Translate this page into:
Cross-sectional study of acral melanoma awareness in a group of South African final phase medical students
Corresponding author: Dr. Johanna M. Eksteen, Department of Dermatology, Stellenbosch University, Tygerberg Academic Hospital, Cape Town, South Africa. jmeksteen96@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Eksteen JM, Visser WI, de Wet J, Lombard C, Zunza M, Tod B. Cross-sectional study of acral melanoma awareness in a group of South African final phase medical students. Indian J Dermatol Venereol Leprol 2022;88:444.
Abstract
Background:
Acral melanoma refers to melanoma arising on the palms, soles and nail unit, which are sun-protected areas and ultraviolet exposure is not a risk factor. Acral melanoma is associated with a poorer prognosis than other melanoma subtypes most likely due to the high rates of delayed diagnosis. Acral melanoma affects all skin types equally. There is a misconception that people with more pigmented skin types (Fitzpatrick 4–6) do not develop melanoma, due to the protective effect of melanin.
Objectives:
The aim of the study was to determine acral melanoma knowledge and awareness of a group of South African, final phase medical students.
Methods:
This was a quantitative and cross-sectional study. A questionnaire consisting of 20 clinical images of skin lesions requiring a diagnosis and management plan was distributed. Responses to six images of melanomas were analysed. Further questions to measure acral melanoma knowledge and related issues were included in the study. A biostatistician appropriately managed statistical analysis.
Results:
Hundred and one final phase medical students’ answers were gathered and analysed. Only 7.9% of the participants diagnosed all six melanomas correctly; 61.4% correctly diagnosed ≥50% of the melanomas. While 77.2% of the participants identified all non-acral cutaneous melanoma correctly, only 8.9% identified all acral melanomas. However, of all participants making the correct diagnosis, >90% selected the appropriate management plan (urgent referral).
Limitations:
This study examined a small sample of trainee healthcare workers. The results cannot be assumed to apply to all South African healthcare workers. Responses given in a questionnaire may not reflect actual behaviour. The dermatology division in question has made acral melanoma a research priority, thus acral melanoma knowledge in this group may in fact be better than in other institutions.
Conclusion:
The present study demonstrates that groups of imminent doctors have low rates of recognition of melanoma, particularly acral melanoma. This is consistent with high levels of primary misdiagnosis of acral melanoma reported in the literature. Fortunately, these participants managed the melanomas they diagnosed appropriately in >90% of cases. This confirms that the deficit in the participant group is awareness and knowledge. Those aware of the disease immediately acknowledged the need for urgent referral.
Keywords
Acral melanoma
awareness
diagnosis
knowledge
melanoma
Plain Language Summary
A group of South African medical students, having completed their dermatology training, answered a questionnaire about skin cancers, consisting of photos with matching diagnoses and management pathways. The aim of the study was to determine the group’s knowledge and awareness of a specific type of skin cancer: acral melanoma. Acral melanoma is the skin cancer most commonly found in people with more pigmented skin types. The areas of occurrence include palms, soles and nails. Ultraviolet light is not a known risk factor causing acral melanoma. Of the 101 participating students, only 8.9% diagnosed all acral melanomas correctly, compared to the 77.2% who correctly diagnosed non-acral melanomas. However, it was reassuring that among those who correctly identified acral melanoma, more than 90% chose the appropriate management plan. We can deduce from this that awareness and recognition of this disease falls short of expectation. This study is important, especially in the South African population, where the majority have more pigmented skin. A 2019 study proved that 62% of patients presenting with acral melanoma for specialist care in public health had a poor, if not terminal, illness.
