Translate this page into:
Cutaneous inflammation as a marker of malignant transformation in a patient with linear unilateral basaloid follicular hamartoma
2 Department of Pathology, School of Medicine, Pontificia Universidad Católica de Chile, Santiago, Chile
3 Department of Dermatology, School of Medicine; Department of Dermatology, School of Medicine, Connective Tissue Diseases Unit, Pontificia Universidad Católica de Chile, Santiago, Chile
Correspondence Address:
Cristián Vera-Kellet
Av. Vicuña Mackenna 4686, Macul, Santiago de Chile
Chile
| How to cite this article: Del Barrio-Diaz P, Meza-Romero R, González S, Vera-Kellet C. Cutaneous inflammation as a marker of malignant transformation in a patient with linear unilateral basaloid follicular hamartoma. Indian J Dermatol Venereol Leprol 2019;85:287-290 |
Abstract
Basaloid follicular hamartoma is a rare, benign and superficial malformation of hair follicles, characterized histologically by epithelial proliferation of basaloid cells with radial disposition. It can be mistaken for basal cell carcinoma. Even though these hamartomas are considered benign lesions, malignant transformation has rarely been reported. We report the case of a 45-year-old healthy woman, with linear, unilateral basaloid follicular hamartoma which developed inflamed papules histologically suggestive of basal cell carcinoma. We believe that identification of local inflammation could be a clinical clue to guide us towards a malignant transformation of basaloid follicular hamartoma.
Introduction
Basaloid follicular hamartoma is a rare, benign and superficial malformation of hair follicles, characterized histologically by epithelial proliferation of basaloid cells with radial disposition. It was first described in 1969 by Brown et al. in association with myasthenia gravis and diffuse alopecia.[1] Clinically, basaloid follicular hamartoma is characterized by solitary or multiple small, skin-colored to brownish papules or plaques, and may be either sporadic or hereditary.[2] Basaloid follicular hamartoma is a lesion of important consideration because it can be mistaken, both clinically and histologically, for basal cell carcinoma. Furthermore, malignant growths have been reported to arise within basaloid follicular hamartoma. We report the case of a patient with localized and unilateral basaloid follicular hamartoma, who developed multiple basal cell carcinomas within the inflamed sites of the hamartoma. We believe that local inflammation could be a clinical tool that could guide us toward a malignant transformation of basaloid follicular hamartoma.
Case Report
A 45-year-old healthy woman presented with a history of asymptomatic papules in a Blaschkoid distribution since childhood. There was no family history of skin disease. The physical examination revealed multiple shiny brown papules over her left hemithorax, left shoulder and left arm [Figure - 1]. Few papules on her cervical region, left nasolabial fold and pectoral region showed clinical signs of inflammation such as erythema and swelling [Figure - 2]. Dermatoscopic findings on this inflamed area showed pigmented areas associated with erythema [Figure - 3]. Histological analysis of a punch biopsy from the noninflamed papules located on left arm showed well-defined tumor composed of cords and nests of basaloid cells without retraction and cell stroma, compatible with basaloid follicular hamartoma [Figure - 4]. Histopathology of inflamed lesions from the cervical region, left nasolabial fold and pectoral region showed multiple nests of basaloid cells with peripheral palisade, mucofibrotic stroma and retraction clefts, histologically compatible with basal cell carcinomas [Figure - 5]. From the time of diagnosis, the patient has had more than 20 lesions excised which show histological features of basal cell carcinoma. Interestingly these were located only in the sites showing clinical inflammation within the basaloid follicular hamartoma.
