Translate this page into:
Cutaneous botryomycosis treated successfully with injectable ceftriaxone sodium in an immunocompetent child
2 Department of Pathology, Prolife Diagnostics, Bhubaneswar, Odisha, India
Correspondence Address:
Chandra Sekhar Sirka
Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar, Odisha
India
| How to cite this article: Pradhan S, Sirka CS, Panda M, Baisakh M. Cutaneous botryomycosis treated successfully with injectable ceftriaxone sodium in an immunocompetent child. Indian J Dermatol Venereol Leprol 2018;84:485-487 |
Sir,
Botryomycosis is a chronic granulomatous suppurative bacterial infection.[1],[2] It is a rare and uncommon disease, mostly reported in immunocompromised adults. Approximately 200 patients have been reported in English literature.[3] Its occurrence in children is rare. We describe a case of cutaneous botryomycosis in an immunocompetent girl child treated successfully with injectable ceftriaxone sodium.
A 14-year-old girl presented to the dermatology outpatient department of All India Institute of Medical Sciences, Bhubaneswar with swellings on the right foot studded with papules and nodules on it for 3 years. She gave a history of trauma on the right foot. She had undergone incision and drainage of the swellings twice in the past with no significant improvement. Rather, she continued to develop papules and nodules on the swellings. Cutaneous examination revealed skin-colored lobulated swellings on the dorsum of the right foot with multiple skin-colored papules and nodules of varying stages with surface change like erosion, crusting and ulceration on papules and nodules and some giving serous and seropurulent discharge [Figure - 1]a. Similar lesions were also present on the sole of the foot [Figure - 1]b. Based on these clinical findings, botryomycosis, eumycetoma, actinomycetoma and actinomycosis were kept in differentials and the patient was investigated.