Introduction
Acral melanoma refers to melanoma arising on the palms, soles and nail unit, which are sun-protected areas.1 Ultraviolet exposure is not a risk factor for acral melanoma development.1 Patients with acral melanoma have worse survival outcomes, poorer prognosis and compared to patients with non-acral cutaneous melanoma.2 The reason for the poorer prognosis in acral melanoma patients is yet to be confirmed, but appears to be largely due to delayed presentation and referral.3,4 This is an international phenomenon.3,4
Acral melanoma affects people irrespective of the degree of pigmentation of their skin, in contrast to cutaneous melanoma of sun-exposed skin (non-acral cutaneous melanoma), which occurs far more commonly in lightly pigmented people (Fitzpatrick phototype 1–3).1,3,5 A common misconception is that people with more darkly pigmented skin types (Fitzpatrick 4–6) do not develop melanoma, due to the protective effect of the increased amount of melanin in their skin.1,14 Melanomas arising in people with Fitzpatrick 4–6 skin types are far more likely to arise in sun-protected areas and are commonly acral melanoma. Since, extrapolating from the 2011 South African Census, the majority of South Africa’s population falls into the Fitzpatrick 4–6 skin type group, acral melanoma is a relevant concern in South Africa.6
In South Africa, there is little research focusing on acral melanoma. A report published in 2019 examined melanoma incidence and clinical features by analysing the South African National Cancer Registry’s data from 2005 to 2013.7 They show that while non-acral cutaneous melanoma is largely a disease of lightly pigmented South Africans, acral melanoma is of particular concern to darkly pigmented South Africans.7 Of 11,784 cases of melanoma reported over the period, 1991 occurred in the ‘Black African’ population group. More concerning is that when a subgroup of these patients who were presumed to have mostly acral melanomas was analysed, 62% of patients presented with advanced disease.7 No South African study to date has focused on determining the reason for acral melanoma patients presenting with advanced disease.
Studies from outside of South Africa have identified a gap in melanoma knowledge of some groups of health-care providers, particularly regarding acral melanoma and melanomas arising in Fitzpatrick 4–6 skin types.8 This represents one possible reason for late presentation.
Objectives
The aim of the study was to assess South African final phase medical students’ knowledge and awareness of the presentation, screening, and management of acral melanoma at a primary health-care level, as one possible reason for late presentation of acral melanoma patients.
A component of this study examines the participants’ knowledge about melanoma in more pigmented skin types (Fitzpatrick phototype 4–6). The motivation for this approach was that the majority of skin cancer research and teaching focuses on skin cancer in lightly pigmented skin types (Fitzpatrick phototype 1–3). This has resulted in inadequate knowledge among many healthcare workers and leads to late diagnosis and poor outcomes in many cases. There are important biological differences in skin cancer between individuals based on the degree of pigmentation of their skin (melanin, the main pigment in skin offers some protection from skin cancer).
Methods
Design
Primary data analysis of a quantitative cross-sectional study was performed. A self-administered questionnaire, partly consisting of 20 clinical images of skin lesions requiring a diagnosis and management plan, was distributed to consenting final phase medical students. Responses to six images, representing melanomas, (4 acral melanoma and 2 non-acral cutaneous melanomas) among the 20 images were analysed. Two nail apparatus acral melanomas were included to determine if this presentation was particularly problematic. The dermatologists (WV, JdW and BT) involved in the study validated the images and their management plans. The dermatologists selected classical examples of melanoma and the other skin conditions presented.
Further questions to measure acral melanoma knowledge, awareness of skin cancer and melanoma in people with darkly pigmented skin types and total body skin examinations were included in the study. Darkly pigmented skin types were defined as Fitzpatrick phototypes 4–6.10 Lightly pigmented skin was defined as Fitzpatrick phototypes 1–3.10 An explanatory table of the Fitzpatrick phototypes was included in the questionnaire. The questionnaire was partly adapted from those used in the two previous studies.8,9
Setting
The study took place at the Faculty of Medicine and Health Sciences of Stellenbosch University, Tygerberg Campus.
Participants
Inclusion criteria were: Final phase medical students (in their final 18 months of training), who had already completed their dermatology clinical rotation and who gave written informed consent. Participants were neither informed that the study topic was melanoma, nor that their responses to questions not relating to melanoma would not be analysed. Exclusion criteria were junior students, students who had not yet completed their dermatology rotation and those who withheld consent.
Variables
The participants’ accuracy in diagnosing melanoma was stratified by those correctly diagnosing melanoma in 100%, ≥50% or <50% of cases. Their accuracy in diagnosing non-acral cutaneous melanoma, acral melanoma and nail melanoma was also analysed in this way. Overall correct melanoma diagnoses were calculated. Correct management plan was calculated as a percentage in both the group making a correct diagnosis and those making an incorrect diagnosis. Theoretical awareness about melanoma was also calculated as a percentage.
Bias
To eliminate the major source of bias, the questionnaire was distributed in two parts. The clinical images section (Section 1) of the questionnaire was completed and collected before the distribution, completion, and collection of Section 2. Section 2 contained skin cancer and melanoma awareness and knowledge questions.
