Translate this page into:
Cutaneous epithelioid angiomatous nodule versus epithelioid hemangioma: A dilemma
2 Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Correspondence Address:
Rashmi Kumari
Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry - 605 006
India
| How to cite this article: Gupta D, Kumari R, Jacob SE, Rajesh NG, Thappa DM. Cutaneous epithelioid angiomatous nodule versus epithelioid hemangioma: A dilemma. Indian J Dermatol Venereol Leprol 2017;83:99-101 |
Sir,
Cutaneous epithelioid angiomatous nodule is a benign vascular proliferation. It overlaps significantly with epithelioid hemangioma both clinically and histologically and uncommon presentations of either of them can give rise to a diagnostic dilemma. Here, we report an unusual presentation of cutaneous epithelioid angiomatous nodule with multiple lesions and describe the clinical and histological overlap between cutaneous epithelioid angiomatous nodule and epithelioid hemangioma.
A 28-year-old man presented with slow-growing nodules on the left side of the abdomen for 6 months. On examination, multiple, dull red to skin-colored nodules were seen on the abdomen along the T7–T9 dermatome [Figure - 1]. The smaller nodules were dome-shaped with a smooth surface but larger ones appeared pedunculated with a rough scaly surface. The larger nodules were also surrounded by a rim of hyperpigmentation.
 |
| Figure 1: Smooth as well as scaly pedunculated nodules along T7–T9 dermatome |
