Translate this page into:
Complications of laser and light-based devices therapy in patients with skin of color
Correspondence Address:
B S Chandrashekar
5/1, 4th Main MC Layout, Near Veeresh Theatre, Vijay Nagar, Bengaluru - 560 040, Karnataka
India
| How to cite this article: Chandrashekar B S, Shenoy C, Madura C. Complications of laser and light-based devices therapy in patients with skin of color. Indian J Dermatol Venereol Leprol 2019;85:24-31 |
Abstract
Lasers and light-based devices are indispensable to an aesthetic dermatology practice. The growing popularity of lasers has been matched by a sharp increase in the incidence of complications. The Indian skin with its high melanin content is more prone to injury and careful setting of laser parameters, early detection of complications and immediate therapy are vital to avoiding permanent sequelae. We review the various complications that occur during laser procedures and their management.
Introduction
A laser complication has been defined as “any undesirable effect that occurs with laser treatment, even if expected.”[1] It is mandatory that the laser physician be familiar with the basic principles of lasers, laser–tissue interactions as well as the device being used in order to minimize complications. The principle of selective photothermolysis proposed by Anderson and Parrish has revolutionized laser therapy and has enabled technology that confines tissue injury to specifically targeted chromophores within the skin.[2] Advances in laser technology have resulted in the development of more effective and safer lasers. Laser physicians need to constantly update themselves to utilize these modern laser and light-based devices that have the potential to produce new and unfamiliar complications.
Indian skin ranges from type IV to VI on the Fitzpatrick skin type scale and is more pigmented in comparison to the Caucasian or Oriental skin types owing to presence of greater amounts of epidermal melanin and larger melanosomes.[3] This makes it more vulnerable to post inflammatory hyperpigmentation following laser treatment.[3] Pigmentary changes are the main manifestation of photoaging in the Indian skin and erythema is usually masked by the darker tone. The degree of wrinkling is not as marked as in Caucasians[4] and melanoma and nonmelanoma skin cancers are less common in Indians. A cavalier attitude toward sun exposure and avoidance of sunscreens is usual in India, and therefore, counseling patients before laser treatment is mandatory.
Complications Due to Lasers and Light-Based Devices
Complications occurring due to laser and light-based devices can be classified into two broad categories: operator-dependent and patient-dependent. Operator-dependent variables include faulty parameters and poor technique (such as the handpiece not being perpendicular to the skin, placing the probe too close or too far from the skin while operating the laser, and not using adequate protection for operating personnel and patients). Patient dependent variables include the skin type, the type of lesion, hormonal status (in female patients undergoing laser hair reduction), inadequate or improper sunscreen application and recent tanning.
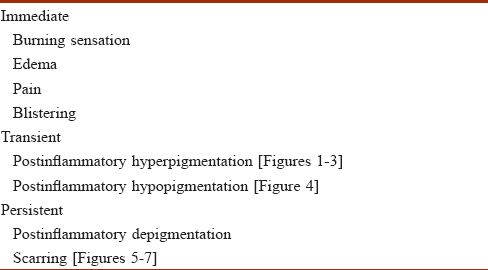
We propose that the complications of laser procedures may be classified as immediate (up to 7 days), transient (1–6 weeks) and persistent (after 6 weeks) [Table - 1].
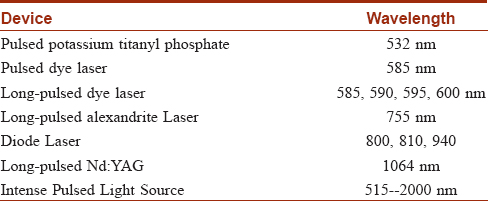
Laser hair reduction
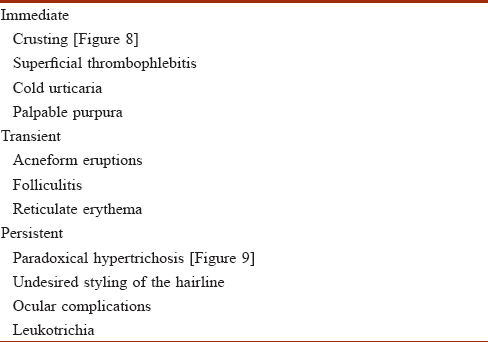
Laser hair reduction is a common procedure performed in the aesthetic clinic. Although the procedure is relatively safe, complications are not infrequent [Table - 2].[5],[6],[7] The devices used in the Indian skin include the long-pulse Nd:YAG, diode and Alexandrite lasers and intense pulse light.[5]
Immediate complications such as a burning sensation, pain, edema and crusting can be reduced with a good precooling and postcooling protocol. Laser burns [Figure - 1] should be recognized early and treated immediately with a moderate potency topical steroid such as mometasone for a few days to reduce the inflammation.
