Translate this page into:
Complete form of pachydermoperiostosis with cutis verticis gyrata resulting from the SLCO2A1 gene mutation
2 Department of Genetic Medicine, School of Life Science, Sichuan University, Sichuan, China
Correspondence Address:
Xian Jiang
37, Guoxue Xiang, Wuhou District, Chengdu, 610041
China
| How to cite this article: Li X, Hao D, Li-Ling J, Jiang X. Complete form of pachydermoperiostosis with cutis verticis gyrata resulting from the SLCO2A1 gene mutation. Indian J Dermatol Venereol Leprol 2019;85:681 |
Sir,
Pachydermoperiostosis, also known as primary hypertrophic osteoarthropathy, is a rare genetic disease characterized by pachydermia, periostosis and digital clubbing. Mutations in the 15-hydroxy-prostaglandin dehydrogenase (HPGD)gene and solute carrier organic anion transporter family member 2A1 (SLCO2A1) gene have been identified to cause pachydermoperiostosis. We herein represent a rare case of pachydermoperiostosis with evident cutis verticis gyrata caused by the SLCO2A1 gene mutation.
A 19-year-old Tibetan man was referred to our hospital for enlargement of his limbs and skin creases of 4-years duration with mild to moderate pain in the ankle and knee joints after repetitive use. He had a past history of hematemesis 8 months before and was otherwise healthy. He was born to healthy nonconsanguineous parents and one of his seven siblings had the same clinical presentation [Figure - 1]. Upon examination, the patient's physical and mental development were normal. He had