Translate this page into:
Comparative study of the efficacy and safety of two grafting procedures (an automated epidermal harvesting system and non-cultured epidermal cell suspension) in the treatment of stable vitiligo
Corresponding Author: Dr. Bhavni Oberoi, Department of Dermatology, INHS Asvini, Mumbai, Maharashtra, India. bhavni.oberoi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Oberoi B, Baveja S, Pathania V, Neema S. Comparative study of the efficacy and safety of two grafting procedures (an automated epidermal harvesting system and non-cultured epidermal cell suspension) in the treatment of stable vitiligo. Indian J Dermatol Venereol Leprol 2023;89:536–42.
Abstract
Background
The non-cultured epidermal cell suspension method is a well-established but tedious grafting modality in the management of stable vitiligo. Recently a more user-friendly automated epidermal harvesting system has been introduced.
Aim
This was a pilot study to compare the efficacy and safety outcomes of the above two grafting procedures.
Study design
The study was a single-blinded split-body randomised controlled trial. After scientific and ethical clearance, the trial was registered with CTRI (CTRI/2018/05/014225). Thirty consenting patients of stable vitiligo with 60 near-symmetrical patches were recruited. Block randomisation was done using computer-generated randomisation software and each patch was allocated either of the two grafting modalities. Efficacy was assessed by the Physician Global Assessment Scale on serial images and pain by the Numerical Rating Pain Scale.
Results and conclusion
The non-cultured epidermal cell suspension was found to be an overall statistically superior technique to the automated epidermal harvesting system in terms of efficacy (re-pigmentation). Both donor and recipient site complications were significantly less with the automated epidermal harvesting system grafting and this method had the distinct advantage of being a painless and easy technique with minimal recovery time. A novel observation was that a good colour match and near-complete re-pigmentation occurred in patients with a darker skin colour with both techniques.
Limitations
The main limitation of our study was the small sample size. Also, the size of the treated patches was limited such that they could be covered by the 5 × 5 cm size of the automated epidermal harvesting system blade. However, a larger area can be covered with multiple sessions.
Keywords
Vitiligo
automated epidermal harvesting system
non-cultured epidermal cell suspension
grafting
Plain Language Summary
This study highlights the utility of a novel modality for vitiligo grafting (automated epidermal harvesting system) in vogue for treating non-healing ulcers with that of non-cultured epidermal cell suspension. The two procedures were compared in an interventional trial. Though non-cultured epidermal cell suspension was found to be more efficacious, the distinct advantages of the automated epidermal harvesting system grafting were ease of use, minimal pain, and less complications. We recommend using this technique for smaller patches of vitiligo in patients with darker skin types.
Introduction
In stable vitiligo refractory to medical management and in segmental vitiligo, surgical therapies can often be the treatment of choice.1,2 These surgical techniques involve the replacement of the damaged melanocytes and collectively constitute the grafting procedures.3 The choice of grafting procedure adopted usually depends upon the extent, size, and site of the vitiligo lesions, the age and expectations of the patient and the expertise of the operating surgeon.4,5 These grafting techniques can be broadly divided into tissue grafting procedures like punch grafting, split thickness or suction blister grafting and cellular grafting procedures like non-cultured or cultured epidermal cell suspension grafting.6,7
Non-cultured epidermal cell suspension (NCES) is a time-tested routinely performed technique that has been found to have particularly good results.8 A new method in skin grafting is the autologous negative pressure epidermal harvesting system based on the principle of suction blister grafting.9 This technique, called automated epidermal harvesting system (AEHS), uses sustained vacuum, pressure and heat, resulting in the formation of microdomes of the epidermis (split at the dermoepidermal junction) which can be transferred as such to the recipient skin.10
This was a pilot study to determine the efficacy of this novel treatment modality viz., automated epidermal harvesting system for vitiligo grafting versus a well-established grafting modality viz., the non-cultured epidermal cell suspension. The study also was intended to understand when the automated epidermal harvesting system could be a preferred modality for vitiligo grafting. A review of the literature was done, and we could not find any previous study which has compared these grafting modalities.
