Translate this page into:
Comparison of oral itraconazole given for two days plus topical tacrolimus versus topical tacrolimus for maintenance treatment of seborrheic dermatitis in Vietnam
Corresponding author: Dr. Hien Thi Thu Do, National Hospital of Dermatology and Venereology, Hanoi, Vietnam. hienphuonglinh@yahoo.com.
-
Received: ,
Accepted: ,
How to cite this article: Do HTT, Le TV, Kanekura T. Comparison of oral itraconazole given for two days plus topical tacrolimus versus topical tacrolimus for maintenance treatment of seborrheic dermatitis in Vietnam. Indian J Dermatol Venereol Leprol 2023;89:748-50
Dear Editor,
The efficacy of a combined treatment with topical tacrolimus and oral itraconazole has not been investigated in Vietnamese patients with moderate or severe seborrheic dermatitis. In this study, we assessed the effectiveness of a combination therapy with oral itraconazole and topical tacrolimus in the treatment of moderate or severe seborrheic dermatitis. Then we compared the effectiveness of two maintenance therapies in patients who did or did not receive additional maintenance treatment with oral itraconazole from week 5.
The sample size was calculated using World Health Organization’s formula for comparative studies, assuming that the rate of complete or good improvement in the group who did and did not receive maintenance therapy with oral itraconazole is 90 and 50%, respectively. 1 In order to obtain 80% power at 0.05 level of significance, a sample size of 62 patients was required. The inclusion criteria included a diagnosis of moderate to severe seborrheic dermatitis and age ≥18 years. Exclusion criteria included prior treatment (2-week topical and 4-week systemic treatment) for seborrheic dermatitis and allergy to oral itraconazole or tacrolimus.
