Translate this page into:
Comparison of acquired bilateral nevus of Ota-like macules in men and women
2 Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
Correspondence Address:
Sung Eun Chang
Department of Dermatology, Asan Medical Center, University of Ulsan College of Medicine, 388-1 Pungnap-dong Songpa-gu, Seoul 138-736
Korea
| How to cite this article: Lee WJ, Lee GY, Won KH, Won CH, Lee MW, Choi JH, Chang SE. Comparison of acquired bilateral nevus of Ota-like macules in men and women. Indian J Dermatol Venereol Leprol 2014;80:313-319 |
Abstract
Background: The clinical and histopathological characteristics of acquired bilateral nevus of Ota-like macules in men are poorly documented due to its rarity. Aims: To compare the clinical and histopathological characteristics of acquired bilateral nevus of Ota-like macules in men with the condition in women. Methods: We studied 11 men and 62 women, all with a clinical diagnosis of acquired bilateral nevus of Ota-like macules. Biopsies were taken from 5 men and 10 women and their clinical and histopathological features were compared. Results: The most frequently affected site in men was the forehead [8 (73%) out of 11 patients]. Lesions on the forehead were more common in men than women (P = 0.001). In contrast to women, there was no apparent tendency of the lesions to become more blue with age in men. Concurrent melasma was observed in 14 (23%) out of 62 women, but not in men. Extra-facial acquired dermal melanocytosis was noted in 2 (18%) out of 11 men and in none of the 62 women. Conclusion: Significant differences were noted between men and women in the appearance of concurrent pigmentary lesions and the distribution of lesions. Extra-facial acquired dermal melanocytosis was noted in men.INTRODUCTION
Acquired bilateral nevus of Ota-like macules, or Hori nevus, was first described by Hori et al., in 1984. [1] This is a common acquired facial dermal melanocytosis in Asians and has distinctive features. It is characterized by multiple speckled, bilateral, blue-gray and brown areas of pigmentation on both cheeks, the sides of the forehead, temples, eyelids, the root of the nose, and the ala nasi. Recent histopathological studies identified differences between the melanocytes of acquired bilateral nevus of Ota-like macules and those of the nevus of Ota. Melanocytes in acquired bilateral nevus of Ota-like macules are bipolar and irregularly shaped and are dispersed throughout the upper dermis, often in a perivascular fashion. [2],[3] In contrast, melanocytes in the nevus of Ota are diffusely distributed throughout the upper and lower dermis. [3] Nevus of Ota melanocytes contain mature, late-stage melanosomes whereas those in acquired bilateral nevus of Ota-like macules contain melanosomes at earlier stages of melanization (stages II, III, and IV). [4],[5]
A population-based study has found the overall prevalence of acquired bilateral nevus of Ota-like macules to be 2.5% in Chinese people. The authors also noted that this condition was more common in women. [6],[7] More than 90% of the cases in that study were female and the majority of those affected were aged 45-55 years (median- 46 years). [6] The condition was less common in very young (<25 years) and very old (>75 years) women. Few reports have characterized the condition in men.
The aim of our present study was to characterize the clinical and histopathological features of acquired bilateral nevus of Ota-like macules in men and examine the differences between this condition in men and women.
METHODS
This study was conducted in accordance with the Declaration of Helsinki principles and was approved by the Institutional Review Board of the Asan Medical Center.
The study cohort comprised 11 men and 62 women, all with a clinical diagnosis of acquired bilateral nevus of Ota-like macules. Both men and women were examined at the Dermatology Outpatient Clinic at the Asan Medical Center from December 2000 to April 2013. The diagnosis was made on the basis of the characteristic brown/blue color and symmetrical distribution of the lesions. All cases were diagnosed by dermatologists through examination and history taking, which included both family and drug histories. The site and color of all lesions in the study cohorts were estimated. The color of the lesions was categorized as brown, slate-gray or blue. All patients were examined for the presence of other pigmentary disorders, including facial nevomelanocytic nevi, facial seborrheic keratosis, melasma and extra-facial acquired dermal melanocytosis. Biopsy specimens were taken from lesions in 5 men and 10 women. Melanin was visualized using the Fontana-Masson stain, and melanocytes were detected using the Melan A stain. The number of melanocytes as well as the amount of melanin pigment per unit area in the epidermis and dermis was evaluated using image analysis software (Image J; National Institutes of Health, Bethesda, MD). Image analysis was performed at a constant magnification (original magnification ×100). The dermal depth at which the melanocytes occurred was assessed by measuring the distance from the top of the granular layer to the deepest dermal melanocytes using a scale mounted in the eyepiece of the microscope.
