Translate this page into:
Comparison of dermatoses seen in community health camps and a tertiary care centre in Kashmir
2 Community Medicine, Govt. Medical College, Srinagar, University of Kashmir, Jammu and Kashmir, India
Correspondence Address:
Iffat Hassan
Postgraduate Department of Dermatology, Sexually Transmitted Diseases and Leprosy, Govt. Medical College, Srinagar, University of Kashmir, Jammu and Kashmir
India
| How to cite this article: Hassan I, Anwar P, Bilquis S, Nabi S, Rasool F, Munshi I. Comparison of dermatoses seen in community health camps and a tertiary care centre in Kashmir. Indian J Dermatol Venereol Leprol 2014;80:214-220 |
Abstract
Background: Various environmental, socio-economic and geographical factors influence the pattern of dermatoses in an area. Observations made at tertiary dermatology centres may not reflect the actual pattern of dermatoses at the community level. Aims: To evaluate the pattern of dermatoses at community level and compare it with that at a tertiary centre. Methods: Cases were registered through community visits in block Hazratbal in Kashmir valley, once a week over a calendar year. The pattern of dermatoses observed was compared with that seen at the tertiary centre over the same period. Results: A total of 1065 community cases, with 1105 dermatoses, were compared with 4358 patients with 4466 dermatoses seen at the tertiary centre. Non-infectious dermatoses in each group were more common than infectious dermatoses (34.08% infectious dermatoses versus 65.97% non-infectious in community cases and 29.42% infectious dermatoses versus 70.58% non-infectious in hospital patients). Infectious cases were seen significantly more in the community (34.08%) than at the tertiary centre (29.42%). Among the infectious diseases, fungal infection was the most common and in the non-infectious group, pigmentary disorders were the most common, followed by acne and eczema. Conclusion : Infectious dermatoses were found statistically significantly more in community cases as compared to hospital patients while the opposite was the case with non-infectious dermatoses. The study emphasizes the need for providing frequent dermatology services to the community at the primary healthcare level so that the burden of dermatoses, especially infectious, may be reduced. Also, wider studies should be conducted in different regions in order to assess the actual magnitude of dermatological illnesses in the community.INTRODUCTION
Dermatological concerns are a common cause of morbidity in rural and urban areas of developing countries and account for a high proportion of visits to healthcare centres.
The pattern of dermatoses in a particular area is determined by many factors, such as geographical location including environmental and climatic factors, socio-economic condition of the people, literacy levels, psychological, cultural and racial factors, to mention a few. [1] Most of the knowledge presently available about various aspects of dermatological diseases is based on observations made and data collected from secondary and tertiary level hospitals. [2],[3]
The patterns of dermatoses observed at tertiary level centres may not necessarily represent those at the primary healthcare level. [4] In order to evaluate dermatoses in the community and look for any difference between the patterns of dermatoses at specialized tertiary care centres and at community level primary health centres, we conducted the present study by offering dermatological services at the primary care level in block Hazratbal of Srinagar district of Kashmir valley.
Background
Kashmir valley, with its plain as well as hilly and high altitude terrains, has different climatic and weather conditions from the rest of India. The maximum temperature during summers rarely goes beyond 37 degrees centigrade, but during winter drops down to sub-zero levels. This may have a bearing on the pattern of dermatological diseases. The reason for choosing block Hazratbal of Srinagar district for the study is that it consists of urban, sub-urban, rural, as well as hilly and tribal areas and thus represents diverse population groups.