 |
| Figure 1: Crusting following Nd:YAG laser for hair removal |
 |
| Figure 2: Postinflammatory hyperpigmentation after diode laser for hair removal |
 |
| Figure 3: Postinflammatory hypopigmentation following diode laser hair removal session |
 |
| Figure 4: Paradoxical hypertrichosis following hair removal with intense pulse light |
 |
| Figure 5: Postinflammatory hypopigmentation after Nd:YAG laser for Batwing melanosis |
 |
| Figure 6: Hypertrophic scar following Nd:YAG laser for tattoo removal |
 |
| Figure 7: Postinflammatory hyperpigmentation following carbon dioxide laser for acne scars |
 |
| Figure 8: Hypertrophic scar following carbon dioxide laser for posttraumatic scar |
 |
| Figure 9: Laser imprint following intense pulse light |
Acneform eruptions occur in 6% of the patients undergoing laser hair reduction.[9] They arise independently of gender, the number of previous sessions or the presence of polycystic ovarian syndrome. Folliculitis and acneform eruptions may be treated with oral doxycycline for 10–20 days along with topical antibiotics.[9]
Postinflammatory hyperpigmentation is treated with topical hydroquinone, kojic or glycolic acid creams. The application of a broad spectrum sunscreen is mandatory. Post-laser hypopigmentation or depigmentation are anxiety inducing complications which may result after laser hair reduction, pigment lasers or resurfacing lasers. Appropriate delivery of energy using optimal laser settings may reduce the incidence of this complication. Postinflammatory hypopigmentation may treated with topical tacrolimus, as it enhances both tyrosinase activity and melanocyte migration.[10] The application of 65% trichloroacetic acid on depigmented spots may be successful in repigmenting these patches.[11]
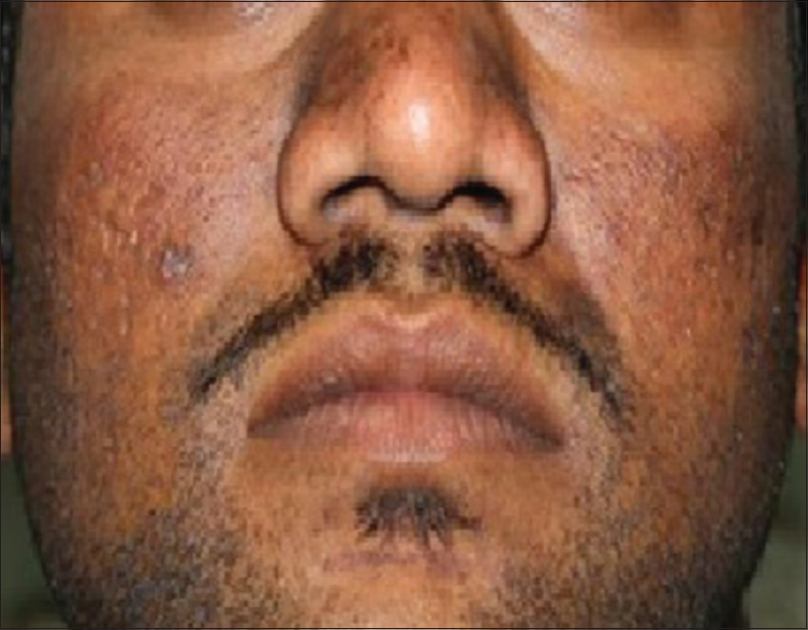
Paradoxical hypertrichosis may occur in 0.6–10% of patients undergoing laser hair reduction and is more common after treatment with intense pulse light. It is more frequent in the head and neck areas (especially on the chin, mandibular and zygomatic areas in patients with darker skin), and in patients with thick dark hair or underlying hormonal imbalance.[12],[13] An uncorrected hormonal abnormality that might be triggering hair growth should be eliminated before labeling a patient as having paradoxical hypertrichosis. It has been suggested that subtherapeutic thermal injury to the surrounding vellus hair stimulates conversion into terminal follicles and inflammatory mediators and upregulatory cytokines may also play a role. Protecting the nonlasered area with cold packs during the procedure may help prevent this complication. Paradoxical hypertrichosis may be treated by using a higher fluence and doubling the number of laser passes on the affected area.
