Translate this page into:
Cutaneous larva migrans
2 Department of Pathology, Dr. R. P. Government Medical College, Kangra (Tanda), Himachal Pradesh, India
Correspondence Address:
Vikram K Mahajan
Department of Dermatology, Venereology and Leprosy, Dr. R. P. Government Medical College, Kangra (Tanda) 176 001, Himachal Pradesh
India
| How to cite this article: Upendra Y, Mahajan VK, Mehta KS, Chauhan PS, Chander B. Cutaneous larva migrans. Indian J Dermatol Venereol Leprol 2013;79:418-419 |
A 50-year-old female presented with multiple non-pruritic and mildly painful migratory erythematous curvilinear and serpiginous lesions of 1-week duration over her left wrist, base of left middle finger, and its knuckle and medial side of left index finger [Figure - 1]. She was an agriculturist and attributed her problem to handling compost the day before her visit. She had no associated cough, wheezing, or urticaria. Systemic examination and routine laboratory workup were essentially normal. Histological features of spongiosis and eosinophilic infiltrate were observed in a lesional biopsy [Figure - 2]. The lesions subsided within 5 days following a treatment with ivermectin (12 mg, PO) and albendazole (400 mg/day × 3 days, PO) with a diagnosis of cutaneous larva migrans.
Cutaneous larva migrans (syn, creeping eruption, sand worm eruption, plumbers itch, duck hunters itch) is caused by penetration of skin by third-stage larvae of animal hookworms; Ancylostoma brasiliense, A. caninum, A. ceylonicum, Uncineria stenocephala, and Bubostomum phlebotomum. A. brasiliense (dog hookworm) is the commonest cause of these creeping eruptions in humans who act as dead-end hosts. Adult hookworms infest the intestines of cats and dogs and their ova in excreta hatch under favorable conditions to infective larvae that penetrate the host skin. Warm, sandy, humid and shady fields, sandpits or sea shores are particularly favored areas; thus, predisposing the farmers, gardeners, hunters, or beach visitors to acquire the infection occupationally/accidently. Clinically itchy, erythematous, serpiginous raised lesions advancing at the rate of 2 mm to 3 cm per day develop in 1-6 days after the infection is acquired. Classic clinical picture may get superimposed with impetigo following secondary bacterial infection from repeated scratching. Bullous lesions and lesions with folliculitis or eczematization are other observed presentations. Cutaneous larva migrans may also be a cause of fever in HIV-infected patients. The body areas commonly affected are the dorsum of feet, buttocks, and, less commonly, dorsal hands. Lesions over anterior abdominal wall, penile shaft, perianal area, sole, or oral cavity may occur uncommonly. Breast lesions may occur in women from lying topless and prone in a tropical beach. More than one lesion may occur due to multiple entry points. As the larva survives in the human host for 2-4 weeks only, the disease is self limiting in over 80% cases. Symptoms like cough, wheezing, and chest pain are occasional, while pulmonary eosinophilia (Loeffler′s pneumonia) usually accompany severe infestation.
 |
| Figure 1: Erythematous curvilinear serpiginous lesions over dorsum of the left hand, middle finger, and medial aspect of index finger |
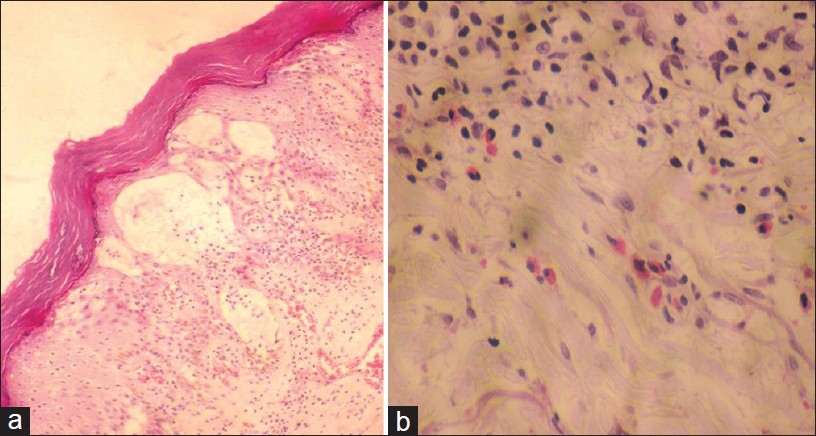 |
| Figure 2: Histology from a lesion showing orthokeratosis, multiple intraepidermal bullae, spongiosis, dilated vascular channels, lymphocytic exocytosis, and numerous eosinophils (H and E, × 10 (a), × 40 (b)) |
Diagnosis is from classic lesions, especially in occupationally exposed individuals or travelers returning from tropical regions. Peripheral eosinophilia is transient and may be associated with migratory pulmonary infiltrates or increased serum IgE levels of little diagnostic value. Skin biopsy is not helpful in the diagnosis and shows predominant eosinophilic infiltration, while larva is rarely seen as it would have advanced beyond the skin lesions. Epiluminescence microscopy is an effective, non-invasive method to confirm the diagnosis. The larva is visualized best at ×40 magnification as a translucent, brownish, segmented linear area, and the empty burrow as red dotted vessels. Examination under reflectance confocal microscope can be used for effectively visualizing highly refractile larva and dark disruption in the honeycomb epidermal pattern corresponding to the larval burrow. Recently, the identification of larva by optical coherence tomography has been found useful in its direct removal. Similar creeping lesions of larva currens are caused by Strongyloides stercoralis. Other differentials include cercarial dermatitis, curvilinear lesions of contact dermatitis, and migratory myiasis.
Currently, a single dose of ivermectin (200 μg/kg, PO) is first line therapy. Albendazole (400 mg/day, PO) for 3 days is also an effective alternative. The larva will eventually die and the cutaneous lesions resolve even without treatment in weeks to months. Cryosurgery with liquid nitrogen, ethyl chloride spray, or carbon dioxide slush is no longer recommended in view of highly effective anthelminthic drugs. Avoiding contact of bare skin with contaminated soil by covering the ground with impenetrable material or large beach towels while sitting or lying, wearing footwear, and avoiding bare feet walking, prohibiting dogs at beach area, and de-worming the pets are some suggested preventive measures.
Fulltext Views
12,287
PDF downloads
2,249