In the first week, all 62 patients were treated with oral itraconazole (200 mg/day) (Figure 1). At week 5, the patients were randomly allocated to two groups by assigning equal number of ballots to each group and drawing a ballot for each patient. Group 1 underwent maintenance therapy with oral itraconazole (200 mg/day for the first two days of the next three months) while group 2 did not. Throughout the study, all patients in the two groups were treated with topical tacrolimus once at night daily or once at night twice weekly if the symptoms improved. They were also instructed to use a shampoo containing a nonsteroidal anti-inflammatory agent with anti-fungal properties and moisturizer.
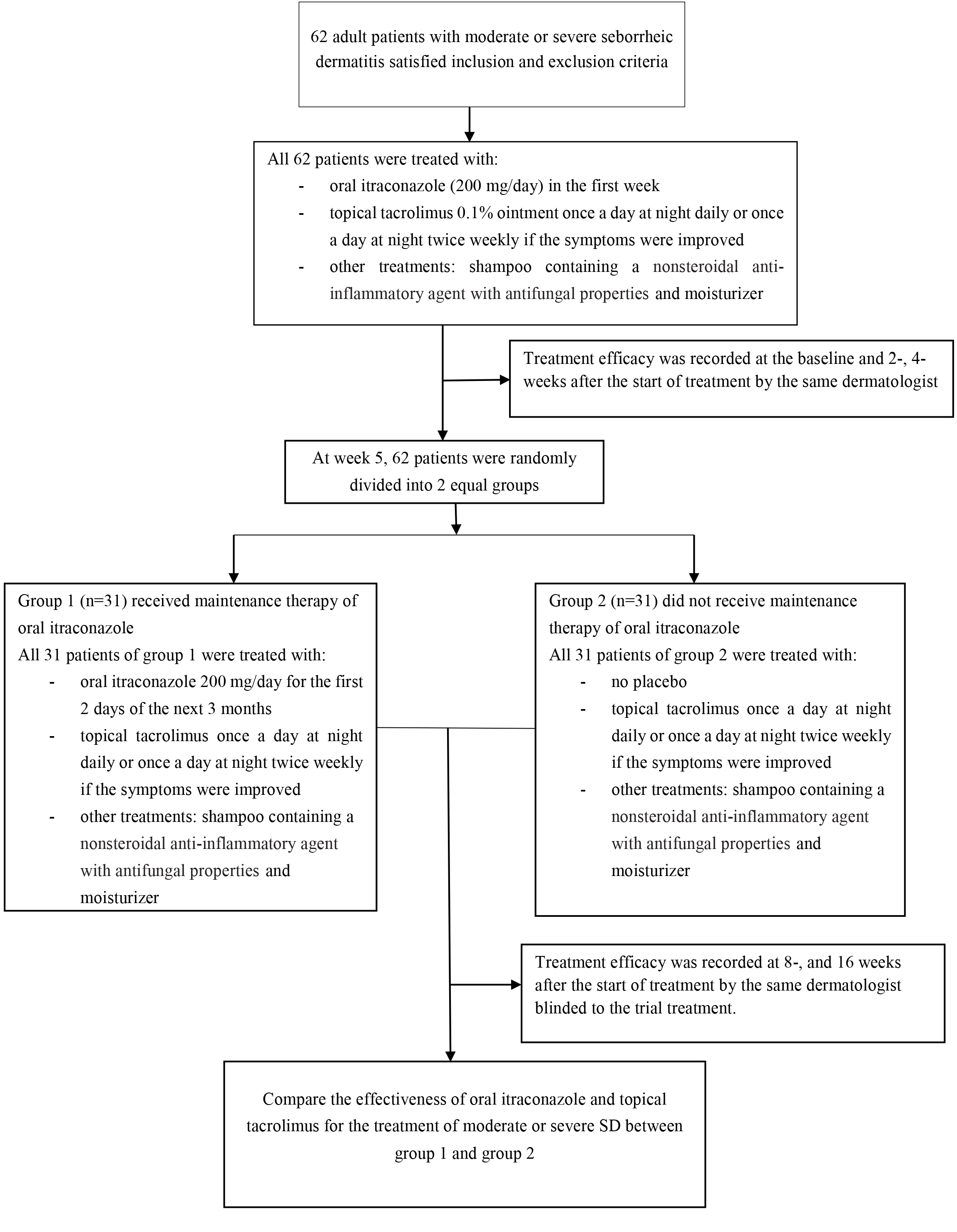
- Study flowchart
Four clinical parameters, i.e., erythema, scaling, burning and itching were assessed using the 4-point Shemer scale 2 where 0 = absent, 1 = mild, 2 = moderate, 3 = severe. The total score for the four parameters ranged from 0 to 12. A total score of at least 5 was required for a diagnosis of moderate to severe seborrheic dermatitis. Clinical improvement was recorded as complete (score = 0), good (score 1 or 2), moderate (score 3 or 4), and none (score 5 or higher). Recurrence was recorded when the total score of the four parameters rose twice as high as the total score obtained after the first two weeks of treatment. Statistical analysis was performed using Stata 20.0 statistical software.
This study was approved by the ethics committee of the National Hospital of Dermatology and Venereology and Hanoi Medical University. Prior informed consent was obtained from all participants.
At two and four weeks after the start of treatment with oral itraconazole and topical tacrolimus, all 62 patients experienced improvement in seborrheic dermatitis which was statistically significant. Their mean total score for erythema, scaling, burning and itching fell from 7.44 at the baseline to 1.76 after two weeks and 1.79 after four weeks. At two weeks, seven patients had improved completely, 44 showed good and 11 patients, moderate improvement. After our 4-week initial treatment, eight patients achieved complete, 40 patients good and 14 patients experienced moderate improvement [Figure 2]. Treatment did not fail to show response in any of the 62 patients.