exaggerated facial skin thickening and furrows as well as evident cutis verticis gyrata, which led to blepharoptosis and obvious nasolabial folds, giving him an appearance of aging prematurely [Figure - 2]. Associated seborrhea and acne were also seen. His upper and lower extremities, as well as wrist, knee and ankle joints were all enlarged but had normal joint movements. Digital clubbing was also observed [Figure - 3].
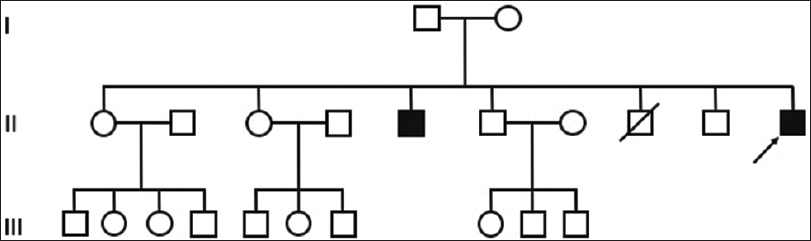 |
| Figure 1: Pedigree of the family |
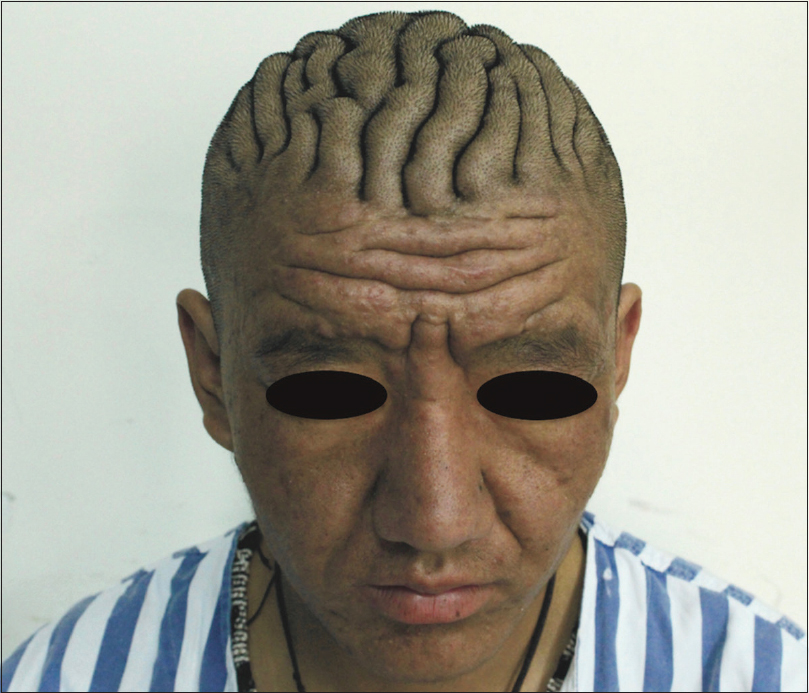 |
| Figure 2: Thickening and furrows of the facial skin with evident cutis verticis gyrata |
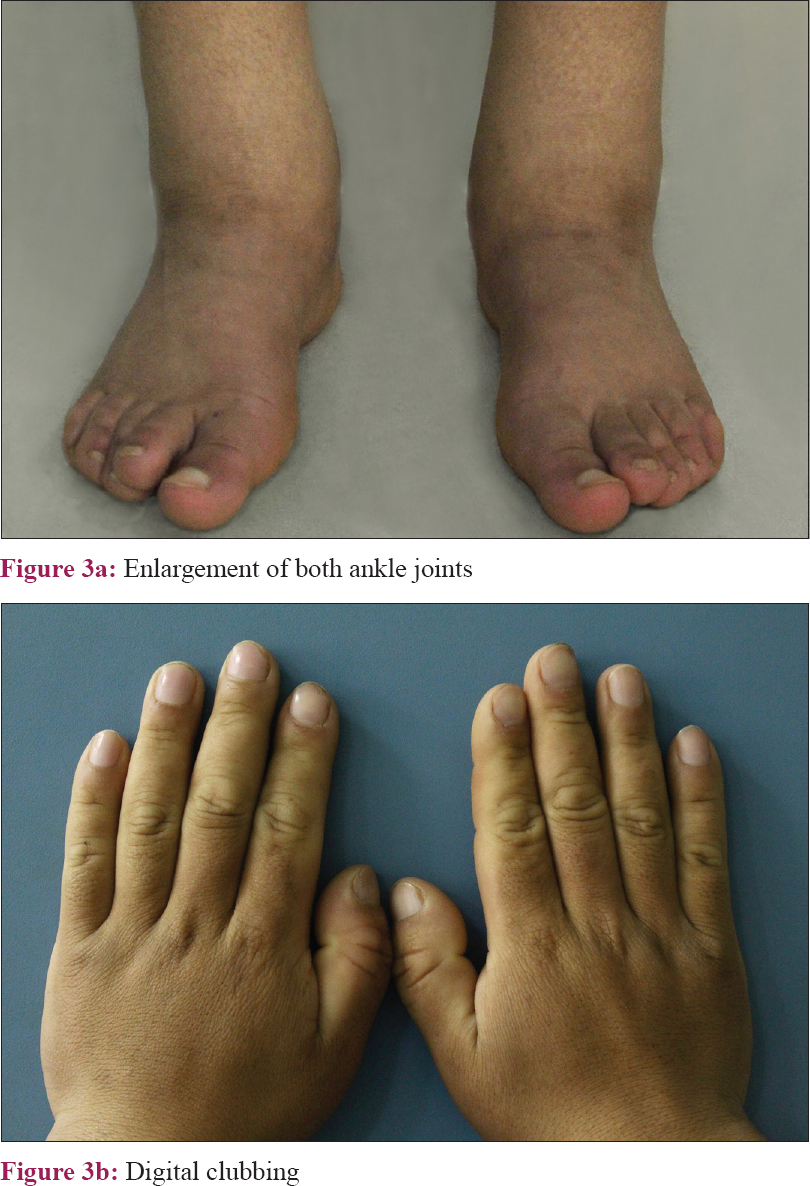 |
| Figure 3: |
Hemogram revealed mild microcytic hypochromic anemia, and insulin-like growth factor-1 level was 100.39 ng/mL (normal range: 138.8–353.1 ng/mL). X-ray of the extremities demonstrated enlarged diaphysis, soft tissue swelling and periosteal proliferation [Figure - 4]. Biochemical parameters, antinuclear antibodies, growth hormone level, thyroid function, echocardiography and computed tomography scan of the chest were unremarkable. Urinary prostaglandin E2 level was unavailable. Furthermore, gastroscopy revealed hypertrophic gastric folds with multiple ulcers in gastric antrum and biopsy of the gastric mucosa showed mild and chronic inflammation and intestinal metaplasia. Colonoscopy findings were normal. Skin biopsy from the scalp showed mucin deposition and hypertrophic sebaceous glands [Figure - 5] and [Figure - 6].