 |
| Figure 1: Multiple shiny brown papules on left hemithorax |
 |
| Figure 2: Inflamed erythematous papules on pectoral region |
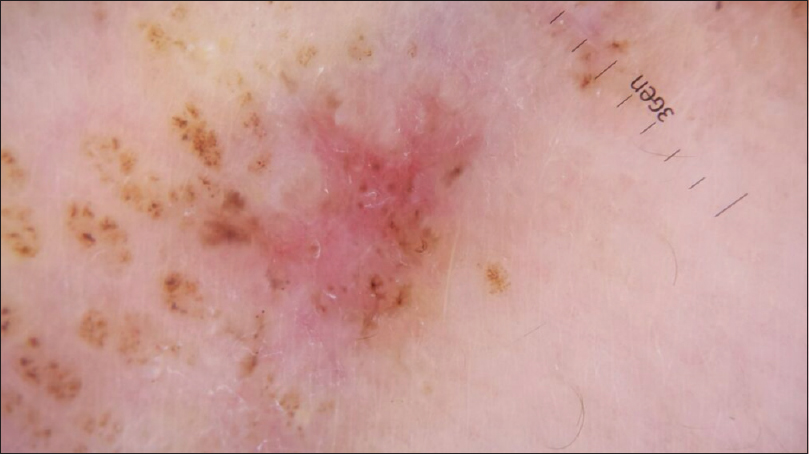 |
| Figure 3: Dermatoscopic features: pigmented areas associated with inflammation (polarized, �10) |
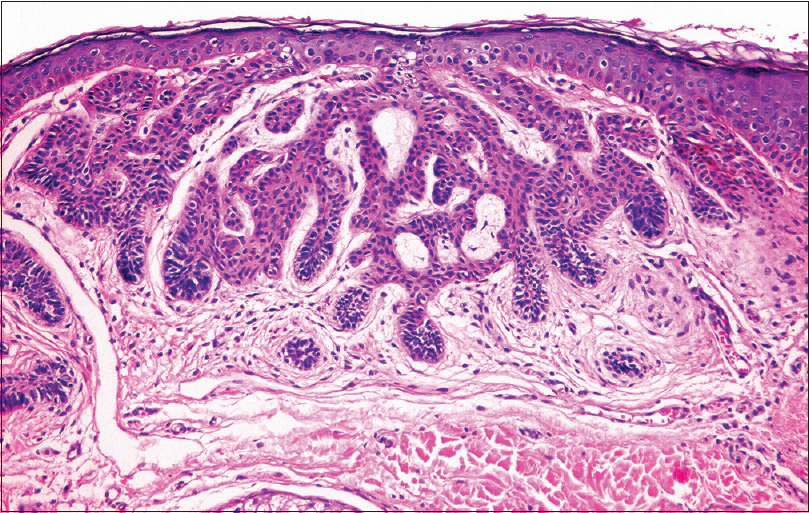 |
| Figure 4: Histology of lesional noninflamed skin showing well-defined tumor composed of cords and nests of basaloid cells without retraction and cell stroma, compatible with multiple basaloid follicular hamartoma (hematoxylin and eosin, �100) |
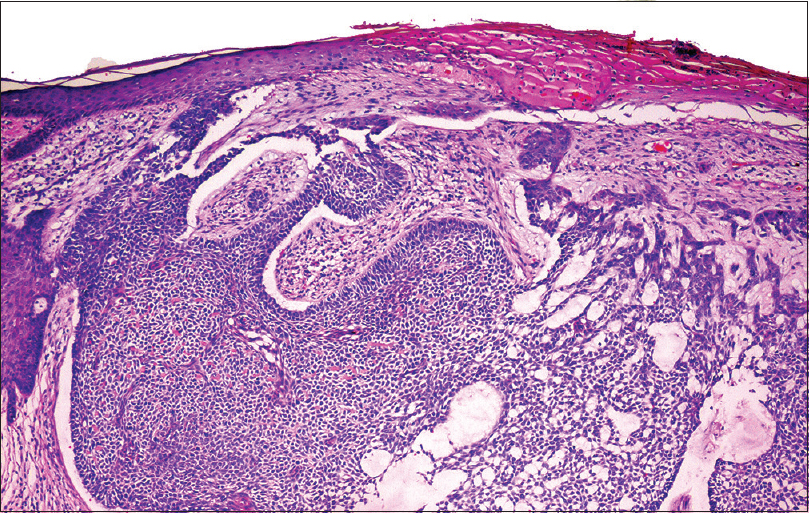 |
| Figure 5: Histology of lesional inflamed skin showing multiple nests of basaloid cells with peripheral palisade, mucofibrotic stroma and retraction clefts, compatible with basal cell carcinoma (hematoxylin and eosin, �100) |
Discussion
Basaloid follicular hamartoma is a rare follicular malformation with variable clinical presentations. It is characterized by single or multiple skin-colored papules, hypochromic macules and/or comedones, plaques and nodules mostly on the face, which may also appear in the axillae, pubic area and scalp.[2] The distribution may be localized or generalized. It may occur alone or in association with various systemic disorders such as Bazex–Dupré–Christol syndrome, myasthenia gravis, systemic lupus erythematosus, alopecia and cystic fibrosis.[3]
The localized form, as seen in our patient, is the most common and tends to be sporadic. It occurs at birth or during the first 20 years of life and is characterized by alopecic patches or unilateral linear lesions which follow the lines of Blaschko.[2],[4]
The generalized form is less common tends to be inherited.[2] Several subtypes of generalized basaloid follicular hamartoma have been noted: (1) sporadic: multiple lesions without systemic disease; (2) inherited: autosomal dominant disease which may be associated with hypotrichosis, hypohidrosis and palmoplantar pitting; (3) acquired: generalized basaloid follicular hamartoma associated with alopecia and autoimmune diseases such as myasthenia gravis or systemic lupus erythematosus; (4) congenital: generalized basaloid follicular hamartoma associated with alopecia and cystic fibrosis.[2],[5]
