Translate this page into:
Cutaneous mastocytosis: Report of six cases
Correspondence Address:
Arun C Inamadar
Department of Dermatology, Venereology and Leprology, BLDEA's SBMP Medical College, Hospital and Research Centre, Bijapur 586103, Karnataka
India
| How to cite this article: Inamadar AC, Palit A. Cutaneous mastocytosis: Report of six cases. Indian J Dermatol Venereol Leprol 2006;72:50-53 |
Abstract
Cutaneous mastocytosis is a rare infiltrative disorder of the skin. Though often asymptomatic, systemic features may be associated with any clinical pattern of the disorder at any age group. We present our experience with six cases of cutaneous mastocytosis, including three with diffuse cutaneous mastocytosis, a rare entity.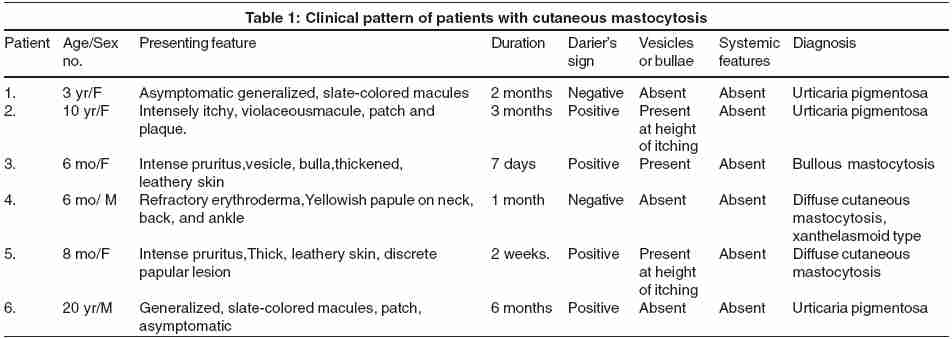
 |
 |
 |
 |
 |
 |
INTRODUCTION
Mast cells are naturally distributed in the dermis, respiratory, gastrointestinal, and genitourinary mucosa, adjacent to the blood vessels, lymphatics, and peripheral nerves.[1] These are the source of various preformed, biologically active substances that are released from the cell by the process of degranulation. An increase in the number of mast cells is observed in a variety of inflammatory dermatoses and in systemic disorders such as polycythemia rubra vera and chronic renal failure.[1] However, diffuse infiltration of one or more organs with mast cells gives rise to the clinical condition called mastocytosis. The most common site for an abnormal accumulation of mast cells is the skin,[2] known as cutaneous mastocytosis.
Cutaneous mastocytosis is a rare disorder. Cinical categories are urticaria pigmentosa, mastocytoma, diffuse cutaneous mastocytosis, and telangiectasia macularis eruptiva perstans (TMEP) in order of frequency of occurrence.[2] Diffuse cutaneous disease has two clinical variants, pseudoxanthomatous or xanthelasmoid and bullous type.[3] Urticaria pigmentosa and mastocytoma are the common clinical patterns seen in childhood. TMEP is commoner in adolescents and young adults, though childhood onset has been reported.[4] Darier′s sign, i.e, urtication of the lesional skin following firm stroking, is pathognomonic of this disorder. We report on six cases of cutaneous mastocytosis with varied clinical presentations.
CASE REPORT
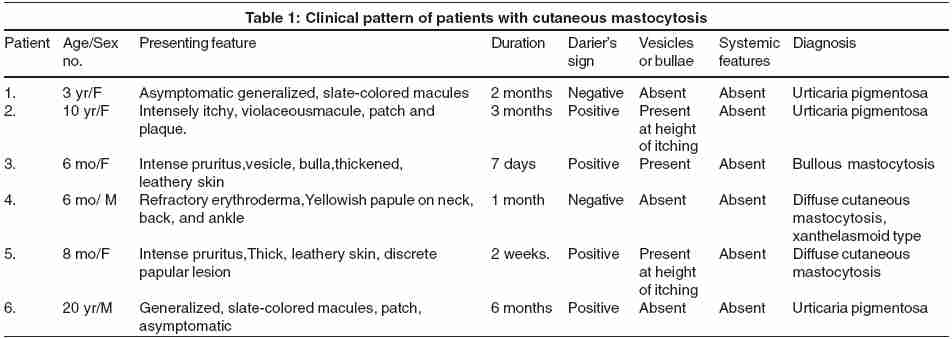
Six patients with cutaneous mastocytosis were examined over a period of 10 years in the dermatology outpatient department of a tertiary-care hospital. Three patients had urticaria pigmentosa and three had diffuse cutaneous mastocytosis. Their clinical presentation is described in [Table - 1].