Aims
To compare the efficacy and safety of two grafting procedures (automated epidermal harvesting system and non-cultured epidermal cell suspension) in the treatment of stable vitiligo.
Materials and methods
The study was a prospective, split-body (patient served as case and control with near symmetric patches), single-blinded (two independent outcome assessors were blinded) randomised control trial conducted in a tertiary care hospital in Western Maharashtra, India. Approval was taken from the institutional scientific and ethics committee and the trial was registered with the Clinical Trials Registry-India (CTRI - CTRI/2018/05/014225) and carried out over a period of two years. Using the proportion of vitiligo patients showing excellent re-pigmentation by both techniques, α = 5 % and a power of 80%, a minimum of 20 cases were required for each technique; however, a total of 30 non-segmental stable vitiligo patients fulfilling the inclusion criteria were enrolled for the study. Inclusion criteria included age >18 years, minimum six-month duration of stability, non-segmental vitiligo, and near-symmetric patches. The six months of stability were counted only after stopping any systemic therapy for stabilisation like narrow-band ultraviolet B (UVB) phototherapy or oral steroids. Pregnant women, patients with bleeding disorders, keloidal tendency and active infections were excluded. After taking written informed consent each patient was subject to detailed history and investigations as per the study proforma and baseline clinical images were taken.
Two comparable near-symmetrical vitiligo patches on either side of the body in each patient were selected for carrying out the procedures. Each was randomly allotted to group A or group B using computer-generated block randomisation. Vitiligo patches in group A were subjected to non-cultured epidermal cell suspension grafting whereas vitiligo patches in group B were treated with the automated epidermal harvesting system of grafting such that each patient was subjected to both the procedures on either side. The anterolateral aspects of both thighs of the patient were taken as donor sites (one thigh for each technique).
The suspension for non-cultured epidermal cell suspension grafting was prepared by the cold trypsinisation method over a span of two days.11 On the first day, thin split thickness skin grafts of about one-tenth to one-fourth of the recipient area were taken from the donor site (anterolateral thigh) after application of topical anaesthesia under complete aseptic precautions [Figures 1a and b]. The grafts were cut, thoroughly washed, and transferred to a sterile conical tube containing trypsin-ethylenediamine tetra-acetic acid (EDTA) solution [0.25% trypsin + 0.02% EDTA] and placed overnight for 18 hours at 4°C. On the second day, the melanocyte-keratinocyte suspension was prepared under a laminar airflow system. The trypsin solution was aspirated and the grafts were washed with Dulbecco’s Modified Eagle’s Medium. The test tube was subject to vigorous manual shaking to facilitate the separation of the dermis from the epidermis. The contents were then transferred to a petri dish and the dermis was teased gently with a fine forceps and separated from the epidermis. The solid fragments of epidermis and dermis were discarded. The melanocyte-keratinocyte cell suspension in the petri dish was transferred to a conical tube and centrifuged at 3600 rpm for 9 minutes to form a pellet [Figure 1c]. The supernatant was discarded, and the pellet was then mixed with 1 ml of Dulbecco’s Modified Eagle’s Medium and 1 ml of hydroxymethyl cellulose to increase the viscosity.

- Procedure of non-cultured epidermal cell suspension grafting: split thickness graft being taken from donor area on thigh

- Procedure of non-cultured epidermal cell suspension grafting: thin split thickness graft

- Procedure of non-cultured epidermal cell suspension grafting: melanocyte pellet after centrifugation
The vitiligo patches (recipient sites) in both groups A and B were cleaned, draped and under topical anaesthesia were dermabraded till the papillary dermis (pinpoint bleeding) with a motorized dermabrader. The melanocyte-keratinocyte suspension was pipetted out and was applied over group A patches followed by a collagen dressing, semi-porous dressing, gauze pieces and adhesive dressing to form a four-layer dressing which was kept in place for a week [Figure 1d].