 |
| Figure 4: Radiograph of the right tibia showing enlargement of the diaphysis (black asterisks), soft tissue swelling (white asterisks) and periosteal proliferation (arrow) |
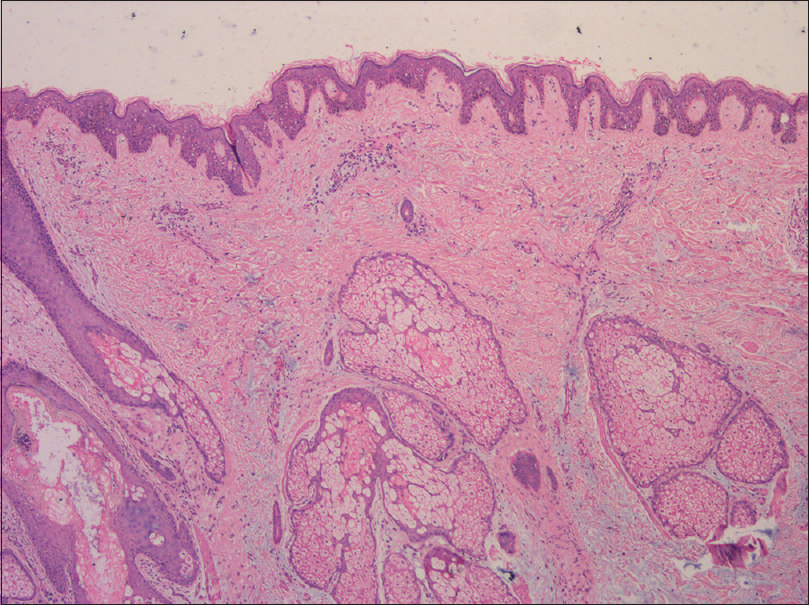 |
| Figure 5: Biopsy of the scalp showing mucin deposition and hypertrophic sebaceous glands (hematoxylin and eosin, ×40) |
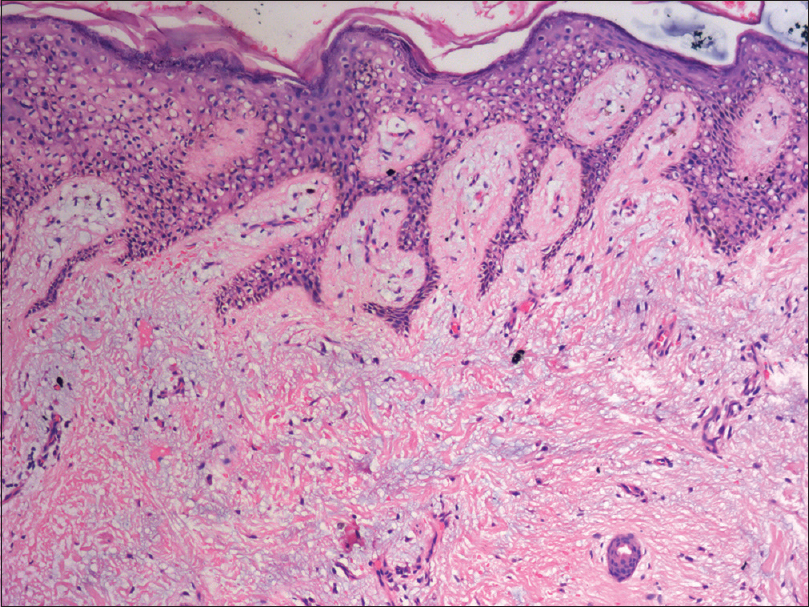 |
| Figure 6: Biopsy of the scalp showing mucin deposition (hematoxylin and eosin, ×100) |
A clinical diagnosis of complete form of pachydermoperiostosis was made for this patient because he manifested all three major features (pachydermia, periosteal proliferation and digital clubbing). To confirm the diagnosis, we carried out whole-exome sequencing after obtaining the patient's informed consent. Results showed a homozygous nonsense mutation c.1807C>T/p.R603* in the SLCO2A1 gene [Figure - 7], which is in agreement with our diagnosis. Further gene detection for his parents and affected brother was recommended but they refused it.