METHODS
The study was conducted by the department of dermatology in collaboration with the community medicine department over a period of one year from October 2012 to September 2013. Dermatological consultation was provided by qualified dermatologists at all sub-centres, allopathic dispensaries, primary health centres and community health centres of the block through community visits once every week, thus providing services at the door step. Health camps were organized at centres located within localities, very close to the beneficiaries. As such, the access of patients to these health camps was not difficult and all of them could walk to attend the camps and on occasion home visits were undertaken. Consequently, most of the patients in the peripheral health camps presented of their own or were detected after proper screening in the health camps itself or during house to house visits. The medical block of Hazratbal is comprised of 12 sub-centres, 2 allopathic dispensaries and 2 primary health centres covering an estimated population of around one lakh and having urban, semi-urban, rural, hilly and tribal areas as well. The distance of these centres from the tertiary hospital ranges from 10-30 kilometres. The dermatology team visited the areas by turns and it was ensured that all health centres were visited frequently, at least three times and in different seasons of the year. On the first visit, all new cases were included and dermatological disease identified and on subsequent visits to the same area, only new dermatological diagnoses were recorded. Majority of the diagnosis were made by history and clinical examination. Those who required skin biopsy, patch testing and other specialized investigations were called to the tertiary hospital. Samples for KOH examination and fungal culture, pus/tissue for microscopic examination, culture/sensitivity and Tzanck smear etc., were collected on the spot, when needed and brought to the tertiary centre.
The comparison group comprised of patients seen by the same dermatology team over the same period in the out-patient department of our tertiary care centre. In the tertiary care centre, patients seek dermatological consultation of their own or are referred by other health care professionals/centres. At the end of the study, data was compiled, tabulated and analysed by statistical analysis using software statistical product and service solutions (SPSS) version 16 and windows 7. Chi square test (χ2😉 was used and significance taken as P < 0.05.
RESULTS
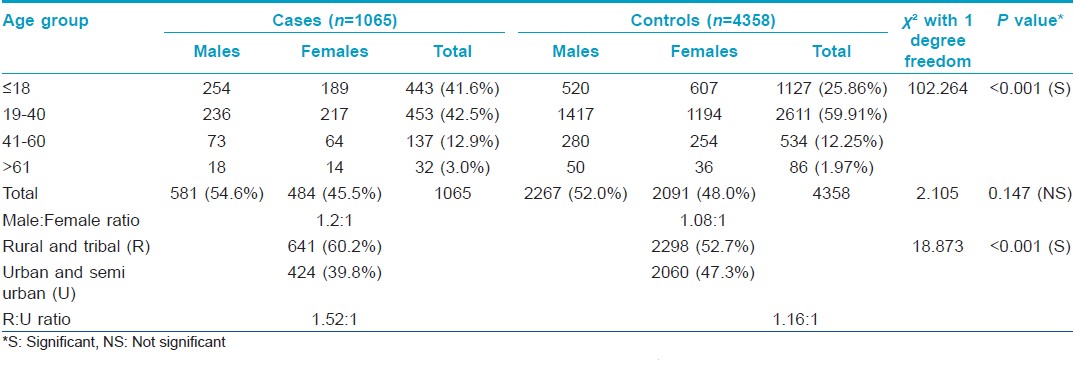
This prospective community based study involved 1065 cases registered during community visits over one year in block Hazratbal of Kashmir. There were 581 (54.6%) males and 484 (45.5%) females, with a male to female sex ratio of 1.2:1. Six hundred and forty one cases (60.2%) had rural and tribal background and 424 (40.0%) belonged to urban and semi-urban areas, making a rural to urban population ratio of 1.52:1.
The control group consisted of patients visiting the outpatient department of the tertiary centre during the same time period. A total of 4358 patients were registered, 2267 (52.0%) males and 2091 (48.0%) females, with a male to female ratio of 1.08:1. Of these, 2298 (52.7%) had a rural background and 2060 (47.3%) belonged to urban and semi-urban areas, with a rural to urban ratio of 1.16:1. The rural versus urban difference between community cases and hospital patients was statistically significant (P < 0.001), but not the sex difference (P < 0.147).
The number of children (age ≤ 18 years) seen in the community was 443 (41.6%) and 1127 (25.9%) in hospital patients, this difference was statistically significant (P = 0.001).
The age of patients in community cases ranged from 2 months to 75 years, with an average of 24.5 years (±SD 16.78) and in hospital patients from 2 months to 80 years, with an average age 26.3 years (±SD 14.68). Most of the patients were in the age group 19-40 years, 453 (42.5%) in community cases and 2611 (59.9%) in hospital patients, followed by children; the smallest number was in the age group >61 years. The demographic features in the two groups are elaborated in [Table - 1].
There were a total of 1105 dermatoses in the 1065 community cases and 4466 dermatoses in 4358 hospital based patients, as some patients presented with more than one dermatosis.
