terbinafine group |
 |
| Figure 3: Pre-treatment and 12 weeks' post-treatment photograph of a patient from continuous terbinafine group |
At 12 weeks, more patients in the continuous treatment group achieved mycological cure than in the pulse group [11 (28.9%) vs. 7 (18.4%), P = 0.280]. The difference in mycological cure rates was statistically notsignificant at 24 weeks as well [29 (76.3%) vs. 30 (78.9%), P = 0.783] [Figure - 4]. Differences in the KOH preparation and culture results were also not significant in the two groups at any follow-up visit [Table - 3].
 |
| Figure 4: Mycological, clinical, and complete cure rates of target nail in the two treatment groups |

At 12 weeks, clinical cure and complete cure of the target nail were achieved in only one patient (belonging to pulse terbinafine group), and none achieved clinical and complete cure of all nails. At 24 weeks, clinical cure of the target nail was achieved in 4 (10.5%) patients in the continuous treatment group and 5 (13.2%) in the pulse group, while the corresponding figures for complete cure of all nails were 3 (7.9%) and 2 (5.3%) respectively [Figure - 4].
Differences in mycological cure rates for the three causative fungal species were statistically not significant at 24 weeks [Table - 4]. Clinical effectivity at 12 weeks was also found to be independent of the causative species, being seen in 34 (72.3%) of 47, 22 (88.0%) of 25 and all 4 of the patients with onychomycosis caused by T. mentagrophytes, T. rubrum, and T. verrucosum respectively (P = 0.399).

At 12 weeks, 27 (71.1%) patients in the continuous treatment group and 31 (81.6%) in the pulse group were deemed treatment failures (P = 0.280), while at 24 weeks, the respective numbers were 9 (23.7%) and 8 (21.1%). No relapses were noted during the post-treatment follow-up period of 12 weeks.
Both treatment regimes were tolerated well. Only 8 (10.5%) of 76 patients (5 from the continuous group and 3 from the pulse terbinafine group) complained of mild gastric discomfort that stopped on taking the drug with meals, and it did not affect compliance. None of the patients developed any hematologic or biochemical abnormalities.
DISCUSSION
Clinical cure rates ranging from 54% to 76% have been shown with continuous terbinafine treatment in onychomycosis. [16],[18] One study with daily oral terbinafine for 12 weeks and post-treatment follow-up at 48 weeks found significant improvements (64.2% vs. 37.5%) in scores on a 4-point scale assessing hyperkeratosis, onycholysis and paronychial inflammation as compared to itraconazole. [16] Another assessed these features and nail brittleness on continuous terbinafine treatment of fingernail onychomycosis and again, showed significant reductions (5.8 vs. 0.9) in scores at 24 week follow up. [17]
A few studies have found that the alternative pulse regimen, which is in accordance with the pharmacokinetics of terbinafine in the nail, is also effective. [12],[13],[14] Our study corroborates the findings of some of these [Table - 5]. While one study demonstrated significantly higher cure rates with continuous rather than intermittent terbinafine (clinical cure in 44.6% vs. 29.3%, complete cure of all nails in 25.2% vs. 14.7%) at 18 months, [15] another yielded converse results (clinical cure in 35% vs. 53.5% respectively). [14] Likewise, no significant differences in mycological cure rates with continuous and pulse dose terbinafine (79-82%vs. 72-74%) were found by some investigators [12],[14] while others did find significant differences. [15] As mycological cure is achieved earlier than clinical cure, mycological cure rates in our study were similar to those in previous studies notwithstanding our shorter follow-up.Mycological cure rates and clinical effectivity in the two groups in our study were found to be independent of the causative dermatophyte species, an aspect not evaluated in previous studies.

The proportion of patients with a negative culture rose between 12 and 24 weeks in our study; this is attributable to fungicidal concentrations of terbinafine persisting in nails for several weeks after treatment. KOH positivity remained higher than culture positivity in both groups throughout follow-up, perhaps due to the persistence of non-viable fungal filaments. This is similar to a previously reported observation of higher KOH positivity (24%) than culture positivity (6%) amongst patients treated with continuous terbinafine. [7] A higher median response time to negative microscopy than to negative culture (18-24 weeks vs 12-18 weeks) has also been found. [6] It would therefore appear that the KOH preparation alone cannot be used as a marker of treatment response in onychomycosis.
