Translate this page into:
Congenital lichenoid porokeratosis
2 Department of Pathology, Guru Teg Bahadur Hospital, University College of Medical Sciences, University of Delhi, Shahdara, Delhi, India
Correspondence Address:
Prashant Verma
9 State Bank Colony, G.T. Karnal Road, Delhi
India
| How to cite this article: Verma P, Sharma R, Sharma S. Congenital lichenoid porokeratosis. Indian J Dermatol Venereol Leprol 2012;78:750-752 |
Sir,
Porokeratosis, a keratinization disorder, represents a repertoire of morphological reaction patterns comprising porokeratosis of Mibelli, disseminated superficial porokeratosis (DSP), linear porokeratosis, punctate porokeratosis, and porokeratosis palmaris, plantaris et disseminata. Nevertheless, "cornoid lamella", a uniform denominator, is the diagnostic hallmark. The cornoid lamella consists of a thin column of tightly packed parakeratotic cells within a keratin-filled epidermal invagination. Within the parakeratotic column, the horny cells appear homogeneous and possess deeply basophilic pyknotic nuclei. In the epidermis beneath the parakeratotic column, the keratinocytes are irregularly arranged and have pyknotic nuclei with perinuclear edema. No granular layer is seen within the parakeratotic column, while the keratin-filled invagination of the epidermis has a well-developed granular layer. [1]
A moderately dense, lymphocytic infiltrate and dilated capillaries may be present in the papillary dermis. The center of the lesion often displays atrophy, with areas of liquefaction degeneration in the basal layer, colloid-body formation, and flattening of rete ridges. [1],[2] The dermis may be edematous or fibrotic with telangiectasia. The present case is being reported for the purpose of illustration of a rare clinical presentation and the extraordinary histopathological feature of uniform pigment incontinence in the papillary dermis.
A 16-year-old boy accessed our dermatology clinic with an asymptomatic dark coloured eruption over his left shoulder and arm present since birth. The lesions were non-progressive. There were no other mucocutaneous complaints. Review of systems was normal. There was no significant family history. Examination revealed multiple discrete to coalescent keratotic papules and plaques with atrophy in the centre and raised ridge-like borders. These lesions were distributed in a blaschkoid fashion along the left side of chest, shoulder, ventral and medial aspect of arm, and forearm [Figure - 1]. Section from a representative lesion showed thin column of tightly packed parakeratotic cells within a keratin-filled epidermal invagination, the cornoid lamella. The parakeratotic column extended at an angle away from the center of the lesion. In the epidermis beneath the parakeratotic column, the keratinocytes were irregularly arranged and depicted pyknotic nuclei with perinuclear edema. Within the parakeratotic column, granular layer was absent [Figure - 2]. In addition, pigmentary incontinence in the upper dermis was remarkable [Figure - 3]. Accordingly, a diagnosis of congenital blaschkoid porokeratosis was rendered.
 |
| Figure 1: Porokeratosis: Hyperpigmented annular lesions distributed in a blaschkoid fashion along the left side of chest, shoulder, ventral and medial aspect of arm, and forearm |
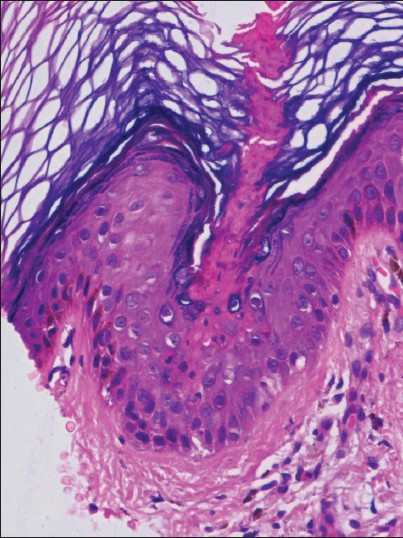 |
| Figure 2: Epidermal invagination with parakeratotic column, the cornoid lamella (H and E, ×400) |
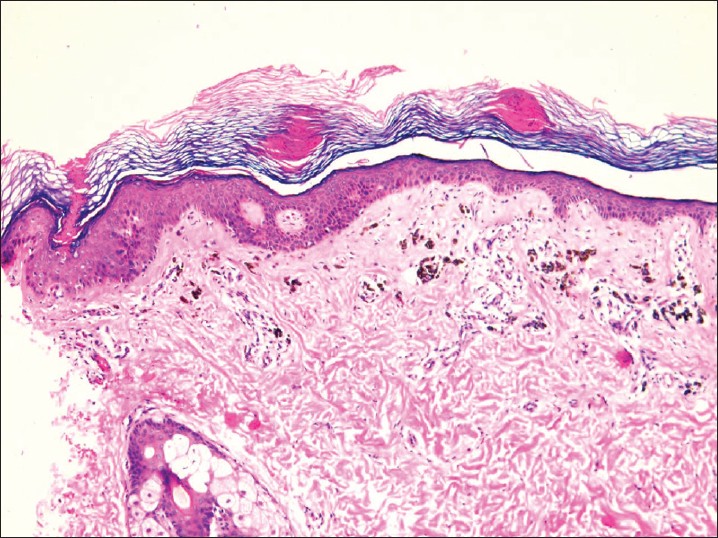 |
| Figure 3: Hyperkeratosis, epidermal atrophy, parakeratotic columns and pigmentary incontinence in the upper dermis (H and E, ×100) |