At the time of data compilation, dermatoses were divided into infectious and non-infectious groups.
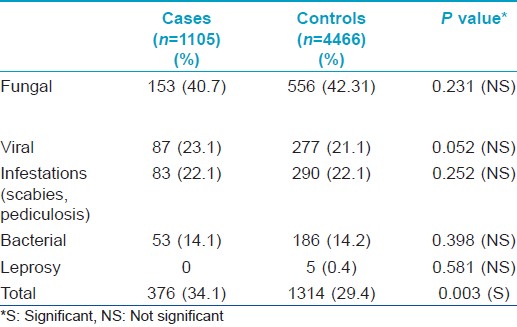
Infectious dermatoses, which included bacterial, viral, fungal and parasitic infestations such as scabies and pediculosis, were fewer than non-infectious dermatoses in each group. In the community, there were 376 (34.1%) cases of infectious dermatoses compared to 729 (65.0%) cases of non-infectious dermatoses. Similarly, 1314 (29.4%) infectious dermatoses were registered in the hospital patients compared to 3152 (70.6%) non-infectious dermatoses. The difference in the proportion of infectious cases between community and hospital was statistically significant (P = 0.003).
The difference between hospital and community with regards to each type of infection was not statistically significant. In the community, fungal infection was the most common type (40.7%), followed by viral infections (23.1%), infestations (22.0%) and bacterial infections (14.1%). In hospital patients, fungal infections were most common (42.3%), followed respectively by infestations (22.1%), viral infections (21.1%) and bacterial infections (14.2%).
Five cases of leprosy (0.38%), 2 indeterminate and 3 lepromatous, were detected in non-locals in the hospital. This is summarized in [Table - 2].
In contrast to infectious dermatoses, more non-infectious dermatoses were found in hospital patients than in the community, 3152 (70.58%) in the hospital and 729 (65.97%) in the community, a statistically significant difference (P = 0.003).
Among non-infectious dermatoses, in the community the five most common dermatoses were pigmentary disorders in 156 (14.18%), followed by acne vulgaris in 109 (9.9%), eczema in 98 (8.9%), papulo-squamous disorders in 77 (7.0%) and hair disorders in 41 (3.7%). Similarly among the hospital patients, the five most common dermatoses were pigmentary disorders in 652 (15.0%), acne vulgaris in 443 (10.0%), eczema in 355 (8.0%), hair disorders in 355 (7.95%) and papulo-squamous disorders in 332 (7.4%).
The 10 most common dermatoses in descending order, when community and hospital cases were considered together, were pigmentary disorders (hypo- and hyperpigmentation), acne vulgaris, various forms of endogenous and exogenous eczemas, papulo-squamous disorders (psoriasis, lichen planus etc), hair disorders, rosacea and steroid-induced rosacea, insect bite reactions, psycho-neuro-cutaneous disorders, photodermatoses and urticaria. Hypopigmented disorders included vitiligo, post-inflammatory hypopigmentation, pityriasis alba and naevi among others. Hyperpigmentary disorders included melasma, post inflammatory hyperpigmentation and naevi, among others [Table - 3].