Histopathology revealed a hyperkeratotic and acanthotic epidermis. Dermis showed a circumscribed lesion consisting of proliferating small- to medium-sized blood vessels arranged in a lobular architecture [Figure - 2]a. Some of the vessels were thick-walled and lined by plump epithelioid endothelial cells with enlarged nuclei, prominent nucleoli and cytoplasmic vacuoles [Figure - 2]b. These were arranged in solid sheets and were surrounded by myxoid stroma [Figure - 3]a. A perivascular infiltrate of lymphocytes and eosinophils, was present [Figure - 3]b. The endothelial cells stained positive for CD34 and CD31 [Figure - 3]c. Nuclear atypia, hyperchromasia and mitotic figures were absent. Warthin–Starry and Giemsa stains for Bartonella henselae and cultures for deep fungal and mycobacterial infections were negative. A magnetic resonance imaging scan revealed the plane of the swelling to be limited to the subcutis.
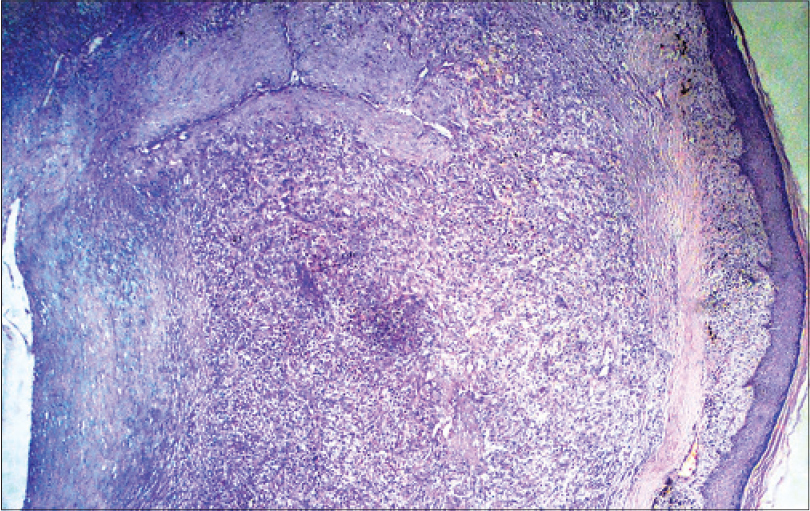 |
| Figure 2a: Small to medium-sized blood vessels arranged in a lobular architecture (H and E, ×400) |
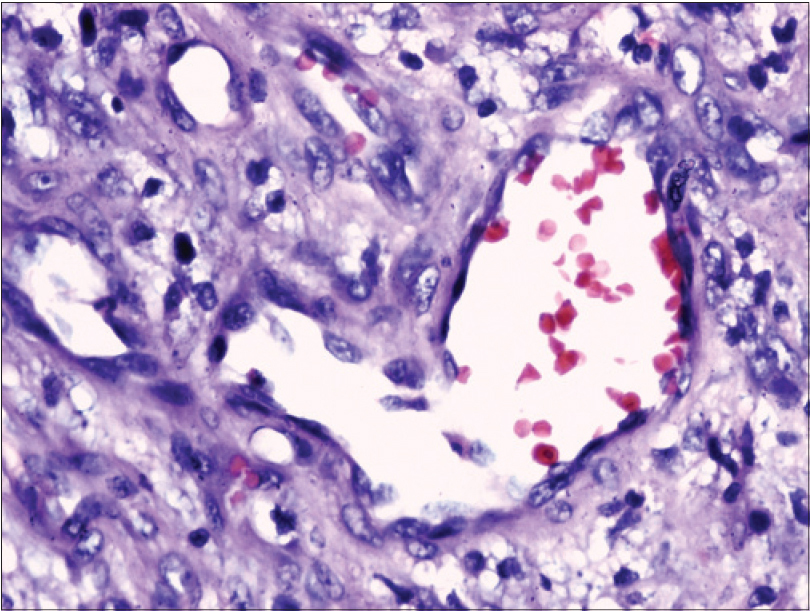 |
| Figure 2b: Blood vessels lined by plump endothelial cells with cytoplasmic vacuoles (H and E, ×400) |
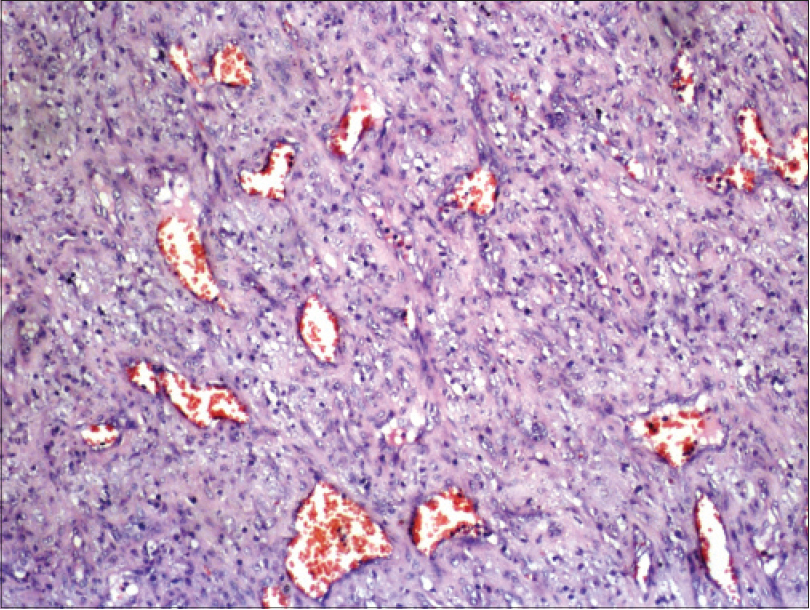 |
| Figure 3a: Solid sheets of epithelioid endothelial cells around the blood vessels (H and E, ×100) |
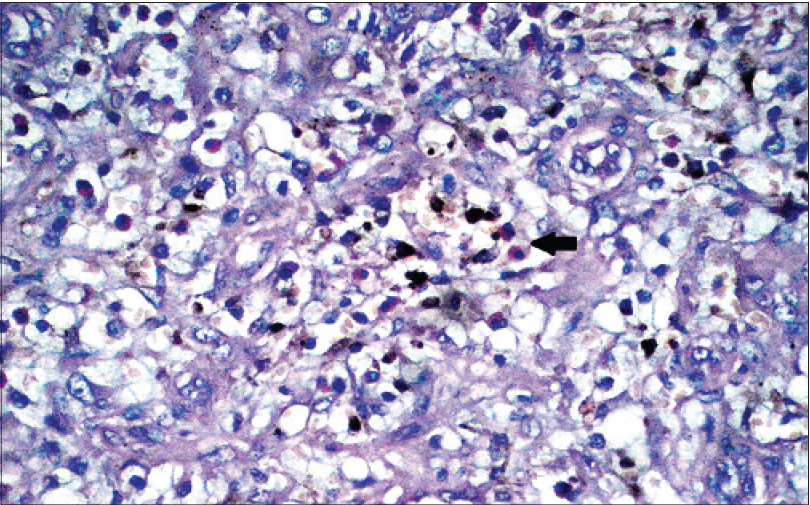 |
| Figure 3b: Inflammatory infiltrate composed of lymphocytes and eosinophils (arrow) (H and E, ×200) |
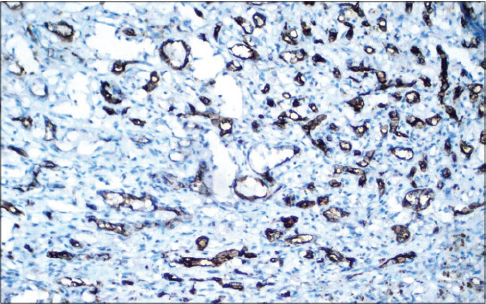 |
| Figure 3c: CD34 positivity of the endothelial cells (×100) |