Leukotrichia may develop following laser hair removal and may be temporary or permanent. Differences in the thermal relaxation times of melanocytes and germinative cells may result in destruction or impairment of the function of melanocytes without injury to the hair follicle cells.[15] Epilation or electro-optical synergy hair removal technology may be employed for removal of gray hair.[16]
Undesired styling of hairline is a common complaint when shaping the eyebrows and side locks in women and beard line in men. Drawing the desired hairline margin with a white marking pencil and photographing can prevent future disputes.
Ocular complications have been reported mostly during epilation of the lower part of the eyebrow. When the eyelid closes, the eyeball rolls up owing to the Bell's phenomenon making it vulnerable to laser damage. The insertion of a metallic intraocular eye shield is mandatory during lower eyebrow hair removal.[14]
Cold urticaria, superficial thrombophlebitis and palpable purpura are uncommon, self-limiting side effects that may be encountered on occasion.[6],[7],[8]
Pigment lasers
Lasers are now used to treat various pigmentary conditions such as nevus of Ota, acquired bilateral nevus of Ota-like macules, freckles, lentigines, tattoos, melasma and postinflammatory hyperpigmentation. The 1064 nm Q-switched Nd:YAG, 532 nm KTP (potassium titanyl phosphate) laser, 532 nm frequency doubled Q-switched Nd:YAG, the 755 nm Q-switched alexandrite laser and intense pulse light are commonly used to treat pigmented lesions in the Indian skin.
Q-switched lasers are precision devices and complications are dependent on the beam profile of the laser machine. Devices with a Gaussian beam profile are more prone to adverse effects as compared to those a with a Top hat beam. Pico-second lasers are superior to nanosecond devices in both efficacy and side effect profile. Patient-dependent factors such as the type of lesions, its depth and the skin type of the patient may also influence complications.
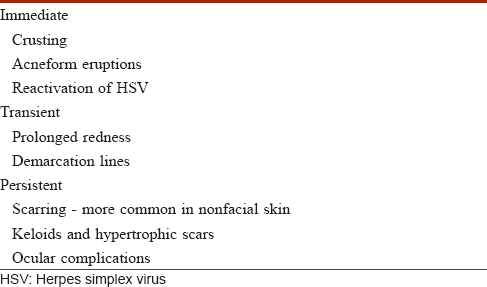
Complications that may occur during treatment with pigment lasers are listed in [Table - 3].[1],[4],[17] Close observation of the tissue response while performing the procedure is necessary to achieve the desired results. Since responses vary widely among patients, a test spot is vital to determine the optimal parameters for the lesion in that patient. It also allows the patient to become familiar with and understand the procedure.

Immediate complications such as pain, erythema, edema and blistering are directly related to the energy used during the procedure. Application of a topical anesthetic cream 45 min prior to starting of the procedure and cold compresses following the session may alleviate pain and discomfort. The application of a topical steroid and antibiotic cream along with a short course of oral prednisolone in patients with immediate blistering helps relieve the symptoms. Blistering or crusting usually resolves over a period of 7–10 days.
Acute compartment syndrome has been reported with treatment of decorative circumferential tattoos.[18] Dividing the circumferential tattoo into different parts may prevent this complication.
Adverse reactions to tattoo ink after laser removal such as eczematous reactions and generalized urticaria are well-known.[17] Anaphylaxis after laser removal of tattoos may be due to the release of ink particles into the systemic circulation. Immediate cutaneous hypersensitivity and delayed anaphylaxis following laser for tattoo removal have been rarely reported. In such cases, pretreatment with antihistamines and topical or oral corticosteroids has been successful in suppressing allergic sequelae; other ablative modalities such as CO2 or Erbium: YAG laser may then be used to remove the tattoo.[1],[19]
Hypertrophic scars and keloids following tattoo removal are rare. In a recent study of tattoo removal with a Q-switched Nd:YAG laser in 1041 patients, keloids were not seen and hypertrophic scars were seen in 3 (0.28%) patients.[20] Hypertrophic scars may be treated with intralesional triamcinalone acetonide injections.