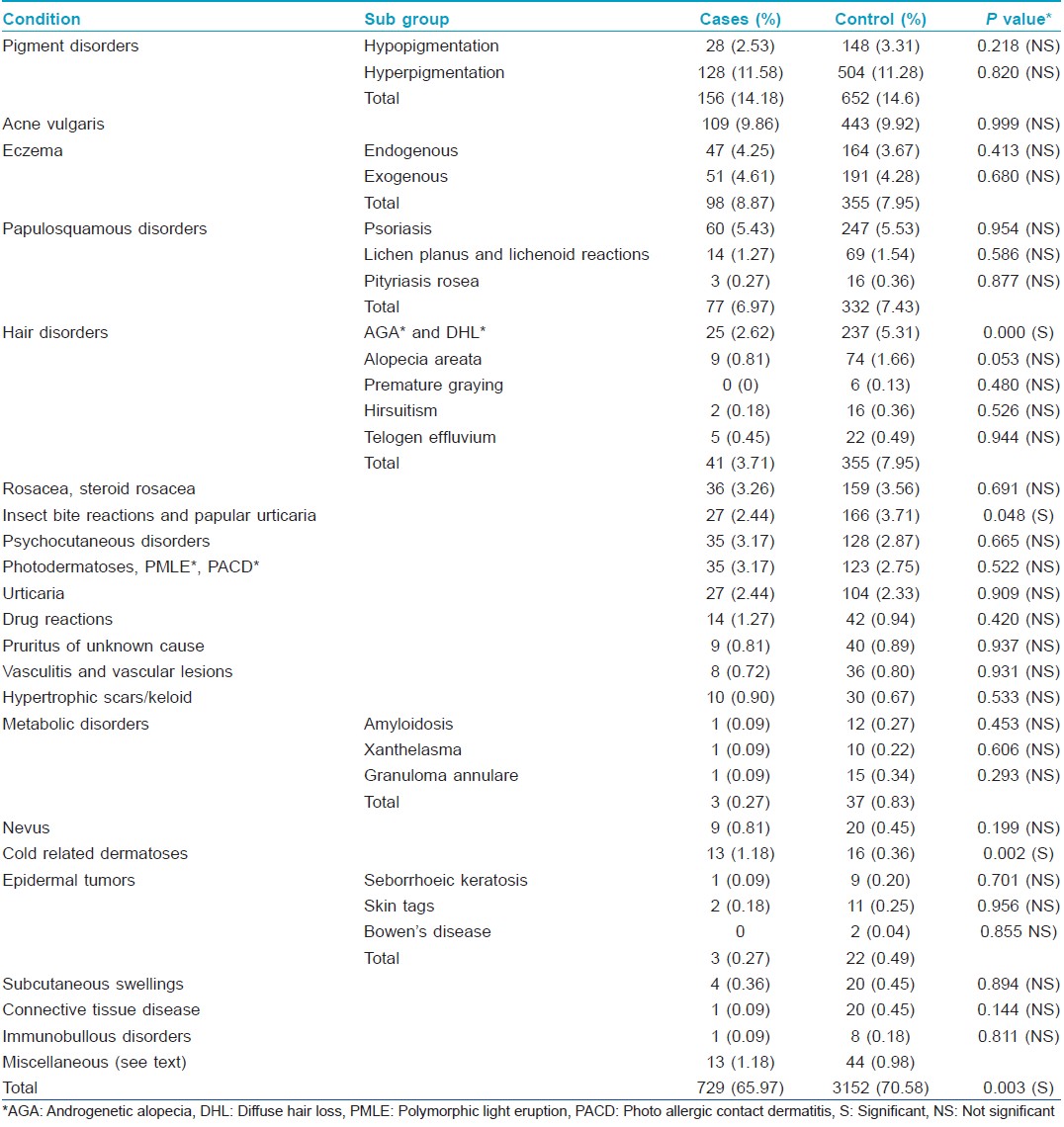
The difference between community and hospital cases was not statistically significant for most of the non-infectious dermatoses, except diffuse hair loss, androgenetic alopecia, insect bite reactions and cold related dermatoses. Alopecia was found more frequently in the hospital group (5.3%) than the community cases (2.6%), ( P ≤ 0.001). Similarly, insect bite reactions occurred in 3.7% of hospital patients versus 2.4% of community cases (P = 0.048). Cold related dermatoses were found more frequently in the community (1.2%) than in the hospital patients (0.4%) (P = 0.002).
Among the infrequently encountered miscellaneous dermatoses in the community, we found granulomatous cheilitis and perforating dermatoses in 2 patients and ichthyosis, striae, xerosis, prurigo, Dupuytrens contracture, pearly penile papules, annular erythemas, acrodermatitis enteropathica and pellagra in 1 patient each. None of the community cases had keratosis pilaris, miliaria, pseudopelade of Brocq, pitted keratolysis and pityriasis lichenoides chronica.