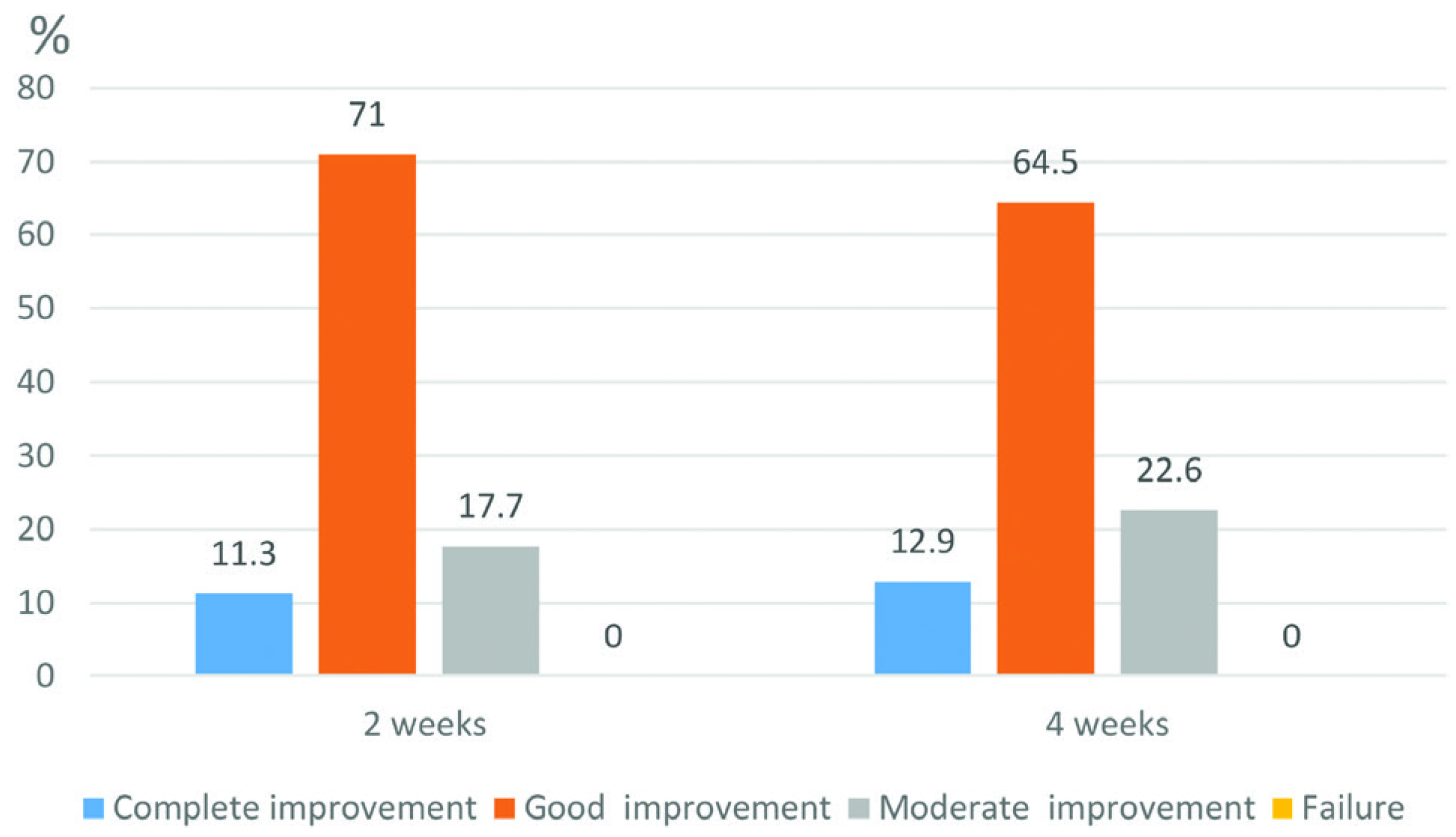
- Clinical improvement after 2- and 4-week initial treatment with oral itraconazole and topical tacrolimus
At eight weeks, of the 31 group 1 patients, 10 showed complete and 13 good improvement; among group 2, only two improved completely and nine experienced good improvement. Treatment for eight weeks failed in five group 2 patients; all group 1 patients responded. The inter-group difference was statistically significant (P = 0.006) [Figure 3].