Statistical analysis
All statistical analyses were performed using SPSS, version 18.0 (SPSS Inc., Chicago, IL). Fisher′s exact test was used to examine differences in affected sites between men and women. Differences in the occurrence of concurrent extra-facial acquired dermal melanocytosis between men and women were examined using the Fisher′s exact test. A linear-by-linear association test was performed to analyze differences in the color of the lesions between the two groups. The Student′s t-test was used to analyze differences in age at first presentation and age at onset between the two groups. Spearman′s correlation analysis was performed to determine whether age had a significant effect on lesion color. The data from the histological studies were evaluated with a Mann-Whitney U test. All P values were two sided and a value of P < 0.05 was considered statistically significant.
RESULTS[/tAG:2]
Patients
The clinical data for the 11 male patients are summarized in [Table - 1]. The mean age was 36.5 years (range: 18-58). The mean age at onset was 31.5 years (range: 17-54). The mean age of the female patients was 33.8 years (range: 21-56) and the estimated mean age at lesion onset was 33.1 years (range: 16-54). There were no statistically significant differences between the men and women in terms of age at first presentation (P = 0.12) or age of onset (P = 0.28). Most patients were of Fitzpatrick skin type IV [men: 7 (64%) out of 11; women: 43 (69%) out of 62] and the remainder were type III [men: 4 (36%) out of 11; women: 19 (31%) out of 62].
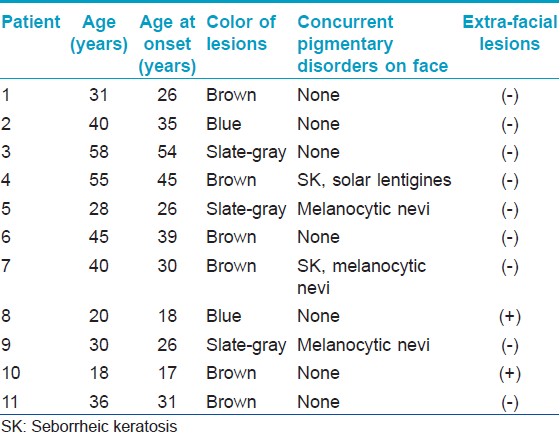
Concurrent pigment disorders of the face, such as facial nevomelanocytic nevi, solar lentigines, facial seborrhoiec keratoses, and melasma, were observed in 4 (36%) out of 11 male patients and in 23 (37%) out of 62 female patients [Table - 2]. Nevomelanocytic nevi and seborrhoiec keratoses were common concurrent disorders in men but melasma was the most common concurrent pigmentary disorder in women. There was a significant difference in the prevalence of melasma between women and men (P = 0.001). Concurrent melasma was observed in 14 (23%) out of 62 women, whereas none of the men showed evidence of melasma. Lesions of extra-facial acquired dermal melanocytosis were noted in 2 (18%) out of 11 men [Figure - 1] and in none of the 62 women. Concurrent extra-facial lesions were significantly more common in men than women (P = 0.021).

 |
| Figure 1: Two male patients with concomitant extra-facial acquired dermal melanocytosis |
Clinical features in two men with extra-facial acquired dermal melanocytosis
Patient 1
A 28-year-old man presented with pigmentary lesions on the face, both hands, feet, and back. The pigmentation on the nasal root started at the age of 3 and on the hands/feet at the age of 13. There were a number of brown macules scattered over the dorsum of hands and feet. The patient noticed discrete brown macules on the zygomatic area and forehead at the age of 25. He took no oral medications when the skin lesions were found. A diagnosis of acquired bilateral nevus of Ota-like macules with extra-facial lesions was made on the basis of clinical features and histopathological evaluation.
Patient 2
A 20-year-old man presented with a history of pigmentation on his face of three years duration. The patient had multiple hyperpigmented macules on the right forearm that had appeared 12 years previously. He denied any history of taking oral medication. Based on the clinical and histopathological findings, we diagnosed the facial lesion as acquired bilateral nevus of Ota-like macules and those on the right arm as extra-facial acquired dermal melanocytosis.