A drawback of the present study was the relatively short follow-up which could have led to lower cure rates and higher failure rates than expected. Complete cure rates of 67% at 60 weeks and 46% at 72 weeks have been noted previously with continuous terbinafine therapy. [18],[19] Others have reported complete cure in 34% with continuous treatment and in 47% with intermittent treatment at 2 months post-treatment. [14] With a longer follow-up of 10 months, lower treatment failure rates (inability to achieve negative KOH microscopy and culture) of about 5% and 20% respectively with daily and pulse terbinafine have been reported. [13]
Relapse rates of 9% at around 72 weeks and 12% at 96 weeks′ follow-up have been reported in patients with toenail onychomycosis treated with continuous terbinafine, [6],[20] while pulse terbinafine treatment resulted in relapse rates of 7% at 48 weeks and 12% at 72 weeks in another study. [15] A recent study has shown mycological recurrence rates of 32% and 36% with continuous and intermittent terbinafine respectively, at 48 weeks′ follow up. [5] The absence of relapses in our study also may be due to the shorter post-treatment follow-up.
Side effects do not appear to be common with terbinafine. Out of 145 patients in one report, only 7 (5%) reported side effects (reversible loss of taste, reversible alteration in liver function tests, cold feet, severe allergic reaction, dizziness, shortness of breath, moderate acneiform eruption). [14] However , severe side effects have been reported in another study in 10 (6.8%) of 148 patients on continuous terbinafine and 8 (5.4%) of 149 patients on the pulsedosing schedule. [13]
To conclude, we found that oral terbinafine in a pulse dosing schedule was as efficacious as in a continuous daily schedule in the treatment of dermatophyte toenail onychomycosis, with both producing equivalent clinical, mycological, and complete cure rates. As with itraconazole, pulse terbinafine may therefore potentially be a treatment schedule of choice with significant cost reduction.
ACKNOWLEDGMENTS
Our sincere thanks to Ms. Rekha Sharma, staff nurse at the Department of Dermatology and STD, for dispensing the study drugs to the patients and to Dr. Rajeev Malhotra, PhD (Statistics) for assisting with the design of the study and for carrying out the statistical analysis.
| 1. |
Verma S, Hefferman MP. Superficial fungal infection. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Pallar AS, Leffell DJ, Editors. Fitzpatrick′s Dermatology in General Medicine, 7 th ed. New Delhi: McGraw Hill; 2008. p. 1817.
[Google Scholar]
|
| 2. |
Roberts DT. Prevalence of dermatophyteonychomycosis in the United Kingdom: Results of an omnibus survey. Br J Dermatol 1992;126 (Suppl. 39):23-7.
[Google Scholar]
|
| 3. |
Sobhanadri C, Rao DT, Babu KS. Clinical and mycological study of superficial fungal infections at Government General Hospital: Guntur and their response to treatment with Hamycin, Dermostatin and Dermamycin. Indian J Dermatol Venereol Leprol 1970;36:209-14.
[Google Scholar]
|
| 4. |
Elewski BE. Onychomycosis: Pathogenesis, diagnosis and management. Clin Microbiol Rev 1998;11:415-29.
[Google Scholar]
|
| 5. |
Gupta AK, Cooper EA, Paquet M. Recurrences of dermatophyte toenail onychomycosis during long-term follow-up after successful treatments with mono- and combined therapy of terbinafine and itraconazole. J Cutan Med Surg 2013;17:201-6.
[Google Scholar]
|
| 6. |
Drake LA, Shear NH, Arlette JP, Cloutier R, Danby FW, Elewski BE, et al. Oral terbinafine in the treatment of toenail onychomycosis: North American multicenter trial. J Am Acad Dermatol 1997;37:740-5.