The differential diagnosis is broad and depends on the clinical form. In our patient, differential diagnoses included linear epidermal nevus, nevoid basal cell carcinoma syndrome and linear syringomas.[6]
Histopathology of basaloid follicular hamartoma is common to the different clinical variants and is characterized by epithelial basaloid cords emerging radially from the hair follicles, partially or totally replacing them.[3] Thus, the histopathological differential diagnosis includes all entities that have basaloid epithelial proliferations such as the infundibulocystic basal cell carcinoma, trichoepithelioma and folliculocentric basaloid proliferation.[3] However, there are some histological signs that differentiate infundibulocystic basal cell carcinoma from basaloid follicular hamartoma. For example, infundibulocystic basal cell carcinoma unlike basaloid follicular hamartoma is not a folliculocentric tumor, may be located in the interfollicular dermis. Pilosebaceous structures are usually destroyed and may have mitotic figures, deep infiltration, epidermal ulceration and neoplastic cells. Besides, infundibulocystic basal cell carcinoma has a more intense immunohistochemical staining for Ki-67, Bcl-2 and CD10, and negative for CD34.[3]
Even though the basaloid follicular hamartoma is a benign tumor, it has been described in the literature that the different clinical variants have an increased risk of basal cell carcinoma, which tends to arise de novo. This could be explained based on genetic studies, which have linked basaloid follicular hamartoma to mutations of the patched signaling pathway in locus near mutation sites causing basal cell carcinoma.[6]
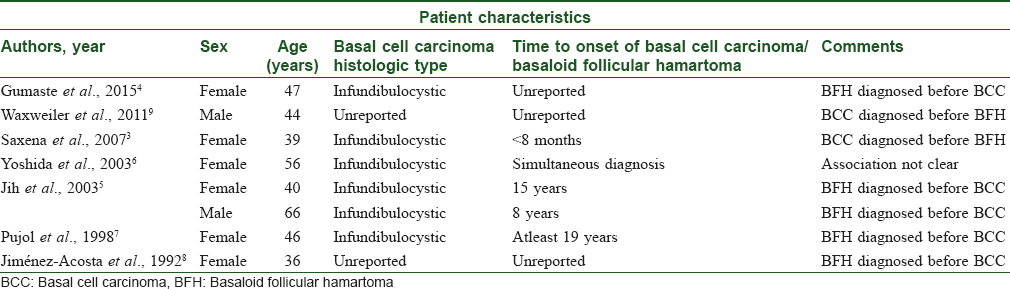
On a literature search, we found eight cases of basaloid follicular hamartoma related with basal cell carcinoma.[4],[5],[6],[7],[8],[9],[10] We have summarized their clinical features in [Table - 1]. Even though for some reports the relationship between basaloid follicular hamartoma and basal cell carcinoma is debatable, in our case we think that basal cell carcinomas arose from basaloid follicular hamartoma as basal cell carcinoma lesions appeared only at inflamed sites within the basaloid follicular hamartoma.