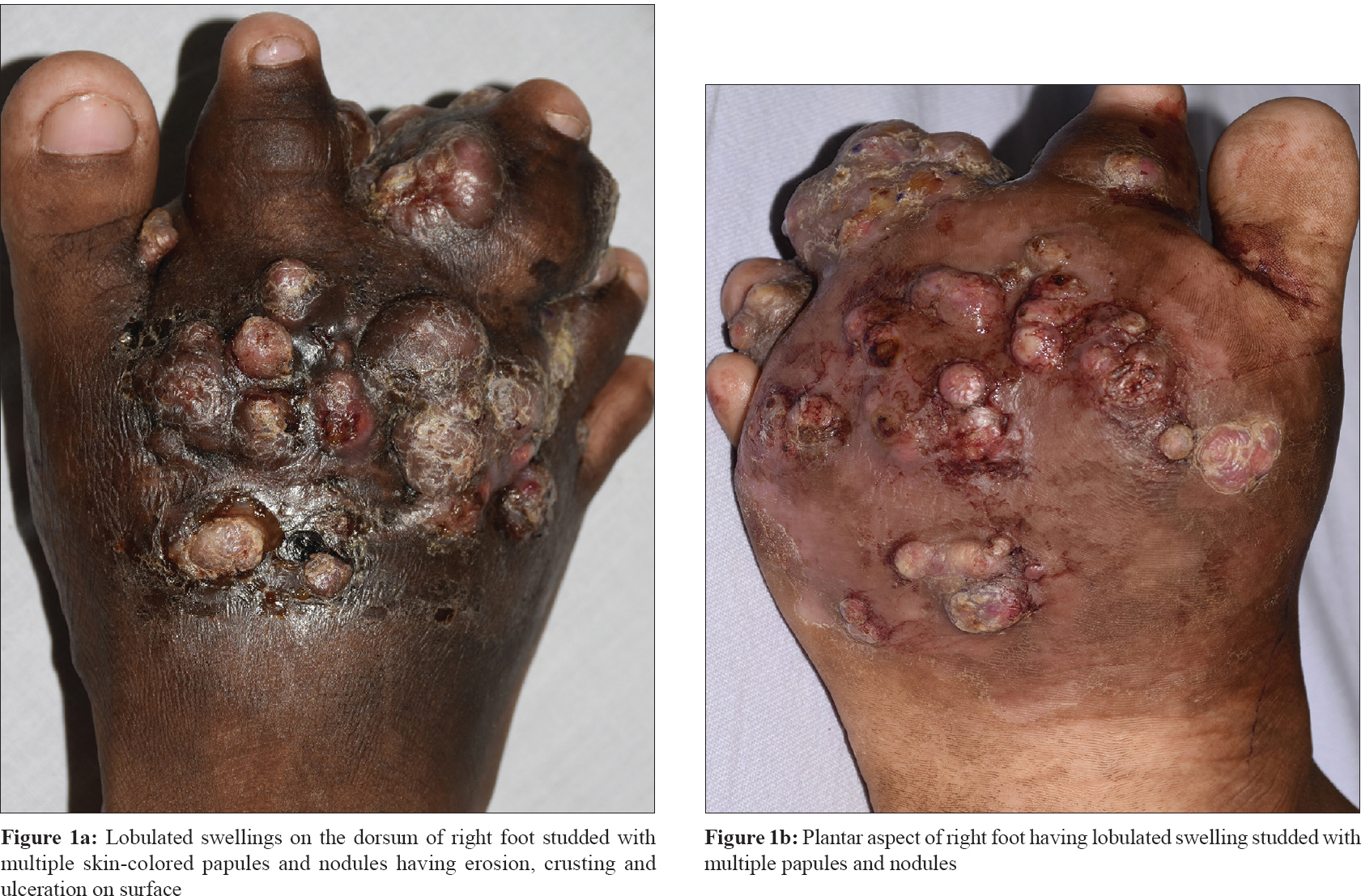 |
| Figure 1 |
Her routine investigations were within normal limit. Test for human immunodeficiency virus by enzyme-linked immunosorbent assay was negative. X-ray of the right foot did not show any bony abnormalities. Tissue culture and pus culture showed methicillin-sensitive Staphylococcus aureus sensitive to amikacin and ceftriaxone. KOH and fungal culture of the seropurulent discharge did not reveal any organism. Biopsy of the nodule showed bacterial granules in dermis with an eosinophilic rim at the periphery suggestive of Splendore–Hoeppli phenomenon [Figure - 2]. Based on clinical, microbiological and histopathological findings, the diagnosis of botryomycosis was made. Patient was initiated on injection ceftriaxone sodium 1,000 mg intravenous daily. After 2 and 1/2 months of treatment, the swelling subsided and nodules and papules disappeared completely [Figure - 3]. The repeat complete hemogram, liver and renal function tests at the end of 2 months were normal. The patient had no side effects with ceftriaxone. Currently, the patient is under follow-up for 30 days with no recurrence.
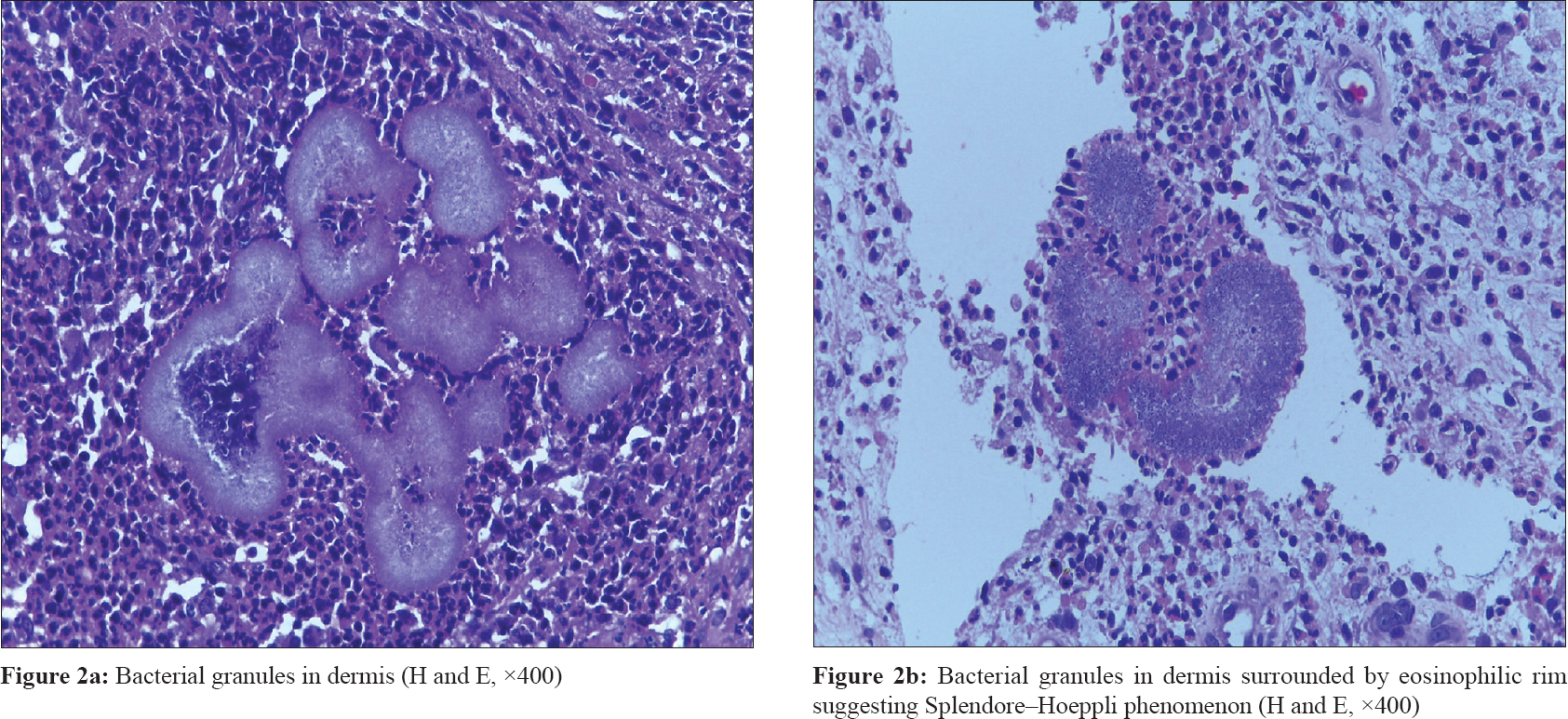 |
| Figure 2 |
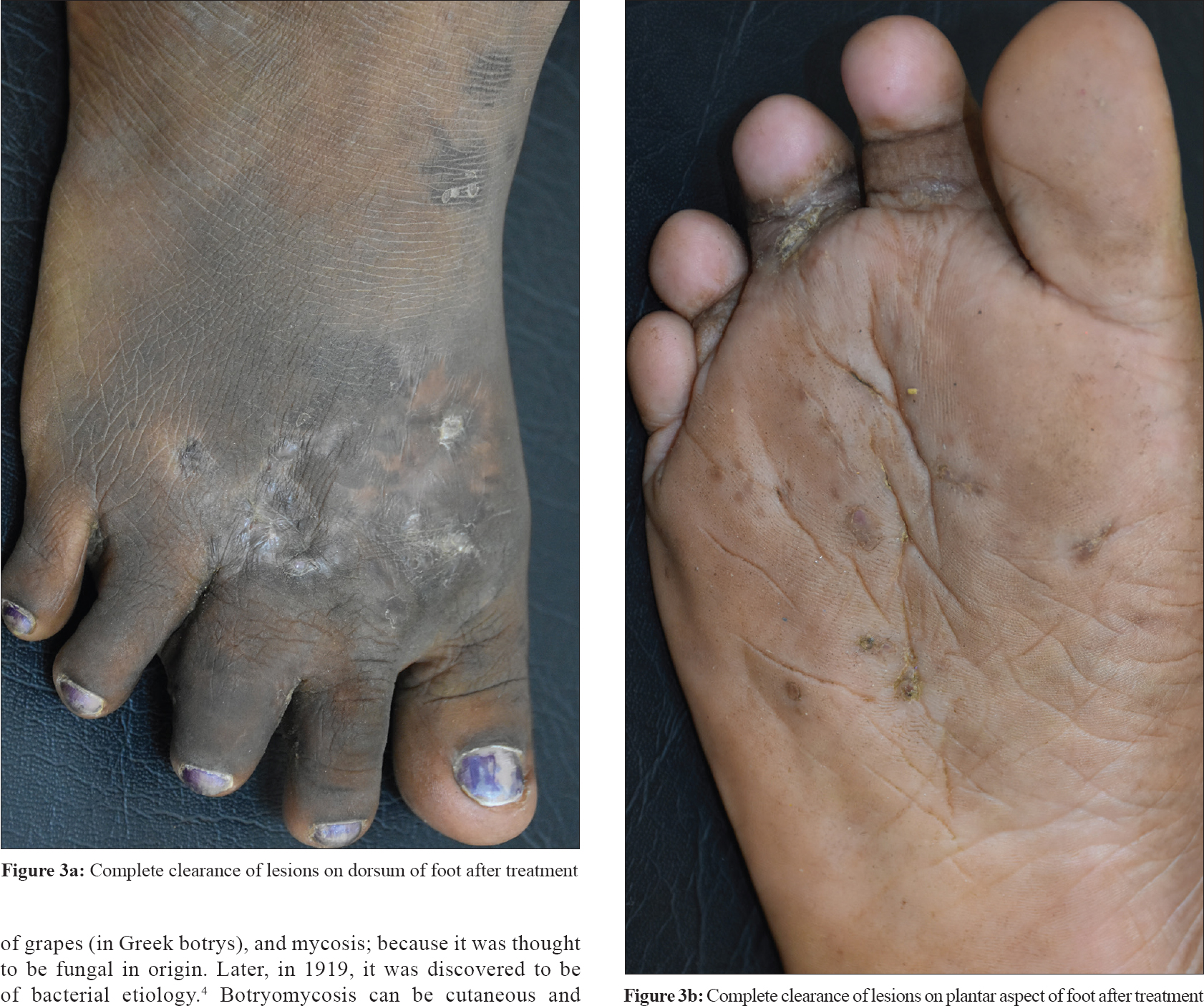 |
| Figure 3 |
The term botryomycosis was coined by Rivolta in 1884. The bacteria form granules deep in the tissue and resemble bunches of grapes (in Greek botrys), and mycosis; because it was thought to be fungal in origin. Later, in 1919, it was discovered to be of bacterial etiology.[4] Botryomycosis can be cutaneous and visceral. Cutaneous lesion account for 75% whereas rest is visceral form.[5]