Study size
Sample size calculation estimated that 100 participants were required. A total of 101 participants were assessed.
Statistical analysis
We summarised categorical variable as count (percent). We assessed whether the participant had given a melanoma diagnosis for each of the 20 images and then computed the true positive, true negative, false positive and false negative values for each participant. We aggregated the computed values using the STATA Midas module for diagnostic test accuracy and reported the sensitivity and the corresponding 95% CI. We computed the kappa statistic to assess how consistent was the student binary ratings (i.e., melanoma diagnosis vs. other) across the 20 images. The correct management option was correlated with the correct diagnosis to prevent analytic errors.
Ethical considerations
Permission for data collection was granted by the division for institutional research and planning at Stellenbosch University, the Bachelor of Medicine and Bachelor of Surgery programme committee and the Health Research Ethics Committee of Stellenbosch University. Project number U19/01/009. Images used were from online sources (in accordance with their copyright stipulations accompanied by references) and from one author’s (JdW) personal collection (with patient consent).11
Participants did understand the aim was to assess their knowledge of dermatology. Responses were anonymised. The results of the study were communicated to the group after the study. Participants had the option to withdraw their participation at any stage.
Results
The study collected 101 responses from September 2019 to December 2019. This represents approximately 30% of the target group at Stellenbosch University. A potential confounder is that students with a special interest in dermatology may have elected to participate. Study participants’ characteristics are presented in Table 1. Missing data were infrequent.
| Variable | Categories | Frequency | Percentage |
|---|---|---|---|
| Age | 20–29 years | 99 | 98.0 |
| 30–39 years | 1 | 1.0 | |
| 40–49 years | 1 | 1.0 | |
| Gender | Male | 40 | 39.6 |
| Female | 61 | 60.4 | |
| Present year | Final year (6thyear) | 43 | 42.6 |
| of study | Penultimate year (5th year) | 58 | 57.4 |
| Additional clinical experience | None (only 2 weeks dermatology theory and 2 weeks practical experience) | 99 | 98.0 |
| 4 weeks elective in dermatology department | 2 | 2.0 | |
| Ever performed a full body skin examination | Yes | 42 | 41.6 |
| on a patient | No | 59 | 58.4 |
| Recall receiving education on skin cancer in | Yes | 87 | 86.1 |
| people with Fitzpatrick phototype 4–6 | No | 14 | 13.9 |
Figure 1 shows the students’ accuracy in diagnosing melanoma in this study, stratified by those correctly diagnosing melanoma in 100%, ≥50% or <50% of cases. Only 7.9% of the participants diagnosed all the melanomas correctly (95% confidence interval 4.07–14.86). While 77.2% of the participants identified all non-acral cutaneous melanoma correctly (95% confidence interval 67.92–84.45), only 8.9% identified all acral melanomas (95% confidence interval 4.66–16.36) correctly. Overall, 61.4% of participants correctly diagnosed ≥50% of melanomas. Of the six images presenting classical examples of melanoma, 57% (95% confidence interval: 52–62%) of the participants were able to make the correct diagnosis. Overall, the unadjusted agreement of student’s ratings was 61.0% (95% confidence interval 47–65%) and was only slight better than what could be expected by chance (50%). After adjusting for agreement by chance, the agreement of student’s ratings was 21.0% (95% confidence interval 1.5–40%). The participants selected the appropriate management plan (urgent referral) in a majority of cases where they had correctly diagnosed melanoma [Figure 2]. Of those participants making the incorrect diagnosis, 73.9% would have managed these melanomas inappropriately (less than urgent referral).