Among the hospital patients, striae were found in 8 patients, perforating dermatoses in 6, granulomatous cheilitis, ichthyosis and miliaria in 4 each and xerosis, prurigo, Dupuytrens contracture, pearly penile papules, annular erythemas, keratosis pilaris, pseudopelade of Brocq, pitted keratolysis and pityriasis lichenoides chronicain 2 each. None of the hospital patients had acrodermatitis enteropathica or pellagra.
There was no statistically significant difference between hospital and community cases with regard to the miscellaneous dermatoses.
DISCUSSION
The male preponderance in both hospital and community groups taken together, was in accordance with some studies [5],[6] and in contrast to others, where female predominance was noted. [1],[7],[8] This contrast may depend on the institutional set up where the study is conducted.
In the community, there were a greater proportion of cases from rural and tribal background (60.2%) because we had a good turn-out of patients at the health camps conducted in rural areas of the block as compared to the urban and semi-urban areas probably because the urban sections have easy access to tertiary care. Interestingly, patients from a rural background (52.7%) outnumbered those from urban areas (47.3%) in the hospital group, too probably because urban residents avoid the crowded forenoon clinics preferring to visit the centre during evening hours.
A larger proportion of children were seen in the community probably because of the convenience of bringing children to primary care centres near home without having to miss school rather than travelling to a distant tertiary centre. This emphasizes the importance of dermatology outreach clinics in addressing paediatric dermatoses.
The age distribution of patients in our study was consistent with previous reports. [1],[6],[7],[8],[9]
Patients in these peripheral stations and difficult to reach terrains usually do not seek any specialized treatment for dermatological diseases, or are provided preliminary treatment by non-specialists. This is because of long distances from the health centres in some cases, but mostly because of non-availability of specialized dermatology services. In Government run health centres, the services are provided free of cost. Medical facilities in these areas are otherwise provided by traditional practitioners as well as those trained in allopathic medicine such as pharmacists etc.
Had we not conducted health camps and house to house visits and on occasion distributed free medicines, we would have missed many cases and the true prevalence data of dermatological diseases from the community would not emerge.
In accordance with other studies, [5],[10],[11] there were fewer infectious dermatoses than non-infectious dermatoses in both the community and the hospital patient groups probably because of good hygienic and sanitary conditions, cleaning habits and health awareness, more so in the urban population than rural and tribal.
Infectious dermatoses including bacterial, viral, fungal and parasite infestations were commoner in the community than in hospital cases. This may be because of lesser awareness about hygiene, infections and infectious agents among the community cases. Non-availability of dermatology services nearby, poverty and household overcrowding also may contribute to this difference. The higher proportion of infectious dermatoses among community cases found in our study is in accordance with some other studies. [1],[6],[8],[9],[12],[13],[14],[15]
The difference in the proportion of each type of infection between community and hospital in our study was not however, statistically significant. Fungal infections were the commonest infection detected in our study, as in some others, [1],[5],[6],[8],[9],[11],[14],[16] whereas bacterial infections were found predominantly in some, [10],[13],[17],[18] and parasitic infestations in other studies. [12]
Non-infectious dermatoses constituted the major type of dermatoses in each group. In agreement with various other studies in the literature, the most common non-infectious dermatoses included eczema, pigment disorders, acne and papulo-squamous disorders, although with some variations in the order of occurrence in each study. [1],[5],[6],[7],[8],[9],[11],[16],[18]
Hair disorders were important non-infectious dermatoses in our study, as a number of different conditions such as alopecia areata, androgenetic alopecia, diffuse hair loss, hirsutism and premature greying were clubbed together in this group.
There were fewer cases of diffuse hair loss and androgenetic alopecia in the community probably because the population was younger and there might be less concern about cosmetic appearance. Unexpectedly, insect bite reactions were fewer in the community cases and may be because insect bite reactions are considered normal, seasonal, harmless and natural phenomena not requiring medical advice. Cold related dermatoses were found more frequently in the community because more rural and tribal people were encountered in community visits.
CONCLUSION
This study emphasizes the need for providing frequent dermatology services to the community at primary health care level so that the burden of dermatoses, especially infectious dermatoses, may be reduced in the community. This can be accomplished by spreading awareness among the masses about different dermatoses, various aspects of personal hygiene and sanitation conditions and also by provision of frequent medical consultations at the primary care levels. Larger studies should be conducted in different regions in order to assess the actual magnitude of dermatological concerns in the community at the grass root level.