- Procedure of non-cultured epidermal cell suspension grafting: 4-layer dressing after non-cultured epidermal cell suspension grafting
For automated epidermal harvesting system (Cellutome) [Figure 2a] grafting the harvester blade was positioned at the opposite thigh from where the split-thickness graft was taken [Figure 2b]. The device delivers pressure and warmth with an automated setting to form an array of 128, 2 mm wide microdomes with clear fluid over approximately 30-40 minutes (usually set at 35 minutes and can be increased if microdomes are not properly formed) [Figure 2a and c]. No anaesthesia was used for this technique. The microdomes were captured by a self-adhesive semi-porous dressing [Figure 2d] which formed a transferrable skin micrograft that was immediately applied to the dermabraded recipient site, prepared as above. The self-adhesive dressing was covered with two layers of dressing and left intact for a period of 21 days. Procedures on both the days were carried out on OPD basis such that the donor graft for NCES grafting was taken on the first day and the remaining NCES procedure and AEHS grafting were carried out on the second day.
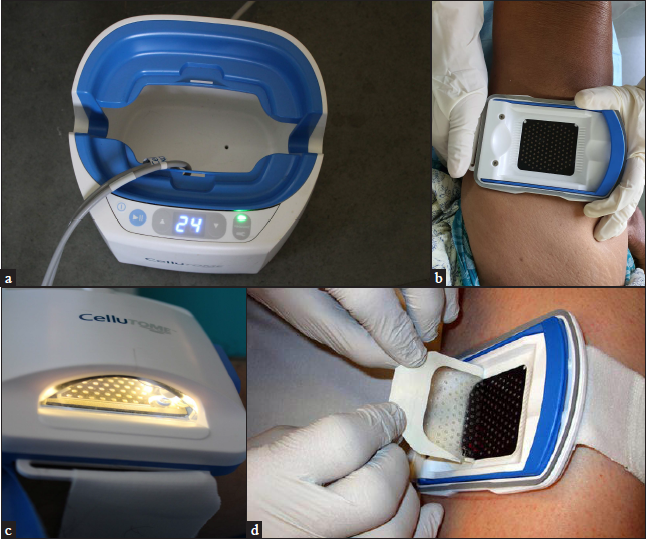
- (a) Procedure of automated epidermal harvesting system grafting: timer set on the equipment; (b) Procedure of automated epidermal harvesting system grafting: blade being positioned on donor area of thigh; (c) Procedure of automated epidermal harvesting system grafting: apparatus attached to blade; (d) Procedure of automated epidermal harvesting system grafting: semi-porous dressing containing microdomes being removed from the donor site
All patients were followed up with narrow band-ultraviolet B phototherapy with the same frequency and duration after removal of dressing on the 21st day on both the sites. Serial images were taken pre-procedure, at one month and then at three-monthly intervals for one year with the same camera settings and lighting and were taken by the same person. The response to the therapy was assessed subjectively using the Physician Global Assessment Scale as follows: 75-100% (excellent repigmentation), 50-75% (good repigmentation), 25-50% (moderate repigmentation) and 0-25% (mild repigmentation). All photos were rated together at the end of the study. Assessment was done on digital screen on the same device with the same lighting for all patients. Two independent observers who were not a part of the procedure and were blinded to which side the two procedures were done (single-blinded) were made to make their assessments while the images were projected. Most of the assessments were same with minimal variation. In case of non-agreement, the lower value was taken.
Pain was assessed by the Numerical Rating Pain Scale (0 as the absence of pain and 10 as the most intense pain possible). Scores were taken at the end of each day as a pain experience for the day and not separately for the procedures. On day 1 only the graft for NCES was taken which is the most painful part of the procedure so the pain was attributed to the taking of graft and over the graft site after weaning of anaesthesia. On day 2 the patients only reported pain during dermabrasion which was common for both procedures.
A comparison was made by the same observers of any complications associated with the procedures like a colour mismatch and perigraft halo at the recipient site (colours were rated as same, somewhat lighter than and somewhat darker than the surrounding normal skin); and dyspigmentation (mixed hyper and hypopigmentation) and scarring (atrophic or hypertrophic) at the donor site. The complications were recorded at each visit; however, the assessment of complications was done at the end of 12 months. Also, variations in results depending on the Fitzpatrick skin type were studied. Data were subjected to statistical analysis using SPSS [Statistical Package for Social Sciences, version 25:0] software and results were compared (P -value < 0.05 was considered as significant).