We initially diagnosed patient 2 with urticaria pigmentosa as lichen planus [Figure - 1]. Patient 3, who had bullous mastocytosis, was referred by a pediatrician with the diagnosis of staphylococcal scalded skin syndrome [Figure - 2]. Patient 4 presented with erythroderma, whose cause could not be immediately ascertained. Patient 6, the only adult patient, was asymptomatic, and presented for a routine pre-employment check-up. None of the patients had a family history of a similar disorder.
The diagnosis was confirmed by histopathological examination of H and E and toluidine blue-stained sections from representative lesions. Diffuse infiltration of mast cells till deeper dermis was seen in patient 5 [Figure - 3]. Routine hematological examination and urinalysis were normal in all patients. Bone marrow aspiration was advised for patients 4 and 5, but declined by their parents.
As patients 1 and 6 were asymptomatic, they were not prescribed any treatment. The parents of the affected children were counseled about careful handling and avoidance of rubbing and toweling. The adult patient was advised to avoid undue exertion. All were advised to avoid exposure to specific drugs.
Symptomatic patients were treated with hydroxyzine (2 mg/kg/day 8 hourly) and oral ketotifen (1 mg OD) with subjective improvement of symptoms while on treatment. Patient 2, who had urticaria pigmentosa, stopped developing urticated lesions and bullae after 3 months of treatment.
Patients 3-5 were administered short courses of prednisolone (1 mg/kg) along with antihistamines. Patient 3 needed initial treatment of 3 weeks for complete clearance of the vesicles. Patients 4 and 5 showed significant improvement of pruritus and flattening of the lesions following 2 weeks of treatment with prednisolone and continued with antihistamines only. All the three patients showed recurrence subsequently-the patient with bullous mastocytosis showed this after 1.5 years whereas the other two within a few months. All the patients have been kept under follow-up.
DISCUSSION
Cutaneous mastocytosis is a rare, mostly sporadic disorder. Familial occurrence has been reported in 50 families to date.[4] Typical childhood disease is linked to Glu-839-Lyc c-kit mutation, whereas adult disease (as well as systemic disease) is often linked to a Asp-816-Val c-kit mutation.[5] Familial cases lack the c -kit mutation that is responsible for enhanced mast cell proliferation in this disorder and may represent a subgroup of the disease.[6]
A skin biopsy and demonstration of diffuse mast cell infiltration in the involved skin confirms the diagnosis. The pattern of collection of mast cells depends on the clinical types. A skin biopsy should be taken with due care so as not to degranulate the mast cells, which may result in a false-negative report. Cytological examination of a smear made by scraping the floor of a ruptured bulla shows numerous mast cells, thus helping in making a diagnosis quickly.[7]
Individual cases of bullous mastocytosis,[8] diffuse cutaneous disease,[9] and the pseudoxanthomatous subtype,[10] like our third, fourth, and fifth patients, have been reported from India. In a series of Indian children with cutaneous mastocytosis,[11] the commonest clinical pattern observed was urticaria pigmentosa. We observed equal numbers of patients of urticaria pigmentosa and diffuse cutaneous mastocytosis. Among our six patients, only one was an adult. Darier′s sign was negative in two patients. None of our patients had systemic symptoms or evidence of other organ involvement.
Though the histopathological features of cutaneous mastocytosis are characteristic, the clinical picture may simulate other disorders, as was seen in two of our patients. Vesiculobullous lesions are frequently seen in pediatric patients with all forms of cutaneous mastocytosis, especially in the early stage of the disease.[3] Three of our patients had this feature. Bullous mastocytosis may be misdiagnosed as staphylococcal scalded skin syndrome,[7],[12],[13] erythema multiforme,[12] and epidermolysis bullosa.[13] In one report,[14] the lesions of urticaria pigmentosa in a child were initially diagnosed as the sequelae of physical abuse by the parents. In our second patient with urticaria pigmentosa, a few violaceous plaques resembled those of lichen planus and led to an initial misdiagnosis. The generalized erythroderma in the fourth child was a diagnostic challenge until the histopathology report was available.