Darkening of ferric oxide and titanium oxide tattoos after treatment with Q-switched Nd:YAG due to oxidation and discoloration of the tattoo pigment may be noted. Oxidized tattoos can only be partially lightened with Nd:YAG laser, and CO2 laser ablation or surgical excision may be necessary for complete removal.[1]
Ablative and fractional resurfacing lasers
Ablative and fractional lasers have evolved significantly over time and the current devices are not only more effective but safer. In India, ablative lasers are mostly used to improve benign lesions. Ablative full-face resurfacing is best avoided on the Indian skin owing to a significant risk of hyperpigmentation and scarring. Fractional resurfacing, on the other hand, has gained popularity in the Indian scenario for the treatment of acne scars and photo aging.[21]
A complete history prior to the procedure should include enquiry into occupational details (to determine the number of hours the patient is exposed to direct or indirect sunlight), tendency to keloids, hypertrophic scars or postinflammatory hyperpigmentation and a history of herpes simplex infections.[22] Old scars should be examined for keloidal tendencies. The patient should be counseled regarding the downtime required after each laser session and it is important to enquire about any significant life events (e.g. marriage) in the near future, to avoid unpleasant surprises. Aggressive parameters, such as increased energy or density, are frequently associated with complications with fractional and ablative lasers. [Table - 4] lists the complications that may be encountered during the use of ablative lasers.[22],[23]
Reactivation of the herpes simplex virus may occur after laser resurfacing leading to widespread facial lesions, delayed epithelialization, and scarring. All at-risk patients undergoing laser resurfacing must be administered antiviral prophylaxis (valacyclovir or famciclovir 500 mg twice daily in patients) starting a day before the procedure and continued 10 days thereafter to prevent herpes simplex virus reactivation.[23],[24],[25],[26]
Prolonged redness may occur after resurfacing of the skin especially with ablative lasers. Temporary fragility of skin and peeling can occur up to a month. Strict photoprotection and moisturizers are helpful in managing these issues. Postinflammatory hyperpigmentation may occur in 26–36% of the patients undergoing laser resurfacing.[27] Demarcation lines (areas of contrast in between the lased and nonlased skin) may be avoided by peripheral feathering of the laser beam into the borders of the treated areas.
Vascular lasers
The flash lamp pumped pulsed dye laser was the first selective laser to be developed on the basis of the theory of selective photothermolysis, for the treatment of port wine stains.[2] The chromophores in vascular lesions are oxyhemoglobin (absorption peaks at 418, 542 and 577 nm) and deoxyhemoglobin (absorption peaks at 430 and 555 nm).[28]
Lasers used for treatment of vascular lesions are listed in [Table - 5] and complications caused by these devices in [Table - 6].
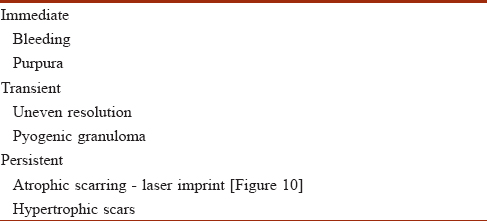
The available vascular lasers are better suited for fairer skin and treatment parameters need to be tweaked for the Indian skin. The pulsed dye laser is safer for superficial vascular lesions as compared to the longer pulse width lasers. The desired endpoint for all vascular lasers is the appearance of purpura.