Results
Out of 30 patients a total of 11 patients (36.7%) were males and 19 (67.3%) were females, and the mean age of patients was 32 ± 10 years. The minimum duration of stability for inclusion was taken at 6 months in our study, that is a minimum Vitiligo Disease Activity score of +1; however, most of the patients (26 out of 30) recruited had a Vitiligo Disease Activity score of at least zero off therapy. The remaining 4 patients were stable on treatment for 12 months before surgery and off treatment for at least six months. The patients enrolled had a Fitzpatrick skin type ranging from III to V with a majority (17, 56.6%) having a Fitzpatrick skin type of IV [Table 1]. The minimum duration of stability was six months while the maximum was seven years with a mean duration of 1.8 ± 1.4 years. The sites involved were acral in 9 out of 30 patients (30%), followed by trunk (26.7%), face (16.7%) and over joints like elbows and knees (13.3%). Similar sites were chosen for both the techniques so both the groups were comparable in terms of the site of vitiligo. The size of the patches chosen for assessment was also similar with a maximum area of 25 sqcm to cover the area covered by the AEHS harvester (blade). All patients completed the follow up except one who turned unstable and developed spontaneous depigmentation and was released from further follow ups.
| Total number of patients- 30 | ||
|---|---|---|
| Age (years) | ||
| ≤ 20 | 5 | 16.7% |
| 21-30 | 9 | 30.0% |
| 31-40 | 9 | 30.0% |
| > 40 | 7 | 23.3% |
| Sex | ||
| Male | 11 | 36.7% |
| Female | 19 | 63.3% |
| Fitzpatrick skin type | ||
| III | 7 | 23.33% |
| IV | 17 | 56.6% |
| V | 6 | 20% |
At the end of six months, the NCES group had achieved excellent to complete (75-100%) re-pigmentation in 5 (16.6%) patches while in the AEHS group only one patch had achieved excellent re-pigmentation. At a follow-up of 12 months excellent (75-100%) re-pigmentation was seen in 8 (26.6%) patches in the NCES group [Figure 3] while the median re-pigmentation achieved was good (50-75%). In the AEHS group, excellent re-pigmentation was achieved at 12 months in 4 patches (13.3%) [Figure 4] while the median re-pigmentation was moderate (25-50%). By this time in the NCES group 7 patches (23.33%) had achieved a good pigmentation, 9 patches (30%) got a moderate pigmentation while 5 patches (16.67%) had a mild pigmentation. In the AEHS group 2 patches (6.67%) got a good pigmentation, 13 patches (43.33%) had a moderate pigmentation and 10 (33.33%) patches could get only a mild pigmentation. Not much effect was noted on leucotrichia (noted in 4 patches treated with NCES and 3 patches with AEHS) with either of the techniques. The difference between the two groups at 12 months was statistically significant (P- value 0.035) [Figure 5]. Site wise, patches on the face had the best re-pigmentation with both techniques followed by those on the trunk including the peri areolar region, followed by patches overlying joints; the least re-pigmentation was noted in acral areas including palms, soles and periungual areas, as expected. The same trend was seen with both the techniques as the sites were comparable. Patients with a darker skin type (Fitzpatrick types IV and V) were found to have better re-pigmentation with a greater number of patches with excellent or near complete pigmentation compared to those with Fitzpatrick skin type III. On comparing the re-pigmentation in patients with Fitzpatrick skin types IV and V it was found that the results with NCES were superior in patients with skin type IV while results with both techniques were comparable in patients having Fitzpatrick skin type V (P- value>0.05) [Figure 6].

