Translate this page into:
Cutaneous manifestations of obesity among dermatology patients in a tertiary care center
Correspondence Address:
Kikkeri Narayanashetty Naveen
Department of Dermatology, OPD no. 10, SDM Medical College, Sattur, Dharwad 580 009, Karnataka
India
| How to cite this article: Divyashree RA, Naveen KN, Pai VV, Athanikar SB, Gupta G. Cutaneous manifestations of obesity among dermatology patients in a tertiary care center. Indian J Dermatol Venereol Leprol 2014;80:278 |
Sir,
Obesity is a major epidemic of the 21 st century and has led to a significant increase in the number of obese patients attending dermatology OPD. It is responsible for changes in skin barrier function, sebaceous glands and sebum production, sweat glands, lymphatics, collagen structure and function, wound healing, microcirculation and macrocirculation, and subcutaneous fat. Moreover, obesity is implicated in a wide spectrum of dermatologic diseases including acanthosis nigricans, acrochordons, keratosis pilaris, hirsutism, striae distensae, adiposis dolorosa and fat redistribution, lymphedema, chronic venous insufficiency, plantar hyperkeratosis, cellulitis, skin infections, hidradenitis suppurativa, psoriasis and tophaceous gout. [1]
The aim of this study was to determine the various cutaneous manifestations in obesity and analyse the relation with body mass index (BMI).
Obese patients (BMI > 30 kg/m 2 ) visiting the dermatology outpatient department, SDM Medical College and Hospital, Dharwad, were included in our study. All patients above 15 years of age were included and patients exposed to factors known to be responsible for causing obesity, pregnant and lactating mothers, severely ill and immune compromised patients were excluded. After taking consent, demographic details, height, weight and cutaneous examination, findings were recorded. Relevant investigations if required, were carried out. This study was conducted after taking clearance from the institute ethics committee.
A total of 100 cases were studied, of which 74 were female and 26 were male. Of the total patients, 30% belonged to the 41-50 year age group followed by 20% in the 51-60 year age group, 16% belonged to the 21-30 year age group, 15% belonged to the 31-40 year and 61-70 year age group, and 2% belonged to the <20 and >70 year age group. Sixty two patients had a family history of obesity while 35 patients had associated systemic diseases (hypertension in 18, diabetes in 2, and diabetes with hypertension in 15 patients). Majority of the patients (68%) had Class I obesity (BMI of 30.00-34.99) while 23% had Class II obesity (BMI of 35.00-39.99), and 9% had Class III obesity (BMI of ≥ 40.00).
The various cutaneous changes seen in our study included infections, acanthosis nigricans, skin tags, plantar hyperkeratosis, striae, and chronic lymphedema. The most common skin condition among obese patients in all age groups was skin tags except the 21-30 year group in which acanthosis nigricans was the commonest skin finding. [Figure - 1] and [Figure - 2]. Specifically, among patients with Class 1 obesity (BMI of 30.00-34.99), the most common skin change was skin tags (67.6%), followed by acanthosis nigricans, plantar hyperkeratosis, fungal infection and intertrigo, striae, and bacterial infections [Figure - 3]. Chronic lymphedema was seen in only two patients. Patients with associated diseases such as hypertension and diabetes also showed skin tags and acanthosis nigricans as the most common skin manifestation [Figure - 4].