Based on the above, a diagnosis of cutaneous epithelioid angiomatous nodule was made. Staged excision of the lesions was carried out without any recurrence at 6-month follow-up.
We found 55 previously reported cases of cutaneous epithelioid angiomatous nodule, with multiple lesions reported in 7 cases.[1],[2],[3],[4],[5] The original series of 15 cases of cutaneous epithelioid angiomatous nodule, described by Brenn and Fletcher, also had a considerable overlap with epithelioid hemangioma, two cases described had a facial distribution and three had deeper extension into the dermis/subcutis.[6] Subsequently, Sangüeza et al. noted that cutaneous epithelioid angiomatous nodule had features similar to epithelioid hemangioma.[7] In their study, the head and neck was the most common site, 30% of cases were located in the deep dermis and recurrence was seen in 20% of cases. Most recently, Pavlidakey et al. reviewed 51 cases of cutaneous epithelioid angiomatous nodule.[1] The common sites in decreasing order were the head and neck, trunk, extremities and vulva. Five patients with cutaneous epithelioid angiomatous nodule had multiple lesions.[1] Since then, two more cases of multiple cutaneous epithelioid angiomatous nodules have been reported.[2],[3], Misago et al. described a case of cutaneous epithelioid angiomatous nodule with extension into subcutis and involvement of medium-sized veins.[8] All these reports point towards a significant overlap between cutaneous epithelioid angiomatous nodule and epithelioid hemangioma.