- Excellent re-pigmentation achieved after 12 months of grafting by non-cultured epidermal cell suspension technique in Fitzpatrick skin type V

- Excellent re-pigmentation achieved after 12 months of grafting by automated epidermal harvesting system technique in Fitzpatrick skin type V

- Extent of re-pigmentation with both the techniques (NCES- Non cultured epidermal cell suspension; Cellutome refers to Automated Epidermal Harvester grafting)

- Re-pigmentation as per Fitzpatrick skin type (NCES- Non cultured epidermal cell suspension; Cellutome refers to Automated Epidermal Harvester grafting)
No donor site complications were found in the automated epidermal harvesting system group, with minimal damage to the epidermis on the day of surgery which healed completely over a week. While in the non-cultured epidermal cell suspension group 10 (33%) patients developed dyspigmentation and one patient developed atrophic scarring at the donor site. At the recipient site, in the NCES group 5 (16.6%) patches developed pigmentary complications like hyperpigmentation and another 5 (16.6%) had a perigraft halo, while in the AEHS group 2 out of 30 patches developed pigment mismatch (hyperpigmentation) at the recipient site. For these hyperpigmented patches the response grading was taken as complete depending upon the area covered by the repigmentation.
On day 1 of the procedures most patients complained of minimal pain at the time of taking the graft for NCES, which increased when the effect of anaesthesia wore off (average Numerical Rating Pain Scale of 6.5 out of 10). On day 2, with the AEHS technique, patients only reported mild warmth and occasional burning sensation generally after around 20 minutes of application of the automated epidermal harvesting system apparatus. The pain reported on that day was due to dermabrasion of the recipient sites (average Numerical Rating Pain Scale of 2.2 out of 10). The donor sites of NCES grafting took a minimum of seven days to heal and by this time the pain reported by patients also reduced.
Discussion
Among the prevalent surgical techniques for vitiligo, non-cultured epidermal cell suspension is a well-established, time-tested technique. In a study by Van Geelet al. it was reported to show >65% re-pigmentation in 40-100% of the patches.8 Another efficacious treatment modality which is a tissue-based technique is the suction blister technique which has been found to have near-similar results to the non-cultured epidermal cell suspension in terms of re-pigmentation.4,12
Most of these surgical techniques are cumbersome and need to be carried out as a planned procedure in an operation theatre. A new device, the automated epidermal harvesting system (Cellutome) carries out a type of suction blister grafting using suction and heat and has been recently introduced as a simple and quick out-patient procedure. The blade is designed in such a way that a 5 × 5 cm array comprising of 128 epidermal micro-grafts spaced 2 mm apart is created which can be easily collected onto a transparent adhesive film.10 In our study, a total of 30 comparable patches were chosen for each arm. The patches that were chosen were of relatively smaller size which could be covered by the 5 × 5 cm area, but both the sites chosen were comparable and mostly near-mirror images.
There was a female preponderance in our study; most other studies on vitiligo grafting procedures have shown a similar skewing of sex distribution.13 More than half of our patients had a Fitzpatrick skin type of IV with the remaining having a Fitzpatrick skin types III or V. Only a few previous studies of surgical grafting procedures in vitiligo have taken the Fitzpatrick skin type into cognizance.14 Minimal pain was reported during AEHS grafting compared to NCES grafting with a very low numerical rating pain score. Similar results were found in an initial study by Janowskaet al. where they reported an average pain score of 1.4 out of 5 by the automated epidermal harvesting system technique with the same device.15 The donor site healed within 24-48 hrs and the patient was symptom-free around an hour after the procedure.15
As in our study, similar groups for assessment by physician global assessment were formed in other studies also which have compared the surgical modalities in vitiligo.16,17
At the completion of our follow-up of 12 months, non-cultured epidermal cell suspension grafting method was found to be more efficacious than the automated epidermal harvester grafting in terms of repigmentation (P -value- 0.035). A possible explanation for a poorer response by the AEHS technique can be that the entire graft does not get captured by the Tegaderm™ dressing but only a few microdomes are picked when we pull the dressing.
Patients with a dark skin colour (Fitzpatrick type V) were found to have statistically comparable and highly efficacious results with both techniques in terms of excellent repigmentation.