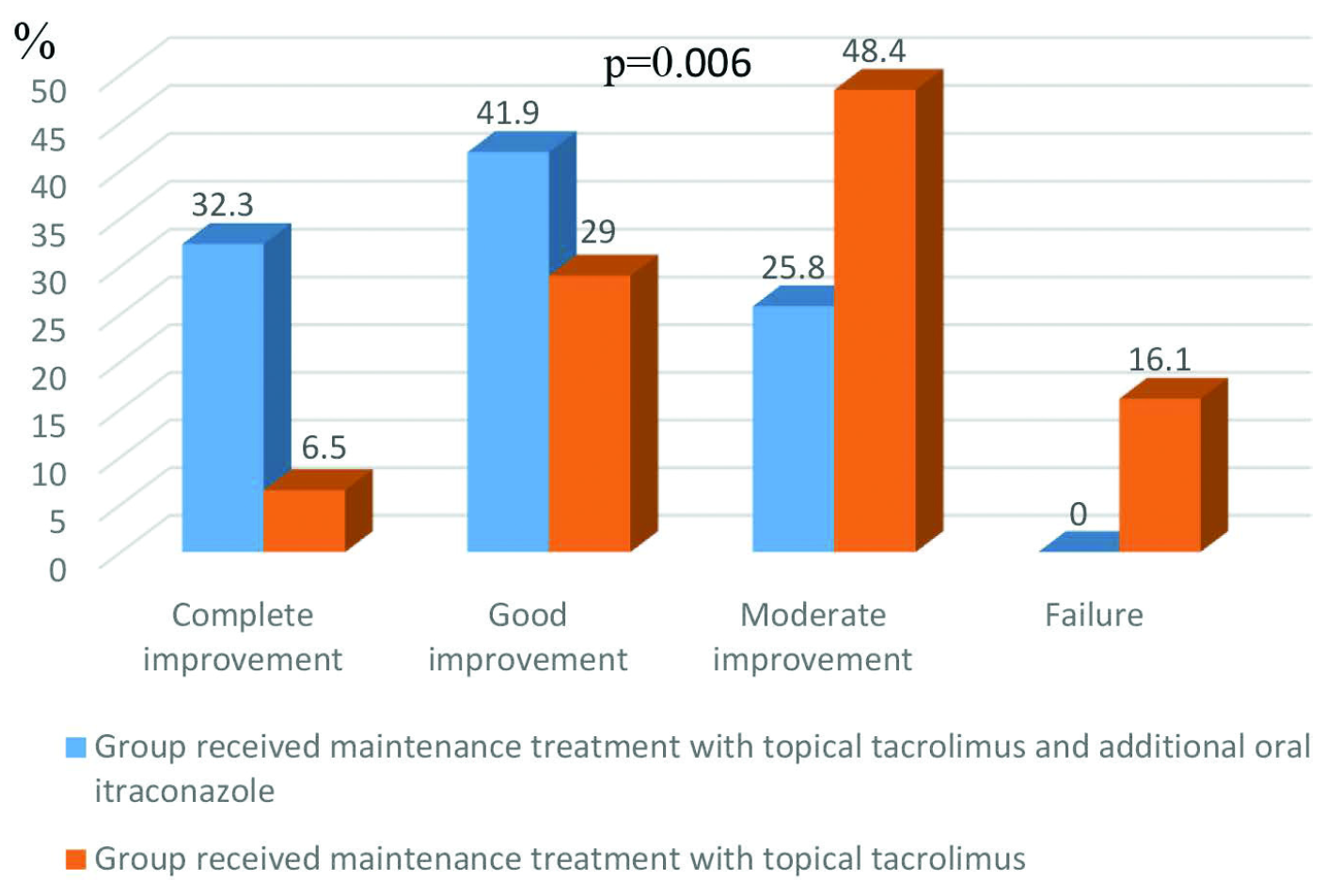
- The effectiveness of 2 maintenance therapies seen after 8 weeks
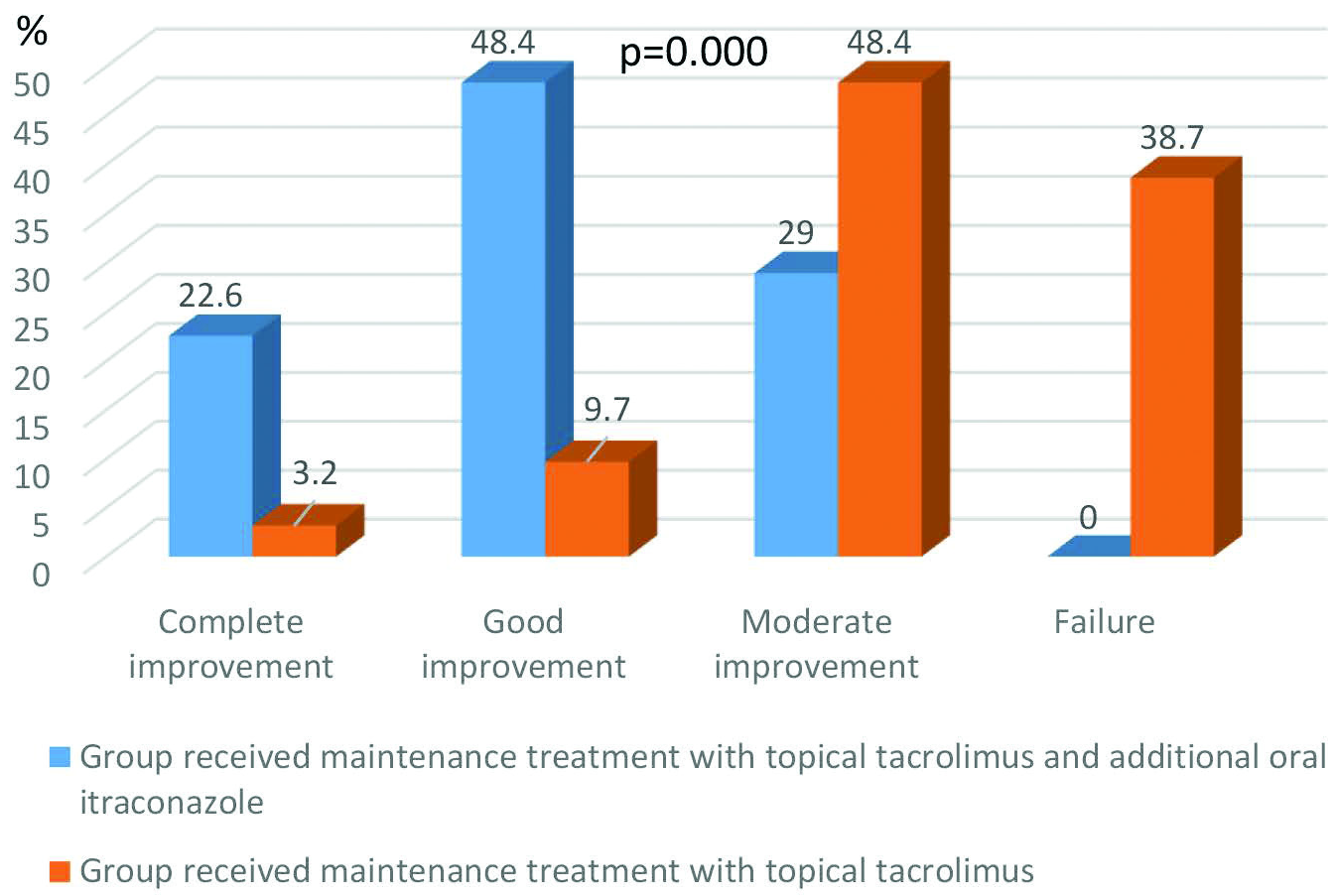
- The effectiveness of 2 maintenance therapies seen after 16 weeks
At 16 weeks also, the inter-group differences were statistically significant (P < 0.001) [Figure 4].
Among group 1, four patients (12.9%) experienced seborrheic dermatitis recurrence at eight weeks; eight (25.8%) did after week 16. The recurrence rates in group 1 were significantly lower than in group 2 where 13 (41.9%) and 22 patients (71%) suffered recurrence at 8- and 16 weeks, respectively. The inter-group difference was significant (P = 0.021 at 8 weeks and P < 0.001 at 16 weeks).
Unlike previous studies, the present study was a comparative one. Though investigations to identify Malassezia spores in the skin lesions were conducted in all patients at baseline, they were not repeated at all evaluation times and hence were not included in the analysis, which was a limitation.
In conclusion, initial treatment with topical tacrolimus and oral itraconazole was beneficial in adult patients with moderate to severe seborrheic dermatitis. Subsequent maintenance therapy with topical tacrolimus and oral itraconazole helped to ameliorate the severity of seborrheic dermatitis and reduced the seborrheic dermatitis recurrence rate.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Efficacy of oral itraconazole in the treatment and relapse prevention of moderate to severe seborrheic dermatitis: A randomized, placebo-controlled trial. Am J Clin Dermatol. 2015;16:431-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of moderate to severe facial seborrheic dermatitis with itraconazole: An open non-comparative study. Isr Med Assoc J. 2008;10:417-8.
- [PubMed] [Google Scholar]