Distribution of the lesions
The distribution of the lesions is summarized in [Figure - 2]. In men, the most frequently affected site was the forehead [8 (73%) out of 11 patients] [Figure - 3]. Zygomatic lesions were noted in 6 (55%) out of 11 male patients; however, all female patients had zygomatic lesions. Forehead lesions were significantly more common in men than women (P = 0.001), whereas zygomatic lesions were significantly more common in female patients (P = <0.001).
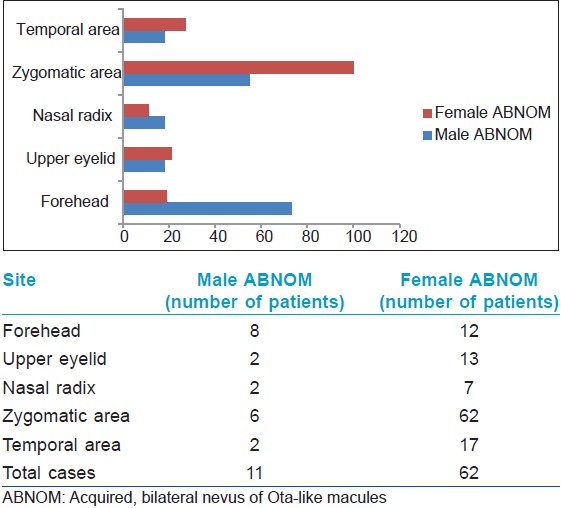 |
| Figure 2: Affected sites in patients. Forehead lesions were significantly more common in men than women, whereas zygomatic lesions were signifi cantly more common in women |
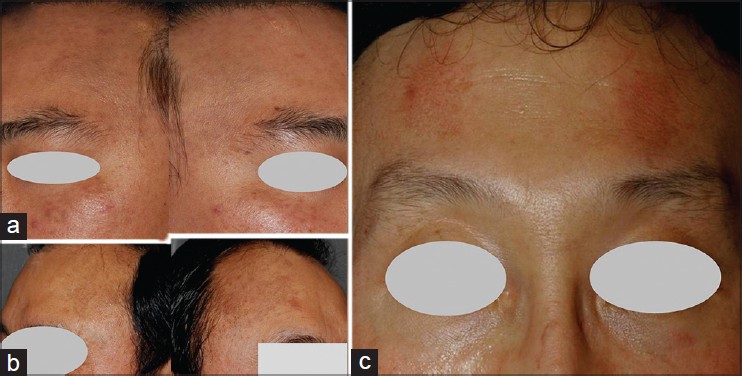 |
| Figure 3: Lesions on the forehead in men. (a) Multiple bluish macules on the forehead and both zygoma. (b) Multiple slategray macules on the lateral sides of the forehead. (c) Brownish macules on the forehead |
Lesion color
Of the 11 men, 6 had brown lesions and 2 had blue lesions [Table - 2]. There was no correlation between patient age and lesion color in men. Of the 62 women, 29 had brown lesions and 16 had blue lesions. According to Spearman′s correlation analysis, lesions tended to become bluer with age in women (correlation coefficient, r = 0.548; P < 0.001). Brown lesions were observed in 17 (77%) out of 22 patients younger than 30 years; blue macules were noted in one patient. In contrast, 9 (60%) out of 15 patients older than 40 years of age had blue lesions [Figure - 4]. There was no significant difference in lesion color between men and women (P = 0.83).