ACKNOWLEDGMENTS
We acknowledge the help and support provided by the staff of all health centres of block Hazratbal.
| 1. |
Kuruvilla M, Sridhar KS, Kumar P, Rao G. Pattern of skin diseases in Bantwal Taluq, Dakshina Kannada. Indian J Dermatol Venereol Leprol 2000;66:247-8.
[Google Scholar]
|
| 2. |
Mehta TK. Pattern of skin diseases in India. Indian J Dermatol Venereol Leprol 1962;28:134-9.
[Google Scholar]
|
| 3. |
Dayal SG, Gupta GD. A cross section of skin diseases in Bunelkhand region, UP. Indian J Dermatol Venereol Leprol 1977;43:258-61.
[Google Scholar]
|
| 4. |
Mahalingam C. Prevalence of Dermatoses in Tribal population of Kalrayan Hill (South Arcot District). Indian J Dermatol Venereol Leprol 1986;52:213-5.
[Google Scholar]
|
| 5. |
Rao GS, Kumar SS, Sandhya. Pattern of skin diseases in an Indian village. Indian J Med Sci 2003;57:108-10.
[Google Scholar]
|
| 6. |
Kuruvila M, Dubey S, Gahalaut P. Pattern of skin diseases among migrant construction workers in Mangalore. Indian J Dermatol Venereol Leprol 2006;72:129-32.
[Google Scholar]
|
| 7. |
Shenoi SD, Davis SV, Rao S, Rao G, Nair S. Dermatoses among paddy field workers-A descriptive, cross-sectional pilot study. Indian J Dermatol Venereol Leprol 2005;71:254-8.
[Google Scholar]
|
| 8. |
Grover S, Ranyal RK, Bedi MK. A cross section of skin diseases in rural Allahabad. Indian J Dermatol 2008;53:179-81.
[Google Scholar]
|
| 9. |
Das S, Chatterjee T. Pattern of skin diseases in a peripheral hospital's skin OPD: A study of 2550 patients. Indian J Dermatol 2007;52:93-5.
[Google Scholar]
|
| 10. |
Das A, Halder S, Das J, Mazumdar G, Biswas S, Sarkar JN. Dermatologic disease pattern in an urban institution in Kolkata. Indian J Dermatol 2005;50:22-4.
[Google Scholar]
|
| 11. |
Jaiswal AK. Ecologic perspective of dermatologic problems in North Eastern India. Indian J Dermatol Venereol Leprol 2002;68:206-7.
[Google Scholar]
|
| 12. |
Bhatia V. Extent and pattern of paediatric dermatoses in rural areas of central India. Indian J Dermatol Venereol Leprol 1997;63:22-5.
[Google Scholar]
|
| 13. |
Anand IS, Gupta S. A profile of skin disorders in children in Saurasthra. J Indian Med Assoc 1998;96:245-6.
[Google Scholar]
|
| 14. |
Yasmeen N, Khan MR. Spectrum of common childhood skin disease: A single centre experience. J Pak Med Assoc 2005;55:60-3.
[Google Scholar]
|
| 15. |
Behl PN, Mohantay KC, Banerjee S. Ecological study of skin diseases in Delhi area. Indian J Dermatol Venereol Leprol 1979;45:260.
[Google Scholar]
|
| 16. |
Kuruvila M, Shaikh M, Kumar P. Pattern of dermatoses among inmates of district prison- Mangalore. Indian J Dermatol Venereol Leprol 2002;68:16-8.
[Google Scholar]
|
| 17. |
Balai M, Khare AK, Gupta LK, Mittal A, Kuldeep CM. Pattern of pediatric dermatoses in a tertiary care centre of South West Rajasthan. Indian J Dermatol 2012;57:275-8.
[Google Scholar]
|
| 18. |
Das KK. Pattern of dermatological diseases in Guwahati Medical College and Hospital Guwahati. Indian J Dermatol Venereol Leprol 2003;69:16-8.
[Google Scholar]
|
Fulltext Views
2,091
PDF downloads
950