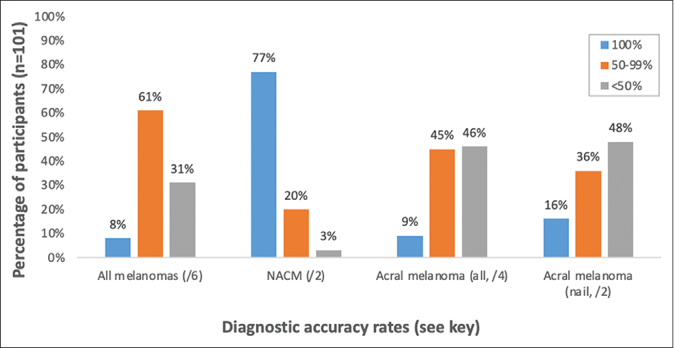
- Diagnostic accuracy rates for melanomas (correctly diagnosed either 100%, ≥50% or <50% of melanomas). NACM: Non-acral cutaneous melanoma
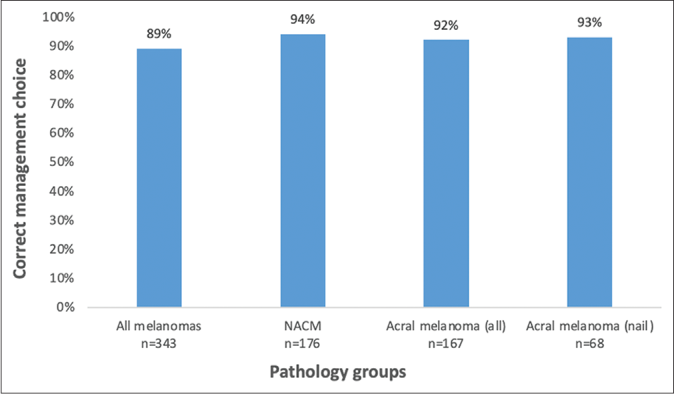
- Percentage of participants selecting the appropriate management plan (among those who made the correct diagnosis). NACM: Non-acral cutaneous melanoma
The most common misdiagnoses for the four acral melanomas combined were trauma (25.8%), tar stains (17.8%), dermatophyte infection (9.4%) and basal cell carcinoma (7.4%). The most common misdiagnoses for the non-acral cutaneous melanoma were moles or naevi (6.9%) and nonmelanoma skin cancer (5.0%). In Section 2 of the questionnaire, 73% of students correctly identified the palms, soles, and nail beds as the commonest location of melanoma in Fitzpatrick phototype 4–6 individuals. In contrast, only 53.5% identified the trunk and limbs as the most likely location for melanoma in the Fitzpatrick phototype 1–3 group. Figure 3 presents further findings regarding the students’ knowledge about skin cancer in individuals with Fitzpatrick phototype 4–6.
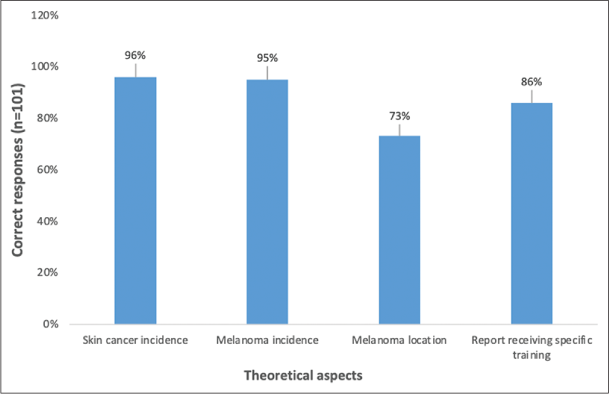
- Correct or positive responses relating to different theoretical aspects of skin cancer in Fitzpatrick phototype 4–6 individuals
Discussion
Cutaneous melanoma carries the worst prognosis of all types of skin cancer.12 Acral melanoma is a unique subtype within the melanoma spectrum, with differing pathogenesis and epidemiology compared to more common melanoma subtypes.3 The present study demonstrates that a group of imminent doctors has low rates of recognition of melanoma, particularly acral melanoma.
The largest study till now found that poor prognosis relates to late diagnosis (although this study examined only acral lentiginous melanoma, the commonest histological subtype of acral melanoma).4 The acceptable level for acral melanoma diagnosis is not defined; however, a meta-analysis of melanoma diagnostic accuracy studies found that among general physicians undertaking naked eye examination of all types of melanoma, the sensitivity was 78.0% (95% confidence interval, 60–90%).13 This student group seems to fall far short of this average (56.6%); however, the high proportion of traditionally difficult melanoma diagnoses (acral melanomas) in this study puts them at a disadvantage. The fact that the participants’ diagnostic accuracy was only marginally better than chance is a better measure of the problem.
An interesting result was higher diagnostic accuracy of nail unit melanoma in comparison to other acral melanomas [Figure 1 for comparison]. The nail acral melanoma was analysed separately to see if there was a specific conceptual issue regarding the topic. The possibility that the participants recognised the image as it was very similar to their training images, could be entertained.