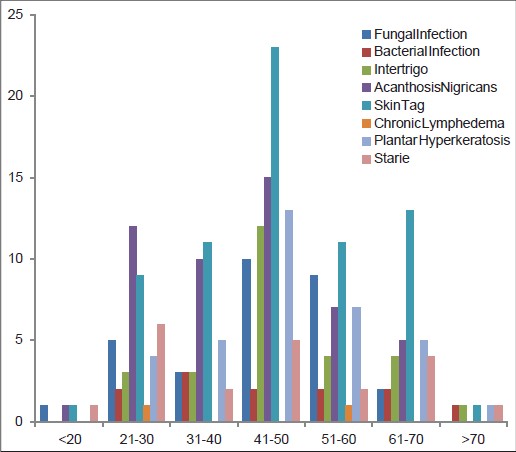 |
| Figure 1: Distribution of the cutaneous manifestations among obese patients according to age |
 |
| Figure 2: Skin tag and acanthosis nigricans |
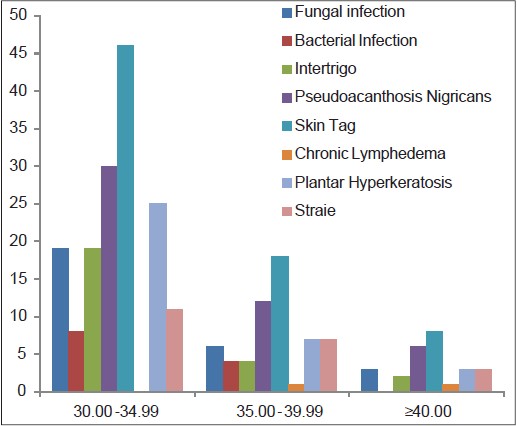 |
| Figure 3: Distribution of cutaneous manifestations among obese patients according to BMI |
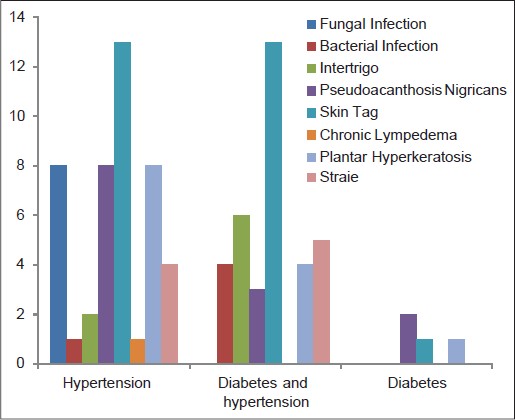 |
| Figure 4: Distribution of cutaneous manifestations among obese patients with associated diseases |
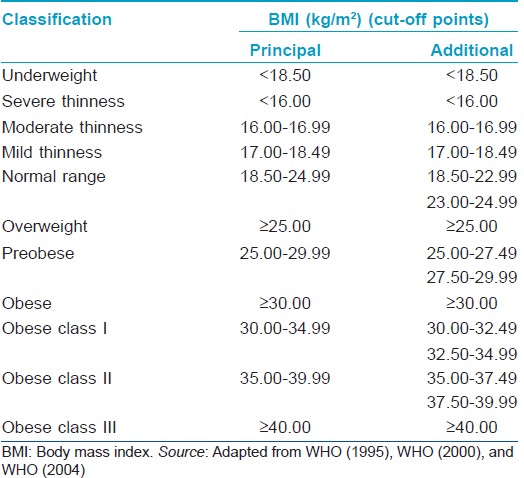
Obesity is defined and classified based on the BMI [Table - 1]. [2] Dermatological changes have been reported in patients with obesity, especially bacterial and fungal infections in skin folds due to occlusion, striae distensae due to skin stretching, stasis pigmentation related to peripheral vascular disease, acanthosis nigricans and skin tags secondary to insulin resistance, and plantar hyperkeratosis due to increased weight. [3]
In a comparative study performed by Boza et al., [4] dermatoses that showed a statistically significant relationship with obesity, compared with the control group, were: Striae (P < 0.001), plantar hyperkeratosis (P < 0.001), acrochordons (P = 0.007), intertrigo (P < 0.001), pseudoacanthosis nigricans (P < 0.001), keratosis pilaris (P = 0.006), lymphedema (P = 0.002), and bacterial infections (P = 0.05). The presence of striae, pseudoacanthosis nigricans, and bacterial infections were also found to correlate with the degree of obesity.
In another study among obese school children conducted in Saudi Arabia, [5] the skin conditions that were statistically significantly associated with obesity included dandruff, acne, xerosis, acanthosis nigricans, folliculitis, alopecia, striae, and callosities.
In our study, the skin conditions associated with obesity were skin tags, acanthosis nigricans, plantar hyperkeratosis, fungal infections and intertrigo, striae, bacterial infection, and lymphedema. Overall, fungal infections and intertrigo were found to be more common in obese individuals compared to bacterial infections. Lymphedema was seen in two patients with class II and class III obesity. The results for plantar hyperkeratosis were almost the same (36.7% for class I, 30% for class II, and 37.5% for class III obesity) among patients with different class of obesity. Striae showed a higher prevalence among class II obesity patients (30.4%).
| 1. |
Yosipovitch G, DeVore A, Dawn A. Obesityandthe skin: Skinphysiology and skin manifestations of obesity. J Am Acad Dermatol 2007;56:901-16.
[Google Scholar]
|
| 2. |
World Health Organization. Obesity: Preventing and managing the global epidemic of obesity. Report of the WHO Consultation of Obesity. Geneva, Switzerland : World Health Organization; 1997.
[Google Scholar]
|
| 3. |
García Hidalgo L. Dermatological complications of obesity. Am J Clin Dermatol 2002;3:497 - 506.
[Google Scholar]
|
| 4. |
Boza JC, Trindade EN, Peruzzo J, Sachett L, Rech L, Cestari TF. Skin manifestations of obesity: Acomparative study. J Eur Acad Dermatol Venereol 2012;26:1220-3.
[Google Scholar]
|
| 5. |
Al-Saeed WY, Al-Dawood KM, Bukhari IA, Bahnassy A. Dermatoses in obese female schoolchildren in the Al-Khobar area, Eastern Saudi Arabia. J Family Community Med 2006;13:65-9.
[Google Scholar]
|
Fulltext Views
4,282
PDF downloads
2,563