In summary, the importance of basaloid follicular hamartoma lies in the clinical and histological similarity with basal cell carcinoma and an increased risk of basal cell carcinoma de novo. We believe that local inflammation could be a clinical tool that could guide us toward malignant transformation of basaloid follicular hamartoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for the images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Brown AC, Crounse RG, Winkelmann RK. Generalized hair-follicle hamartoma: associated with alopecia, aminoaciduria and myasthenia gravis. Arch Dermatol 1969;99:478-93.
[Google Scholar]
|
| 2. |
Wheeler CE Jr., Carroll MA, Groben PA, Briggaman RA, Prose NS, Davis DA, et al. Autosomal dominantly inherited generalized basaloid follicular hamartoma syndrome: Report of a new disease in a North Carolina family. J Am Acad Dermatol 2000;43:189-206.
[Google Scholar]
|
| 3. |
Huang SH, Hsiao TF, Lee CC. Basaloid follicular hamartoma: A case report and review of the literature. Kaohsiung J Med Sci 2012;28:57-60.
[Google Scholar]
|
| 4. |
Saxena A, Shapiro M, Kasper DA, Fitzpatrick JE, Mellette JR Jr. Basaloid follicular hamartoma: A cautionary tale and review of the literature. Dermatol Surg 2007;33:1130-5.
[Google Scholar]
|
| 5. |
Gumaste P, Ortiz AE, Patel A, Baron J, Harris R, Barr R, et al. Generalized basaloid follicular hamartoma syndrome: A case report and review of the literature. Am J Dermatopathol 2015;37:e37-40.
[Google Scholar]
|
| 6. |
Jih DM, Shapiro M, James WD, Levin M, Gelfand J, Williams PT, et al. Familial basaloid follicular hamartoma: Lesional characterization and review of the literature. Am J Dermatopathol 2003;25:130-7.
[Google Scholar]
|
| 7. |
Yoshida Y, Urabe K, Mashino T, Duan H, Kiryu H, Masuda T, et al. Basal cell carcinomas in association with basaloid follicular hamartoma. Dermatology 2003;207:57-60.
[Google Scholar]
|
| 8. |
Pujol RM, Nadal C, Matias-Guiu X, Peyrí J, Ferrándiz C, Palou J, et al. Multiple follicular hamartomas with sweat gland and sebaceous differentiation, vermiculate atrophoderma, milia, hypotrichosis, and late development of multiple basal cell carcinomas. J Am Acad Dermatol 1998;39:853-7.
[Google Scholar]
|
| 9. |
Jiménez-Acosta FJ, Redondo E, Baez O, Hernandez B. Linear unilateral basaloid follicular hamartoma. J Am Acad Dermatol 1992;27:316-9.
[Google Scholar]
|
| 10. |
Waxweiler WT, Adigun CG, Groben P, Rubenstein DS. A novel phenotype with features of basal cell nevus syndrome and basaloid follicular hamartoma syndrome. J Am Acad Dermatol 2011;65:e17-9.
[Google Scholar]
|
Fulltext Views
3,981
PDF downloads
2,890