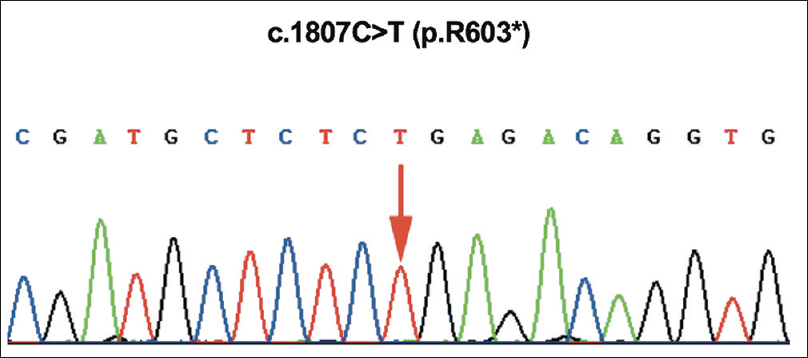 |
| Figure 7: Whole-exome sequencing revealed a homozygous nonsense mutation c.1807C>T/p.R603* in the SLCO2A1 gene |
Hypertrophic osteoarthropathy was described by Friedreich as “hyperostosis” in 1868. In 1935, Touraine, Solente and Gole introduced pachydermoperiostosis as a primary entity to differentiate it from the secondary hypertrophic osteoarthropathy, which is associated with intrathoracic disease and malignancy. There are three forms of pachydermoperiostosis: complete form with both skin and skeletal changes; incomplete form with skeletal changes but without pachydermia and “forme fruste” with pachydermia but minimal or no skeletal changes. Other associated symptoms include polyarthritis, blepharoptosis, seborrhea, acne and hyperhidrosis. Anemia, watery diarrhea, gastric hypertrophy and peptic ulcer have also been reported.[1]
Both autosomal recessive inheritance (HPGD mutation) and autosomal-dominant transmission (SLCO2A1 mutation) have been reported in pachydermoperiostosis cases. Clinical phenotypes of HPGD-deficient and SLCO2A1-deficient individuals are similar but SLCO2A1 mutation tends to affect males with disease onset peaking at puberty. The SLCO2A1 gene encodes prostaglandin transporter that is responsible for cellular uptake of prostaglandin E2, while the HPGD gene encodes 15-hydroxyprostaglandin dehydrogenase which catabolizes prostaglandin E2. Therefore, either HPGD or SLCO2A1 deficiency can contribute to chronically elevated prostaglandin E2 levels, explaining the clinical findings of skeletal and skin changes, as prostaglandin E2 can stimulate the activities of osteoclasts, osteoblasts and fibroblasts. So far, we found that more than 40 mutations in SLCO2A1 had been reported to cause pachydermoperiostosis.[2] c.1807C>T/p.R603* was previously described by Niizeki et al. in a case of compound heterozygous mutations, though no homozygous mutation had been reported earlier.[3]
Several treatments have been proposed to treat pachydermoperiostosis. Nonsteroidal antiinflammatory drugs, systemic corticosteroids, colchicine and bisphosphonates can be used to reduce the pain due to osteoarthropathy. Etoricoxib, which inhibits cyclo-oxygenase-2, was reported to improve both the swelling of joints and the facial coarsening.[4] None of these medications were attempted in our patient as he had gastric ulcers and only mild arthralgia at rest. There have also been successful cases in which patients' facial appearance were improved by plastic surgery and botulinum toxin injection.[5],[6] However, surgery may not be an option until the disease becomes quiescent.
In conclusion, we report a case of pachydermoperiostosis with prominent cutis verticis gyrata. The diagnosis was based on clinical and radiologic findings and further confirmed by gene analysis. A homozygous c.1807C>T mutationin the SLCO2A1 gene responsible for pachydermoperiostosis was identified.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Zhang Z, He JW, Fu WZ, Zhang CQ, Zhang ZL. Mutations in the SLCO2A1 gene and primary hypertrophic osteoarthropathy: A clinical and biochemical characterization. J Clin Endocrinol Metab 2013;98:E923-33.
[Google Scholar]
|
| 2. |
Lee S, Park SY, Kwon HJ, Lee CH, Kim OH, Rhee Y, et al. Identification of the mutations in the prostaglandin transporter gene, SLCO2A1 and clinical characterization in Korean patients with pachydermoperiostosis. J Korean Med Sci 2016;31:735-42.
[Google Scholar]
|
| 3. |
Niizeki H, Shiohama A, Sasaki T, Seki A, Kabashima K, Otsuka A, et al. The novel SLCO2A1 heterozygous missense mutation p.E427K and nonsense mutation p.R603* in a female patient with pachydermoperiostosis with an atypical phenotype. Br J Dermatol 2014;170:1187-9.
[Google Scholar]
|
| 4. |
Li ZT, Wang D, Wang S. Successful treatment of pachydermoperiostosis with etoricoxib in a patient with a homozygous splice-site mutation in the SLCO2A1 gene. Br J Dermatol 2016.
[Google Scholar]
|
| 5. |
Liu CY, Zhang YF. Images in clinical medicine. Pachydermoperiostosis. N Engl J Med 2014;370:1930.
[Google Scholar]
|
| 6. |
Ghosn S, Uthman I, Dahdah M, Kibbi AG, Rubeiz N. Treatment of pachydermoperiostosis pachydermia with botulinum toxin type A. J Am Acad Dermatol 2010;63:1036-41.
[Google Scholar]
|
Fulltext Views
6,512
PDF downloads
2,556