These entities are similar in that they are both benign clusters of papules and nodules occurring in a localized anatomic region with onset in early adulthood. Histology in both shows lobularity, inflammatory infiltrate composed of lymphocytes and eosinophils, epithelioid endothelial cells with vesicular nuclei, prominent nucleoli and absence of nuclear atypia.[6],[7], Nevertheless, cutaneous epithelioid angiomatous nodule can be differentiated from epithelioid hemangioma by subtle but distinct clinical and histological features. Clinically, the former presents as a single lesion, usually on the trunk and extremities, which does not recur after excision, whereas the latter presents as multiple lesions, mostly on the head and neck area, with a tendency for recurrence. Histologically, cutaneous epithelioid angiomatous nodule is usually unilobular, limited to the superficial dermis and shows solid proliferation of epithelioid endothelial cells, hemosiderin deposition, lack of thick vasoformative structures and muscular vessels and a less abundant infiltrate of lymphocytes and eosinophils. Fibrosis is usually present and is seen in a perilesional distribution at the interface with the surrounding dermis.[1],[6],[7] By comparison, epithelioid hemangioma has multilobular vessel proliferation, usually extends to the deep dermis/subcutis and lacks solid proliferation of epithelioid endothelial cells, fibrosis and hemosiderin deposition. Fibrosis (when encountered) is located within the lesion, rather than perilesionally. Thick vasoformative structures and muscular vessels are usually present along with an abundant infiltrate of lymphocytes and eosinophils.[6],[7],
In our case, absence of infiltrative growth pattern, nuclear atypia, atypical mitotic figures and deep soft tissue and internal organ involvement helped us rule out epithelioid angiosarcoma and epithelioid hemangioendothelioma. Cutaneous epithelioid angiomatous nodule is a circumscribed lesion and although mitosis may be seen, atypical mitosis is absent.
In conclusion, our patient showed features of both cutaneous epithelioid angiomatous nodule (i.e., lesions on the trunk, solid sheets of epithelioid endothelial cells, mild eosinophilic and lymphocytic infiltrate, fibromyxoid stroma, hemosiderin deposition, no recurrence after excision) and epithelioid hemangioma (i.e., multiple lesions, involvement of medium-sized vessels and extension into subcutis). The main features of epithelioid endothelial cells and inflammatory infiltrates are shared by cutaneous epithelioid angiomatous nodule and epithelioid hemangioma and there can be varying expressions of these in both. The vascular channels can be collapsed with endothelial cells forming solid sheets and inflammatory infiltrates scant in epithelioid hemangioma, allowing for significant overlap with cutaneous epithelioid angiomatous nodule. Thus, cutaneous epithelioid angiomatous nodule may be considered as a variant of epithelioid hemangioma rather than a separate histological and clinical disorder.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Pavlidakey PG, Burroughs C, Karrs T, Somach SC. Cutaneous epithelioid angiomatous nodule: A case with metachronous lesions. Am J Dermatopathol 2011;33:831-4.
[Google Scholar]
|
| 2. |
Labbène I, Rammeh S, Znaidi N, Fazaa B, Zermani R. A case of multiple epithelioid angiomatous nodules. Dermatol Online J 2012;18:8.
[Google Scholar]
|
| 3. |
Dastgheib L, Aslani FS, Sepaskhah M, Saki N, Motevalli D. A young woman with multiple cutaneous epithelioid angiomatous nodules (CEAN) on her forearm: A case report and follow-up of therapeutic intervention. Dermatol Online J 2013;19:1.
[Google Scholar]
|
| 4. |
Lo CS, Lee MC. Case of a cutaneous epithelioid angiomatous nodule on the foot. J Dermatol 2013;40:480-1.
[Google Scholar]
|
| 5. |
Okano S, Takahara M, Tanaka M, Nakahara T, Suzuki H, Fujii H, et al. Cutaneous epithelioid angiomatous nodule in a patient with a history of multiple pyogenic granulomas. Eur J Dermatol 2015;25:268-9.
[Google Scholar]
|
| 6. |
Brenn T, Fletcher CD. Cutaneous epithelioid angiomatous nodule: A distinct lesion in the morphologic spectrum of epithelioid vascular tumors. Am J Dermatopathol 2004;26:14-21.
[Google Scholar]
|
| 7. |
Sangüeza OP, Walsh SN, Sheehan DJ, Orland AF, Llombart B, Requena L. Cutaneous epithelioid angiomatous nodule: A case series and proposed classification. Am J Dermatopathol 2008;30:16-20.
[Google Scholar]
|
| 8. |
Misago N, Inoue T, Narisawa Y. Subcutaneous epithelioid angiomatous nodule: A variant of epithelioid hemangioma. J Dermatol 2006;33:73-4.
[Google Scholar]
|
Fulltext Views
4,500
PDF downloads
2,548