Multiple sessions over a prolonged period of time are necessary owing to the variable depth of the lesions, locational anatomy and angiogenesis between sessions, and the patient needs to be carefully counseled in this regard.[29] Uneven resolution of the vascular lesions may be seen -- port wine stains may resolve faster on the lateral aspect of the face, and nonfacial lesions respond slowly with treatment with pulsed dye laser, due to the presence of deeper subcutaneous vessels in the central face and in nonfacial lesions.[30]
Pyogenic granulomas may develop in port wine stains after treatment with pulsed dye lasers. These may be treated with the pulsed dye laser itself or excised with a radiofrequency cautery.[31] “Laser imprints” are atrophic scars sometimes seen at laser impact sites due to excessive delivery of energy, absence of cooling or spot overlap.[27]
Excimer Laser and Lamp
The 308 nm Excimer laser and lamp have been used in various dermatological disorders including vitiligo and psoriasis. Adverse effects are dose-dependent and self-limiting. A burning sensation, erythema, peeling of skin, and perilesional hyperpigmentation have been described. The use of a rubber cut-out template during laser delivery and gradual increase in the dose of radiation may help prevent these complications.[32],[33]
Ocular Complications Due to Lasers
Strict adherence to laser protection guidelines may prevent ocular injury.[1] Laser glasses are mandatory and are rated by optical density at various wavelengths. An optical density of >4 for a particular wavelength is considered safe. Ocular injury depends upon the wavelength of laser used, duration of exposure, beam size and incidence of the laser beam. The major chromophores in the eye are water and melanin.[32],[33] Lasers in the 400–1100 nm range target melanin present in the retina, iris, choroid and the sclera causing color flashes, afterimages (in the color complementary to the color of the exposed beam) or immediate visual loss due to damage to the fovea. Lasers of wavelengths between 1400 and 10600 nm may produce immediate burning pain and damage owing to thermal damage of the cornea and lens.[32],[34]
Risks to Operating Personnel
Plume and tissue splatter are potential safety issues for laser operators. Particulate matter as small as 0.12 μm containing bacteria, human papillomavirus, human immunodeficiency virus, carbon and live cellular particles have been identified in surgical smoke. The appropriate use of smoke evacuators, gloves and masks can prevent inhalation of particulate matter and skin contamination of the operator. Tissue splatter is a potential hazard with Q-switched and Erbium:YAG lasers. Fire and electrical hazards are associated with some high-voltage lasers and care must be taken to avoid exposure to flammable objects such as anesthetic gases, oxygen and alcohol-based products during laser procedures.[33],[35]
Complications Due to Topical Anesthetic
Topical anesthetic agents such as EMLA cream (lidocaine and prilocaine cream) used for alleviation of pain during nonablative laser treatments and limited ablative laser treatments may give rise to complications.
Hypersensitivity to topical anesthetic has been well documented [Figure - 10]. If itching or erythema develops after the application of topical anesthetic cream, the procedure must be postponed and other options such as infiltration anesthesia or nerve blocks may be considered. Residual pigmentation in the seborrhoeic area [Figure - 11] may arise after reaction to topical anesthetic creams. This should be recognized early and treated with topical moderate potency corticosteroid creams, depigmenting creams and broad spectrum sunscreen.
 |
| Figure 10: Erythema and edema due to sensitivity reaction to topical anesthetic cream |
 |
| Figure 11: Seborrheic melanosis-like pigmentation due to reaction to topical anesthetic cream |
Methemoglobinemia may ensue when topical anesthetics are used on large areas especially when used with occlusion. It is also more likely to occur in infants.[36]
General Considerations
Written instructions including do's and don'ts given to the patients after the procedure reinforces the postprocedural care instructions given orally. The patients should be educated as to what is to be expected after the procedure and has to report back immediately if any untoward reactions are suspected. Adequate priming with sunscreen, topical retinoids and topical depigmenting agents such as kojic acid, glycolic acid and arbutin will reduce the incidence of complications, especially postinflammatory pigmentary changes. The laser physician should insist on frequent follow-ups in the immediate postlaser period to detect and manage complications early.
Conclusion
Advances in laser technology have not only allowed the development of new devices and expanded the scope of these to target newer diseases more effectively, but has also resulted in a greater incidence of complications, especially in skin of color. A thorough knowledge of basic laser physics, complete understanding of the device in hand, optimal parameter settings, proper methods of laser beam delivery, strict adherence to the standard protocols and early recognition of expected side effects and an intuition to look beyond the routine are the keys to a safe trouble-free laser practice.