Staphylococcus aureus is incriminated in 40% cases, followed by Pseudomonas aeruginosa 20%. Other organisms include coagulase-negative staphylococci, Streptococcus spp., Escherichia coli and Proteus spp.[3] The predisposing factors include altered immune function and comorbid conditions such as diabetes mellitus, liver disease, alcoholism, lupus, cystic fibrosis, asthma, malnutrition, immunoglobulin deficiency, hyperglobulinemia E (Job syndrome), glomerulonephritis, treatment with corticosteroids and human immunodeficiency virus/acquired immunodeficiency syndrome.[6],[7] The local factors such as accident and postoperative skin trauma are also incriminated.[8]
It is believed that grouping and clustering (grains) of organism is responsible for resistance named as Splendore–Hoeppli phenomenon.[5],[8],[9] The Splendore–Hoeppli phenomenon represents presence of an antigen–antibody complex, tissue debris and fibrin that generate an eosinophilic matrix among bacterial granules in botryomycosis which prevents phagocytosis and intracellular destruction of the bacteria leading to chronic infection and thereby requires prolonged treatment. In our case, the patient had thorn prick injury at the site following which the lesions appeared. The reported patients were either adult or elderly patients and majority were immunosuppressed. Our case was a child and there are countable reports of botryomycosis in child. Treatment of botryomycosis is usually prolonged duration of antibiotic. Most often more than one antibiotic is used. However, appropriate antibiotics in combination with surgical excision is the most effective therapy for botryomycosis.[3]