Dramatic response to systemic steroids in a case of bullous mastocytosis was reported by Has et al .[7] In this regard, we have a similar experience. Systemic steroids brought rapid and long-lasting remission to the three children with bullous and diffuse cutaneous mastocytosis.
Cutaneous mastocytosis may mimic other dermatological conditions. Childhood disease may be asymptomatic in majority of the cases. Since clinical presentation of this disorder is varied, high index of suspicion is required for clinical diagnosis and needs confirmation by histopathological examination.
| 1. |
Weedon D. Cutaneous infiltrates-non-lymphoid. In : Weedon D, editor. Skin Pathology. 2nd ed. Edinburgh: Churchill Livingstone; 2002. p. 1057-93.
[Google Scholar]
|
| 2. |
Prendiville JS, Krol AL. Diseases of the dermis and subcutaneous tissues. In : Schachner LA, Hansen RC, editors. Pediatric Dermatology. 3rd ed. Edinburgh: Mosby; 2003. p. 713-67.
[Google Scholar]
|
| 3. |
Husak R, Blume-Peytavi U, Pfrommer C, Geilen CC, Goerdt S, Orfanos CE. Nodular and bullous cutaneous mastocytosis of the xanthelasmoid type: case report. Br J Dermatol 2001;144:355-8.
[Google Scholar]
|
| 4. |
Chang A, Tung RC, Schlesinger T, Bergfeld WF, Dijkstra J, Kahn TA. Familial cutaneous mastocytosis. Pediatr Dermatol 2001;18:271-6.
[Google Scholar]
|
| 5. |
Heide R, Tank B, Orange AP. Mastocytosis in childhood. Pediatr Dermatol 2002;19:357-81.
[Google Scholar]
|
| 6. |
Hartman K, Henz BM. Mastocytosis: recent advances in defining the disease. Br J Dermatol 2001;144:682-95.
[Google Scholar]
|
| 7. |
Has C, Misery L, David L, Cambazard F. Recurring staphylococcal scalded skin syndrome-like bullous mastocytosis: the utility of cytodiagnosis and the rapid regression with steroid. Pediatr Dermatol 2002;19:220-3.
[Google Scholar]
|
| 8. |
Verma KK, Bhat R, Singh MK. Bullous mastocytosis treated with oral betamethasone therapy. Indian J Pediatr 2004;71:261-3.
[Google Scholar]
|
| 9. |
Sethuraman G, Handa S, Radotra B, Kumar B. Diffuse cutaneous mastocytosis with bullae/bullous mastocytosis: a question of semantics. Pediatr Dermatol 1999;16:409-11.
[Google Scholar]
|
| 10. |
Jain R, Dogra S, Verma S, Mohanty SK, Handa S. Diffuse cutaneous mastocytosis: pseudoxanthomatous variant. J Dermatol 2002;29:354-6.
[Google Scholar]
|
| 11. |
Kanwar AJ, Sandhu K. Cutaneous mastocytosis in children: an Indian experience. Pediatr Dermatol 2005;22:85-7.
[Google Scholar]
|
| 12. |
Golitz LE, Weston W, Lane A. Bullous mastocytosis: diffuse cutaneous mastocytosis with extensive blisters mimicking scalded skin syndrome or erythema multiforme. Pediatr Dermatol 1984;1:288-94.
[Google Scholar]
|
| 13. |
Orange AP, Widowati S, Sukardi A, Vuzevski VD, van der Willigen A, Afiani HM. Diffuse cutaneous mastocytosis mimicking staphylococcal scalded skin syndrome: report of three cases. Pediatr Dermatol 1991;8:147-51.
[Google Scholar]
|
| 14. |
Gordon EM, Bernat JR, Jr, Ramos-Caro FA. Urticaria pigmentosa mistaken for child abuse. Pediatr Dermatol 1998;15:484-5.
[Google Scholar]
|
Fulltext Views
4,869
PDF downloads
1,612