Acknowledgement
We are grateful to Dr. Venkataram Mysore for editing the manuscript and his valuable addition to it.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Tosti A, Beer KR, DePadova MP, editors. Anolik R, Geronemus Rg. Complications of fractional lasers (Non-ablative and ablative) In: Management of Complications of Cosmetic Procedures: Handling Common and More Uncommon Problems. Verlag Berlin Heidelberg Springer; 2012.p 23-36
[Google Scholar]
|
| 2. |
Anderson RR, Parrish JA. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science 1983;220:524-7.
[Google Scholar]
|
| 3. |
Alaluf S, Atkins D, Barrett K, Blount M, Carter N, Heath A, et al. Ethnic variation in melanin content and composition in photoexposed and photoprotected human skin. Pigment Cell Res 2002;15:112-8.
[Google Scholar]
|
| 4. |
Tay YK, editor. Treatment of pigmented lesions in the Asian skin. In: Textbook of Laser and Light Dermatology in Asian Skin. Singapore: World Scientific; 2011. p. 37-57.
[Google Scholar]
|
| 5. |
Lim SP, Regina. Laser hair removal in the Asian skin. In: Tay YK, editor. Textbook of Laser and Light Dermatology in Asian Skin. Singapore: World Scientific; 2011. p. 69-81.
[Google Scholar]
|
| 6. |
Lanigan SW. Incidence of side effects after laser hair removal. J Am Acad Dermatol 2003;49:882-6.
[Google Scholar]
|
| 7. |
Lim SP, Lanigan SW. A review of the adverse effects of laser hair removal. Lasers Med Sci 2006;21:121-5.
[Google Scholar]
|
| 8. |
Nasiri S, Saeedi M. Palpable purpura: An uncommon side effects of alexandrite laser hair removal. Iran J Dermatol 2010;13:62-3.
[Google Scholar]
|
| 9. |
Carter JJ, Lanigan SW. Incidence of acneform reactions after laser hair removal. Lasers Med Sci 2006;21:82-5.
[Google Scholar]
|
| 10. |
Kang HY, Choi YM. FK506 increases pigmentation and migration of human melanocytes. Br J Dermatol 2006;155:1037-40.
[Google Scholar]
|
| 11. |
Chandrashekar BS, Sriram R, Madura C. Novel method of treatment of post-Q-switched Nd-YAG laser depigmentation with trichloroacetic acid: A report of two cases. J Cutan Aesthet Surg 2014;7:56-7.
[Google Scholar]
|
| 12. |
Kontoes P, Vlachos S, Konstantinos M, Myrto S. Hair induction after laser assisted hair removal and its treatment. J Am Acad Dermatol 2004;54:64-7.
[Google Scholar]
|
| 13. |
Desai S, Mahmoud BH, Bhatia AC, Hamzavi IH. Paradoxical hypertrichosis after laser therapy: A review. Dermatol Surg 2010;36:291-8.
[Google Scholar]
|
| 14. |
Tosti A, Beer KR, DePadova MP, editors. Remington. Complications of removal lasers. In: Management of Complications of Cosmetic Procedures: Handling Common and More Uncommon Problems. Verlag Berlin Heidelberg Springer; 2012. p. 47-56.
[Google Scholar]
|
| 15. |
Radmanesh M, Mostaghimi M, Yousefi I, Mousavi ZB, Rasai S, Esmaili HR, et al. Leukotrichia developed following application of intense pulsed light for hair removal. Dermatol Surg 2002;28:572-4.
[Google Scholar]
|
| 16. |
Karsai S, Schmitt L, Raulin C, Hammes S. Combination of short- and long-pulsed mode of electro-optical synergy technology for photoepilation: A retrospective study with short- and long-term follow-up. J Eur Acad Dermatol Venereol 2009;23:46-51.
[Google Scholar]
|
| 17. |
Ashinoff R, Levine VJ, Soter NA. Allergic reactions to tattoo pigment after laser treatment. Dermatol Surg 1995;21:291-4.
[Google Scholar]
|
| 18. |
Rheingold LM, Fater MC, Courtiss EH. Compartment syndrome of the upper extremity following cutaneous laser surgery. Plast Reconstr Surg 1997;99:1418-20.
[Google Scholar]
|
| 19. |
Hibler BP, Rossi AM. A case of delayed anaphylaxis after laser tattoo removal. JAAD Case Rep 2015;1:80-1.