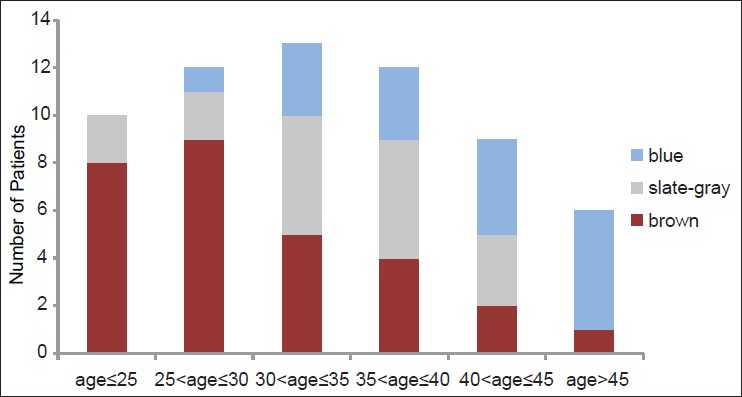 |
| Figure 4: Lesion color according to the age of women. Lesions in older patients tended to be bluer |
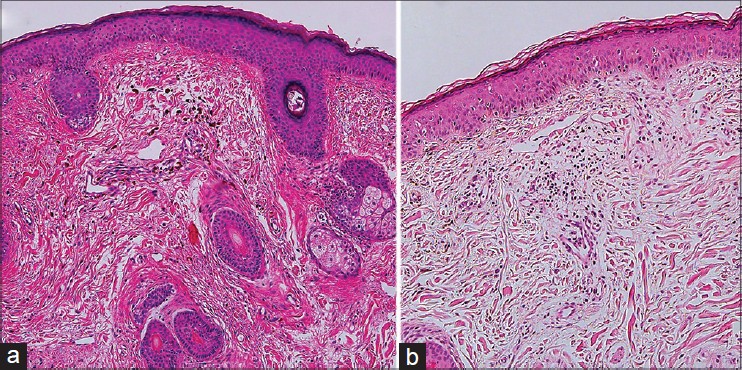
Histopathological findings
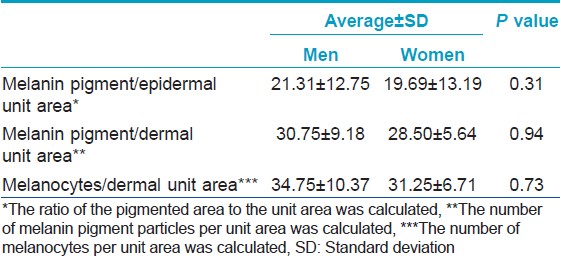
Histopathological findings were similar in men and women. Biopsies of the lesions revealed elongated, slender, pigment-bearing cells that were dispersed throughout the upper dermis. Melanocytes were interstitially dispersed between the collagen fibers of the dermis, with the long axis parallel to the collagen fibers [Figure - 5]a. They were rarely located in the perivascular area in either men or women. Histopathological findings for extra-facial lesions in men were similar to those for facial lesions [Figure - 5]b. There was no difference in the degree of epidermal pigmentation or in the number of dermal melanocytes between men and women [Table - 3]. In addition, there was no significant difference in the depth of the dermal melanocytes between men and women [mean depth (mm); 0.63 ± 0.21 in women, 0.58 ± 0.18 in men; P = 0.32].
 |
| Figure 5: Histopathological findings in (a) acquired bilateral nevus of Ota-like macules (hematoxylin and eosin, ×100) and (b) extra-facial lesions (hematoxylin and eosin, ×100) in a man. Melanocytes dispersed between the collagen fibers throughout the upper dermis were noted |
DISCUSSION
The pathogenesis of acquired bilateral nevus of Ota-like macules is unclear. Three mechanisms have been postulated to explain the origin of the melanocytes observed in patients with this condition: [1],[8] (1) epidermal melanocytes "drop" into the dermis; (2) hair bulb melanocytes migrate into the dermis; or (3) dermal melanocytes migrating from the neural crest during embryological development fail to reach their proper location in the basal layer of the epidermis. The mechanism of "epidermal melanocyte migration" is consistent with the fact that the color of the macules varies with the maturity of the lesion. The early-stage lesions are thought to be brown because the melanocytes are present within the basal layer of the epidermis; their subsequent migration into the dermis results in a darker bluish-gray color. [8] The finding that macules in women in the present study became progressively bluer with age is consistent with this mechanism; however, no progressive age-associated color change was noted in men.