Linear porokeratosis, an uncommon variant, may either be congenital or may develop during adulthood. [3],[4] Lesions of linear porokeratosis are grouped and linearly arranged along the lines of Blaschko. Zosteriform pattern may manifest on the trunk as seen in the present case. Linear porokeratosis may be an expression of genetic cutaneous mosaicism. Malignant degeneration and metastasis may complicate linear porokeratosis, [5] which can be either basal cell carcinoma or squamous cell carcinoma and most likely occur in older adults. [6] The risk of malignancy has been shown to correlate with the size and duration of the lesions. [6] Lesional ulcerations, [7] underlying bony abnormalities [8] and nail dystrophy [9] may complicate the course of linear porokeratosis. Other medical conditions reported in association with porokeratosis include immunosuppression, being a recipient of organ transplantation, burn scar, Crohn disease, and liver disease. [1]
Lichenoid tissue reaction, papillary dermal lymphocytic infiltrate (97%), spinous layer vacuolar changes (90%), dyskeratotic cells in the epidermis (77%), and liquefaction degeneration of the basal layer (67%) under the cornoid lamella have been described in a decreasing order of frequency. [2] However, in the present case only pigmentary incontinence in the papillay dermis was prominent. This may be due to the very fact that the lesion was chronic. Hence, lichenoid porokeratosis may masquerade as lichen planus on first look under the microscope. It is, therefore, imperative to take cognizance of this histopathological variant of porokeratosis and to include the border of the lesion in biopsy. The differential diagnosis of linear porokeratosis include verrucous epidermal nevus, linear lichen planus, linear psoriasis, nevus sebaceous, verrucous stage of incontinentia pigmenti, and linear Darier′s disease to name a few. Topical calcipotriol, tretinoin, cryotherapy, 585-nm flashlamp-pumped pulsed-dye laser and systemic retinoids have been used to treat linear porokeratosis. [10]
| 1. |
Sertznig P, von Felbert V, Megahed M. Porokeratosis: Present concepts. J Eur Acad Dermatol Venereol 2012;26:404-12.
[Google Scholar]
|
| 2. |
Shumack S, Commens C, Kossard S. Disseminated superficial actinic porokeratosis. A histological review of 61 cases with particular reference to lymphocytic inflammation. Am J Dermatopathol 1991;13:26-31.
[Google Scholar]
|
| 3. |
Garg T, Ramchander, Varghese B, Barara M, Nangia A. Generalized linear porokeratosis: A rare entity with excellent response to acitretin. Dermatol Online J 2011;17:3.
[Google Scholar]
|
| 4. |
Malhotra SK, Puri KJ, Goyal T, Chahal KS. Linear porokeratosis. Dermatol Online J 2007;13:5.
[Google Scholar]
|
| 5. |
Lorenz GE, Ritter SE. Linear porokeratosis: A case report and review of the literature. Cutis 2008;81:479-83.
[Google Scholar]
|
| 6. |
Happle R. Cancer Proneness of linear porokeratosis may be explained by allelic loss. Dermatology 1997;195:20-5.
[Google Scholar]
|
| 7. |
Watanabe T, Murakami T, Okochi H, Kikuchi K, Furue M. Ulcerative porokeratosis. Dermatology 1998;196:256-9.
[Google Scholar]
|
| 8. |
Tseng SS, Levit EK, Ilarda I, Garzon MC, Grossman ME. Linear porokeratosis with underlying bony abnormalities. Cutis 2002;69:309-12.
[Google Scholar]
|
| 9. |
Chen HH, Liao YH. Onychodystrophy in congenital linear porokeratosis. Br J Dermatol 2002;147:1272-3.
[Google Scholar]
|
| 10. |
Erkek E, Bozdogan O, Sanli C, Ozoguz P. Clinicopathologic challenge: Linear brown macules on the chest and arm. Linear porokeratosis. Int J Dermatol 2008;47:539-41.
[Google Scholar]
|
Fulltext Views
3,475
PDF downloads
3,226