This cohort of students will enter South African health-care institutions in less than 12 months, with no definite prospect of further dermatological training. Students are not guaranteed to encounter an acral melanoma during their clinical rotation, since it is a rare condition. Student awareness of acral melanoma relies on theoretical knowledge attained during didactic lectures. The topic of acral melanoma is specifically mentioned in the lectures that this group receives, and the participants acknowledge this. Possible reasons for this include poor lecture attendance or failure of synthesis of knowledge allowing application to the clinical context. The fact that a majority of participants have never personally performed a full body skin examination focused on skin cancer screening and detection is also of concern. All students could practise while guided by specialists during their two-week practical rotation.
Studies have shown that melanomas arising in people with Fitzpatrick 4–6 phototype skin have worse outcomes.12,15 Possible reasons for this include delay in patient presentation, diagnostic challenges, misdiagnosis and challenges in the histopathological diagnosis of early lesions, as well as disparities in access to healthcare.12,16-18 Issues such as language barriers may delay presentation in some contexts.19 It is important to note that these studies originate from outside of South Africa. A recent South African study demonstrated deeper Breslow thicknesses (implying worse prognosis) in acral melanoma in people with Fitzpatrick 4–6 phototype skins, conducted at the same institution as the present study, but could only speculate as to the reasons for this.20 The present study aimed to explore one possible reason for this.
In South Africa, the incidence of melanoma is reported as 2.7/100,000 per year (2011–2013).7 In an analysis of the South African population group presumed to have the most pigmented skin (recorded as ‘Black African’), the incidence of melanoma was far lower (0.5/100,000, 2011–2013).7 However, limb lesions (acral melanomas predominantly) were the most common type of melanoma in this group. Where Breslow thickness was available, it was greater than four mm in 62% of cases implying poor, if not terminal, prognosis.7 Thus, this condition is of public health concern, particularly in terms of addressing historical health disparities.
Specific misdiagnoses of acral melanoma in this study were those classically reported in the literature, for example, trauma, tar staining and dermatophyte infection.8,21 This aspect should be specifically addressed in the future teaching strategies.
A further discouraging outcome of this study is that in 73.9% of cases where students misdiagnosed melanoma, they would not have referred the patients urgently. Thus, only a minority of participants demonstrate attainment of level 2 of the learning matrix (conscious incompetence).22 In the case of relatively rare diseases such as acral melanoma, this concept could be exploited through the specific teaching of ‘red flags.’23 Discussion of specific cases may be more effective, working from patient presentations and then progressing to disease features, rather than the rare disease being lost in a bland ‘textbook-style’ presentation of typical disease characteristics.23 In addition, teaching strategies could employ mandatory, supervised assessments concerning full body skin examinations ensuring a 100% exposure rate. Emphasis should be placed on the examination of the palms, soles, and nails in individuals of all skin types. This will ensure improved awareness of acral melanoma.
About 95% of this group of students were aware that people with pigmented skin develop skin cancer and melanoma in particular. More than 70% were aware of the most common sites of melanoma development in people with Fitzpatrick phototypes 4–6. Despite their knowledge, it did not translate into the ability to diagnose melanoma in these locations.
Limitations
This study examined a small sample of trainee healthcare workers. The results cannot be assumed to apply to all South African healthcare workers. Responses given in a questionnaire may not reflect actual behaviour. For example, it is relatively easy to specify ‘urgent referral’ as a management plan, but in reality, this requires a significant amount of time and effort. Responses may be prejudiced by lack of patient history or the option to palpate lesions. The dermatology division in question has made acral melanoma a research priority and therefore may emphasise the topic more than other academic dermatology centres in teaching. Thus, acral melanoma knowledge in this group may in fact be better than in other institutions.
Conclusion
Diagnostic delay is a critical factor in the poor prognosis of acral melanoma. Possible reasons for late diagnosis include lack of awareness and knowledge about acral melanoma among healthcare workers, lack of public awareness of acral melanoma and poor access to and efficiency of health-care systems. This study suggests that a clear teaching strategy is required to inform future doctors about acral melanoma, melanoma in Fitzpatrick 4–6 phototype skins and in general. These actions are a critical factor in addressing acral melanoma as a public health issue in South Africa.
Acknowledgment
Dr. Henriette Burger from the Division of Radiation Oncology at Stellenbosch University and Tygerberg Academic Hospital for proof-reading the manuscript.
Declaration of patient consent
Patients’ consent not required as there are no patients in this study.
Financial support and sponsorship
Division of Dermatology, Tygerberg Academic Hospital. Cape Town.