Dermal melanocytes derived from embryological development may be latent and unnoticed at birth, but melanogenesis is activated later by an unknown event. [1] Some factors associated with the "activation of latent melanocytes" mechanism may induce the development of acquired bilateral nevus of Ota-like macules. The fact that this condition mainly affects women suggests that female sex hormones play a role. This is supported by the finding that the onset of lesions peaks after puberty and declines after menopause. [6] However, recent studies found no increase in the expression of estrogen and progesterone receptors in patients with this disorder. [9] Exposure to UV light is thought to be the most probable cause of lesions in the zygomatic area which often receives a high dose of radiation relative to other areas of the face. [1],[4]
Acquired dermal melanocytosis is a pigmentary disorder that is clinically characterized by the appearance of blue-brown macules which are most frequently observed on the face of Asian women. Extra-facial lesions are rare but can occur on the back, limbs, or extremities. [10],[11],[12],[13] It is unclear whether the extra-facial condition is a separate entity from acquired bilateral nevus of Ota-like macules. A previous study found no significant difference in the histopathological features of facial and extra-facial lesions. [11] In our study, there were no differences in the histopathological findings in extra-facial and facial lesions from two (18%) male patients who had lesions at both sites. Dermal melanocytes were distributed throughout the upper dermis in both lesions. Several reports have described acquired dermal melanocytosis that simultaneously involved the face and other body areas. [4],[5],[10],[14] In the present study, 2 (18%) out of 11 male patients also showed extra-facial pigmentation on the hands, arm, back, and feet while it was seen in none of the 62 women, a statistically significant difference. Although few reports have evaluated the development of acquired bilateral nevus of Ota-like macules in men, these patients often develop facial lesions with concurrent extra-facial lesions on the limbs, palms, fingers, and the dorsum of the hand [Table - 4]. [4],[10],[11],[15]
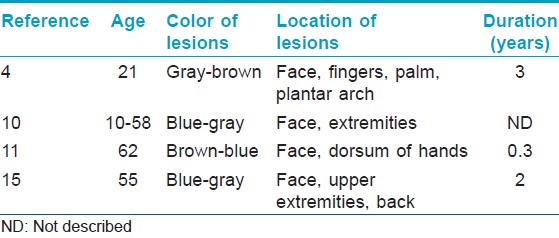
The finding that two male patients in our study showed concurrent extra-facial lesions suggests that the pathogenesis of acquired bilateral nevus of Ota-like macules in men may be different from that in women. A recent large epidemiological study found no association between sun exposure and acquired bilateral nevus of Ota-like macules in men; however, sun exposure increased the risk of developing macules in women. [6] These different characteristics suggest that female sex hormones may act synergistically with UV radiation to trigger the development of pigmentation in women. Although rare, men can present with extra-facial pigmentation which is part of the same disease spectrum, not related to UV radiation and sex hormones. Congenital predisposition to acquired dermal melanocytosis may be more important than acquired factors such as UV exposure in the development of acquired bilateral nevus of Ota-like macules in men.
There is some debate as to whether dermal melanocytosis subtypes are part of the same disease spectrum. Acquired bilateral nevus of Ota-like macules could be associated with Ota′s nevus, [16] and acquired dermal melanocytosis following the distribution of the nevus of Ito has been described. [17] Whitemore et al.[18] described an acquired unilateral nevus of Ota, also known as Sun′s nevus, in a 42-year-old woman. In our present study, two male patients had dermal melanocytic lesions in the extra-facial area from childhood. These cases may support the view that acquired forms of dermal melanocytosis are not separate entities from congenital dermal melanocytosis. Acquired bilateral nevus of Ota-like macules and extra-facial lesions may be attributable to the activation of latent dermal melanocytes from the neural crest during embryological development. [5] Acquired bilateral nevus of Ota-like macules is more common in women than men because these congenitally formed dormant melanocytes would be activated by sex hormones or UV radiation in women but not in men.
We further found in our current analyses that although the zygomatic area was often affected in both male and female patients, forehead lesions were significantly more common in men. Murakami et al.[10] compared the clinical features of atopic dermatitis-associated acquired bilateral nevus of Ota-like macules which were relatively common in men and frequently occurred on the forehead, with those of idiopathic lesions. Although the reasons for the observed differences in the affected sites in men and women in the present study are unclear, UV exposure and female sex hormones are strong candidates. Zygomatic lesions are more common in women than men because UV irradiation has a significant role in the development of lesions in women. The high prevalence of concurrent melasma observed in the female patients may also support this difference.
The color of the lesions in men was not different from that in women with brown lesions being the most common. In contrast to female patients, there was no tendency for the lesions to become bluer with age in male patients. We found no differences in the degree of epidermal pigmentation or in the number of melanocytes, between male and female patients. Dermal melanocytes were interstitially distributed throughout the upper dermis in both male and female acquired bilateral nevus of Ota-like macules; however, it should be noted that we only studied a small number of specimens.
In conclusion, despite the limitations of a small sample size, the results of our present study strongly suggest that the characteristics of acquired bilateral nevus of Ota-like macules in men are distinct from those of female patients. As such, this study will provide a basis for further investigations into the pathogenesis of male acquired bilateral nevus of Ota-like macules. We found that, unlike those in women, the lesions in men occurred mainly on the forehead, and the condition showed a relatively high association with extra-facial lesions. Acquired bilateral nevus of Ota-like macules in men does not appear to be a separate entity from extrafacial melanocytosis. We could not exclude the possibility that lesions in male patients may be attributed to the late appearance of congenitally formed dormant melanocytes migrating from the neural crest.
| 1. |
Hori Y, Kawashima M, Oohara K, Kukita A. Acquired, bilateral nevus of Ota-like macules. J Am Acad Dermatol 1984;10: 961-4.