As regards complications, the automated epidermal harvesting system grafting was found to be superior with negligible complications at both donor and recipient sites. One patient turned unstable and developed spontaneous depigmentation. Some complications were noted in the non-cultured epidermal cell suspension group, mostly dyspigmentation and scarring at the donor site. Similar results were published by Leelavathy B et al. in a study of 30 patients to evaluate the efficacy of non-cultured epidermal cell suspensions, where colour mismatch was the most reported complication followed by scarring at the donor site. They also reported infections and scarring at the recipient site which was not seen in our study. Also, one patient (3.33%) was unable to sustain pigmentation during follow-up in that study, similar to the one patient in our study who developed spontaneous depigmentation.18
Limitations
The main limitation of our study was the small sample size. Also, the size of the treated patches was limited such that they could be covered by the 5 × 5 cm size of the automated epidermal harvesting system blade; however, a larger area can be covered with multiple sessions. Also, no patient-based rating was used for the assessment of repigmentation.
Conclusion
The findings of this study conclude that non-cultured epidermal cell suspension grafting is more efficacious than the automated epidermal harvesting system grafting used in terms of re-pigmentation. However, considering the ease of the procedure and minimal complications with the automated epidermal harvesting system group along with better results in darker skin types (Fitzpatrick skin type V), it could be used as a first-line treatment modality for such patients who have small patches of vitiligo which can be covered by the automated epidermal harvesting system blade. Also, an alternative method for harvesting microdomes (for example, cutting the microdomes with scissors and transplanting, as in suction blister) for the AEHS technique can be tried to improve the yield of grafts.
Further patient studies with larger samples are required to determine the place of this new technique in the armamentarium of vitiligo grafting.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Surgical therapy of vitiligo: Current status. Indian J Dermatol Venereol Leprol. 2005;71:307-10.
- [CrossRef] [PubMed] [Google Scholar]
- Grafting in vitiligo: How to get better results and how to avoid complications. J Cutan Aesthet Surg. 2013;6:83-9.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermal grafting in vitiligo: Influence of age, site of lesion, and type of disease on outcome. J Am Acad Dermatol. 2003;49:99-104.
- [CrossRef] [PubMed] [Google Scholar]
- Update on skin repigmentation therapies in vitiligo. Pigment Cell Melanoma Res. 2009;22:42-65.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of vitiligo by transplantation of cultured pure melanocyte suspension: Analysis of 120 cases. J Am Acad Dermatol. 2004;51:68-4.
- [CrossRef] [PubMed] [Google Scholar]
- Advanced treatment modalities for vitiligo. Dermatol Surg. 2012;38:381-91.
- [CrossRef] [PubMed] [Google Scholar]
- A Review of Non-cultured Epidermal Cellular Grafting in Vitiligo. J Cutan Aesthet Surg. 2011;4:17-2.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermal micrografts produced via an automated and minimally invasive tool form at the dermal/epidermal junction and contain proliferative cells that secrete wound healing growth factors. Adv Skin Wound Care. 2015;28:397-05.
- [CrossRef] [PubMed] [Google Scholar]
- An Automated and Minimally Invasive Tool for Generating Autologous Viable Epidermal Micrografts. Adv Skin Wound Care. 2016;29:57-4.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191-4.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective study to assess the efficacy of various surgical modalities in treatment of stable vitiligo patches over resistant sites. Int J Dermatol. 2020;59:837-42.
- [CrossRef] [PubMed] [Google Scholar]
- Suction blister epidermal grafts combined with CO2 laser superficial ablation as a good method for treating small-sized vitiligo. Dermatol Surg. 2009;35:601-6.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermal grafting for vitiligo in adolescents. Pediatr Dermatol. 2002;19:159-62.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermal skin grafting in vitiligo: A pilot study. Int Wound J. 2016;13:47-1.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study of efficacy of cultured versus non cultured melanocyte transfer in the management of stable vitiligo. Med J Armed Forces India. 2014;70:26-1.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison between autologous noncultured extracted hair follicle outer root sheath cell suspension and autologous noncultured epidermal cell suspension in the treatment of stable vitiligo: A randomized study. Br J Dermatol. 2013;169:287-93.
- [CrossRef] [PubMed] [Google Scholar]
- The first transepidermal transplantation of non-cultured epidermal suspension using a dermarolling system in vitiligo: A sequential histological and clinical study. Pigment Cell Melanoma Res. 2017;30:493-7.
- [CrossRef] [PubMed] [Google Scholar]