[Google Scholar]
|
| 7. |
Watson A, Marley J, Ellis D, Williams T. Terbinafine in onychomycosis of the toenail: A novel treatment protocol. J Am Acad Dermatol 1995;33:775-9.
[Google Scholar]
|
| 8. |
Gupta AK, Konnikov N, Lynde CW. Single-blind, randomized, prospective study on terbinafine and itraconazole for treatment of dermatophyte toenail onychomycosis in the elderly. J Am Acad Dermatol 2001;44:479-84.
[Google Scholar]
|
| 9. |
Gupta AK, Ryder JE, Lynch LE, Tavakkol A. The use of terbinafine in the treatment of onychomycosis in adults and special populations: A review of the evidence. J Drugs Dermatol 2005;4:302-8.
[Google Scholar]
|
| 10. |
Farkas B, Paul C, Dobozy A, Hunyadi J, Horvath A, Fekete G. Terbinafine treatment of toenail onychomycosis in patients with insulin-dependent and non insulin-dependent diabetes mellitus: A multicetre trail. Br J Dermatol 2002;146:254-60.
[Google Scholar]
|
| 11. |
Cribier BJ, Bakshi R. Terbinafine in the treatment of onychomycosis: A review of its efficacy in high-risk populations and in patients with nondermatophyte infections. Br J Dermatol 2004;150:414-20.
[Google Scholar]
|
| 12. |
Alpsoy E, Yilmaz E, Basaran E. Intermittent therapy with terbinafine for dermatophyte toe nails onychomycosis. J Dermatol 1996;23:259-62.
[Google Scholar]
|
| 13. |
Tosti A, Piraccini BM, Stinchi C, Venturo N, Bardazzi F, Colombo MD. Treatment of dermatophyte nail infections: An open randomized study comparing intermittent terbinafine therapy with continuous terbinafine treatment and intermittent itraconazole therapy. J Am Acad Dermatol 1996;34:595-600.
[Google Scholar]
|
| 14. |
Pavlotsky F, Armoni G, Shemer A, Trau H. Pulsed versus continuous terbinafine dosing in the treatment of dermatophyteonychomycosis. J Dermatol Treat 2004;15:315-20.
[Google Scholar]
|
| 15. |
Warshaw EM, Fett DD, Bloomfield HE, Grill JP, Nelson DB, Quintero V, et al. Pulse versus continuous terbinafine for onychomycosis: A randomized, double-blind, controlled trial. J Am Acad Dermatol 2005;53:578-84.
[Google Scholar]
|
| 16. |
Backer MD, Vroey CD, Lesaffre E, Scheys I, Keyser PD. Twelve weeks of continuous oral therapy for toenail onychomycosis caused by dermatophytes: A double blind comparative trial of terbinafine 250 mg/day versus itraconazole 200 mg/day. J Am AcadDermatol 1998;38:S57-63.
[Google Scholar]
|
| 17. |
Haneke E, Tausch I, Brautigam M, Weidinger G, Welzel D. Short duration treatment of fingernail dermatophytosis: A randomized, double blind study with terbinafine and griseofulvin. J Am Acad Dermatol 1995;32:72-7.
[Google Scholar]
|
| 18. |
Evans EG, Sigurgeirsson B. Double blind, randomized study of continuous terbinafine compared with intermittent itraconazole in treatment of toenail onychomycosis. BMJ 1999;318:1031-5.
[Google Scholar]
|
| 19. |
Havu V, Heikkilä H, Kuokkanen K, Nuutinen M, Rantanen T, Saari S, et al. A double-blind, randomized study to compare the efficacy and safety of terbinafine with fluconazole in the treatment of onychomycosis. Br J Dermatol 2000;142:97-102.
[Google Scholar]
|
| 20. |
Sigurgeirsson B, Olafsson JH, Steinsson JB, Paul C, Billstein S, Evans EG. Long term effectiveness of treatment with terbinafinevsitraconazole in onychomycosis: A 5 year blinded prospective follow up study. Arch Dermatol 2002;138:353-7.
[Google Scholar]
|
Fulltext Views
12,168
PDF downloads
2,747