Conflicts of interest
There are no conflicts of interest.
References
- Malignant melanoma of sun-protected sites: A review of clinical, histological, and molecular features. Lab Investig. 2017;97:630-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prognosis of acral melanoma: A series of 281 patients. Ann Surg Oncol. 2013;20:3618-25.
- [CrossRef] [PubMed] [Google Scholar]
- Melanoma of the hand and foot: Epidemiological, prognostic, and genetic features. A systematic review. Br J Dermatol. 2012;166:727-39.
- [CrossRef] [PubMed] [Google Scholar]
- Acral lentiginous melanoma: A skin cancer with unfavourable prognostic features. A study of the German central malignant melanoma registry (CMMR) in 2050 patients. Br J Dermatol. 2018;178:443-51.
- [CrossRef] [PubMed] [Google Scholar]
- Racial differences in skin cancer awareness and surveillance practices at a public hospital dermatology clinic. J Am Acad Dermatol. 2014;70:312-7.
- [CrossRef] [PubMed] [Google Scholar]
- Census 2011. Vol. P0301.4. South Africa: Statistics South Africa 2012. Available from: https://www.statssa.gov.za/publications/p03014/p030142011.pdf [Last accessed on 2020 May 21]
- [Google Scholar]
- The incidence of melanoma in South Africa: An exploratory analysis of national cancer registry data from 2005 to 2013 with a specific focus on melanoma in black Africans. S Afr Med J. 2019;109:246-53.
- [CrossRef] [PubMed] [Google Scholar]
- A dermatological questionnaire for general practitioners in England with a focus on melanoma; misdiagnosis in black patients compared to white patients. J Eur Acad Dermatol Venereol. 2017;31:625-8.
- [CrossRef] [PubMed] [Google Scholar]
- Nurse practitioners' knowledge and practice regarding malignant melanoma assessment and counselling. J Am Acad Nurse Pract. 2008;20:367-75.
- [CrossRef] [PubMed] [Google Scholar]
- Fitzpatrick Skin Phototype. 2012. Available from: https://www.dermnetnz.org/topics/skin-phototype [Last accessed on 2020 May 14]
- [Google Scholar]
- Insert Picture Diagnoses. 2019. Available from: https://www.dermnetnz.org/assets/uploads/[insertimagediagnoses]__watermarkedwyjxyxrlcm1hcmtlzcjd.jpg [Last accessed on 2019 Sep 24]
- [Google Scholar]
- Malignant melanoma in African-Americans. Medicine (Baltimore). 2017;96:e96:e6258.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of malignant melanoma using artificial intelligence: An observational study of diagnostic accuracy. Dermatol Pract Concept. 2019;93:e2020011.
- [CrossRef] [PubMed] [Google Scholar]
- The protective role of melanin against UV damage in human skin. Photochem Photobiol. 2008;84:539-49.
- [CrossRef] [PubMed] [Google Scholar]
- Racial disparities in melanoma survival. J Am Acad Dermatol. 2016;75:983-91.
- [CrossRef] [PubMed] [Google Scholar]
- Histopathological diagnosis of acral lentiginous melanoma in early stages. Ann Diagn Pathol. 2017;26:64-9.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant melanoma in South Africans of mixed ancestry: A retrospective analysis. Melanoma Res. 2003;13:415-9.
- [CrossRef] [PubMed] [Google Scholar]
- Early detection of acral melanoma: A review of clinical, dermoscopic, histopathologic, and molecular characteristics. J Am Acad Dermatol. 2019;81:805-12.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of socioeconomic status and sociodemographic factors on melanoma presentation among ethnic minorities. J Community Health. 2011;36:461-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and pathological features of acral melanoma in a South African population: A retrospective study. S Afr Med J. 2018;108:777-81.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple primary acral melanomas in two young Caucasian patients. Dermatology. 2014;228:307-10.
- [CrossRef] [PubMed] [Google Scholar]
- University Hospitals Birmingham, NHS Trust. 2020. The Four Stages of Competence. Available from: https://www.uhbeducation.co.uk/content/four-stages-competence [Last accessed on 2019 May 22]
- [Google Scholar]
- Rare disease terminology and definitions-a systematic global review: Report of the ISPOR rare disease special interest group. Value Health. 2015;18:906-14.
- [CrossRef] [PubMed] [Google Scholar]