[Google Scholar]
|
| 20. |
Kirby W, Alston DB, Chen AH. The incidence of hypertrophic scarring and keloid formation following laser tattoo removal with a quality-switched Nd:YAG laser. J Clin Aesthet Dermatol 2016;9:43-7.
[Google Scholar]
|
| 21. |
Brightman LA, Brauer JA, Anolik R, Weiss E, Karen J, Chapas A, et al. Ablative and fractional ablative lasers. Dermatol Clin 2009;27:479-89, vi-vii.
[Google Scholar]
|
| 22. |
Petrov A, Pljakovska V. Fractional carbon dioxide laser in treatment of acne scars. Open Access Maced J Med Sci 2016;4:38-42.
[Google Scholar]
|
| 23. |
Gilbert S. Improving the outcome of facial resurfacing – Prevention of herpes simplex virus type 1 reactivation. J Antimicrob Chemother 2001;47 Suppl T1:29-34.
[Google Scholar]
|
| 24. |
Beeson WH, Rachel JD. Valacyclovir prophylaxis for herpes simplex virus infection or infection recurrence following laser skin resurfacing. Dermatol Surg 2002;28:331-6.
[Google Scholar]
|
| 25. |
Alster TS, Nanni CA. Famciclovir prophylaxis of herpes simplex virus reactivation after laser skin resurfacing. Dermatol Surg 1999;25:242-6.
[Google Scholar]
|
| 26. |
Riggs K, Keller M, Humphreys TR. Ablative laser resurfacing: High-energy pulsed carbon dioxide and erbium:yttrium-aluminum-garnet. Clin Dermatol 2007;25:462-73.
[Google Scholar]
|
| 27. |
Ross EV, Krakowski AC. Laser treatment for vascular laser. In: Goldmann MP, Fitzpatrick R, Ross V, Kilmer SL, editors. Lasers and for the Energy Devices Skin. 2nd ed. Boca Raton CRP Press; 2013.
[Google Scholar]
|
| 28. |
Chandrashekar BS, Madura C, Pavan RR, Shenoy C. Complications in vascular lasers. In: Pai GS, editor. Complications of Cosmetology: Crafting Cures. 1st ed. New Delhi Jaypee Publications; 2016.
[Google Scholar]
|
| 29. |
Yu W, Ma G, Qiu Y, Chen H, Jin Y, Yang X, et al. Why do port-wine stains (PWS) on the lateral face respond better to pulsed dye laser (PDL) than those located on the central face? J Am Acad Dermatol 2016;74:527-35.
[Google Scholar]
|
| 30. |
Meeker J, Bruce M, Powers R. Pyogenic granuloma appearing in a port wine stain after pulsed dye laser treatment. J Am Acad Dermatol 2016;74:290.
[Google Scholar]
|
| 31. |
Chandrashekar BS, Shobha N, Jagadish P, Vasanth V, Rajashekar ML, Sandeep MA. 308 nm excimer lamp in combination with topical tacrolimus: A retrospective study of its efficacy and safety in childhood vitiligo. Indian J Paediatr Dermatol 2014;15:74-8.
[Google Scholar]
|
| 32. |
Lolis M, Dunbar SW, Goldberg DJ, Hansen TJ, MacFarlane DF. Patient safety in procedural dermatology: Part II. Safety related to cosmetic procedures. J Am Acad Dermatol 2015;73:15-24.
[Google Scholar]
|
| 33. |
Yates B, Que SK, D'Souza L, Suchecki J, Finch JJ. Laser treatment of periocular skin conditions. Clin Dermatol 2015;33:197-206.
[Google Scholar]
|
| 34. |
Smalley PJ. Laser safety: Beyond signs and goggles. Dermatologist 2008;12:7.
[Google Scholar]
|
| 35. |
Kouba DJ, LoPiccolo MC, Alam M, Bordeaux JS, Cohen B, Hanke CW, et al. Guidelines for the use of local anesthesia in office-based dermatologic surgery. J Am Acad Dermatol 2016;74:1201-19.
[Google Scholar]
|
| 36. |
Minkis K, Whittington A, Alam M. Dermatologic surgery emergencies: Complications caused by systemic reactions, high-energy systems, and trauma. J Am Acad Dermatol 2016;75:265-84.
[Google Scholar]
|
Fulltext Views
12,592
PDF downloads
2,867