Our case had botryomycosis involving the whole right foot with causative organism being MSSA. The lesions were completely cured with injectable ceftriaxone sodium as a monotherapy. We report the case for rarity in an immunocompetent child and complete cure with ceftriaxone monotherapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initial will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Bonifaz A, Carrasco E. Botryomycosis. Int J Dermatol 1996;35:381-8.
[Google Scholar]
|
| 2. |
Machado CR, Schubach AO, Conceição-Silva F, Quintella LP, Lourenço MC, Carregal E, et al. Botryomycosis. Dermatology. 2005;211:303-4.
[Google Scholar]
|
| 3. |
Padilla-Desgarennes C, Vázquez-González D, Bonifaz A. Botryomycosis. Clin Dermatol 2012;30:397-402.
[Google Scholar]
|
| 4. |
Bonifaz A, Carrasco E. Botryomycosis. Int J Dermatol. 1996;35:381–8.
[Google Scholar]
|
| 5. |
Bersoff-Matcha SJ, Roper CC, Liapis H, Little JR. Primary pulmonary botryomycosis: Case report and review. Clin Infect Dis 1998;26:620-4.
[Google Scholar]
|
| 6. |
Vasishta RK, Gupta N, Kakkar N. Botryomycosis–A series of six integumentary or visceral cases from India. Ann Trop Med Parasitol 2004;98:623-9.
[Google Scholar]
|
| 7. |
Saadat P, Ram R, Sohrabian S, Vadmal MS. Botryomycosis caused by Staphylococcus aureus and Pneumocystis carinii in a patient with acquired immunodeficiency disease. Clin Exp Dermatol 2008;33:266-9.
[Google Scholar]
|
| 8. |
Follows GA, Mathew J, Lucas S, Black MJ, Goodship TH. Cutaneous botryomycosis in a patient with lupus nephritis. Nephrol Dial Transplant 1998;13:3200-1.
[Google Scholar]
|
| 9. |
Akiyama H, Kanzaki H, Tada J, Arata J. Staphylococcus aureus infection on cut wounds in the mouse skin: Experimental staphylococcal botryomycosis. J Dermatol Sci 1996;11:234-8.
[Google Scholar]
|
Fulltext Views
6,503
PDF downloads
2,857