[Google Scholar]
|
| 2. |
Park JM, Tsao H, Tsao S. Acquired bilateral nevus of Ota-like macules (Hori nevus): Etiologic and therapeutic considerations. J Am Acad Dermatol 2009; 61:88-93.
[Google Scholar]
|
| 3. |
Lee B, Kim YC, Kang WH, Lee ES. Comparison of characteristics of acquired bilateral nevus of Ota-like macules and nevus of Ota according to therapeutic outcome. J Korean Med Sci 2004;19: 554-9.
[Google Scholar]
|
| 4. |
Hidano A, Kaneko K. Acquired dermal melanocytosis of the face and extremities. Br J Dermatol 1991;124: 96-9.
[Google Scholar]
|
| 5. |
Mizushima J, Nogita T, Higaki Y, Horikoshi T, Kawashima M. Dormant melanocytes in the dermis: Do dermal melanocytes of acquired dermal melanocytosis exist from birth? Br J Dermatol 1998;139: 349-50.
[Google Scholar]
|
| 6. |
Wang BQ, Shen ZY, Fei Y, Li H, Liu JH, Xu H, et al. A population-based study of acquired bilateral nevus of Ota like macules in Shanghai, China. J Invest Dermatol 2011;131: 358-62.
[Google Scholar]
|
| 7. |
Cho SB, Park SJ, Kim MJ, Bu TS. Treatment of acquired bilateral nevus of Ota-like macules (Hori's nevus) using 1064-nm Q-switched Nd: YAG laser with low fluence. Int J Dermatol 2009; 48:1308-12.
[Google Scholar]
|
| 8. |
Ee HL, Wong HC, Goh CL, Ang P. Characteristics of Hori naevus: A prospective analysis. Br J Dermatol 2006;154: 50-3.
[Google Scholar]
|
| 9. |
Long TF, Liu L, He L, Shen LD, Gu H, Yang Z, et al. Androgen, estrogen and progesterone receptors in acquired bilateral nevus of Ota-like macules. Pigment Cell Melanoma Res 2010; 23:144-6.
[Google Scholar]
|
| 10. |
Murakami F, Soma Y, Mizoguchi M. Acquried symmetrical dermal melanocytosis (naevus of Hori) developing after aggravated atopic dermatitis. Br J Dermatol 2005;152: 903-8.
[Google Scholar]
|
| 11. |
Lee JY, Lee JS, Kim YC. Histopathological features of acquired dermal melanocytosis. Eur J Dermatol 2010; 20:345-8.
[Google Scholar]
|
| 12. |
Mizoguchi M, Murakami F, Ito M, Asano M, Baba T, Kawa Y, et al. Clinical, pathological, and etiologic aspects of acquired dermal melanocytosis. Pigment Cell Res 1997; 10:176-83.
[Google Scholar]
|
| 13. |
Kawakami T, Saito C, Soma Y. Acquired dermal melanocytosis naevus of Ota-like macules on the face and extremities lesions in a young Japanese Woman. Acta Derm Venereol 2009; 89:415-6.
[Google Scholar]
|
| 14. |
Buka R, Mauch J, Phelps R, Rudikoff D. Acquried dermal melanocytosis in an African-American: A case report. J Am Acad Dermatol 2000; 43:934-6.
[Google Scholar]
|
| 15. |
Ono S, Hori M, Yamashita K, Yamakawa M. Generalized type of acquired dermal melanocytosis. Nihon Hifuka Gakkai Zasshi 1991; 101:965-71.
[Google Scholar]
|
| 16. |
Park JH, Lee MH. Acquired, bilateral nevus of Ota-like macules (ABNOM) associated with Ota' nevus: Case report. J Korean Med Sci 2004;19:616-8.
[Google Scholar]
|
| 17. |
Mataix J, López N, Haro R, González E, Angulo J, Requena L. Late-onset Ito's nevus: An uncommon acquired dermal melanocytosis. J Cutan Pathol 2007; 34: 640-3.
[Google Scholar]
|
| 18. |
Whitemore SE, Wilson BB, Copper PH. Late-onset nevus of Ota. Cutis 1991; 48: 213-6.
[Google Scholar]
|
Fulltext Views
4,748
PDF downloads
3,386





