Translate this page into:
Cutaneous meningioma
2 Department of Radiodiagnosis, Dr. S. N. Medical College, Jodhpur, Rajasthan, India
3 Department of Neurosurgery, Dr. S. N. Medical College, Jodhpur, Rajasthan, India
Correspondence Address:
Swagat S Waghmare
Room No. 120, Interns Hostel, MDM Hospital, Shastri Nagar, Jodhpur, Rajasthan
India
| How to cite this article: Waghmare SS, Chaturvedi K, Kachhawa D, Garg S. Cutaneous meningioma. Indian J Dermatol Venereol Leprol 2016;82:200-202 |
Sir,
Meningothelial heterotopias or cutaneous meningiomas are lesions in the skin and soft tissue that have meningothelial elements. These tumors are difficult to diagnose clinically and histopathologically as they are rare. They may be associated with intracranial meningiomas and neurological deficits. [1] They can occur at various sites and are slow-growing tumors with a good prognosis. [2]
A 35-year-old man was seen at the outpatient clinic of the department of dermatology, Dr. S N Medical College, Jodhpur with complaints of two painless swellings on the scalp which he had developed over the last 3 years. The patient had a history of similar swellings on the scalp which were excised three times over 9 years but recurred after every excision. The initial surgery, 9 years ago, was for a swelling which he developed 3-4 months after suffering a head injury. He developed weakness of left upper and lower limb after the surgery. The swelling recurred in 5-6 months after this surgery. Subsequently, there was a recurrence of the lesion within 6 months after each surgery. Detailed records of the previous excisions were not available; a discharge summary mentioned the diagnosis of meningioma without details of the type or location of the tumor.
On examination, there were two distinct tumors on the scalp, the larger one, approximately 12 cm × 10 cm × 8 cm, located on the posterior parietal region in the midline and an adjacent smaller tumor measuring 6 cm × 6 cm × 6 cm located to the right. Lesions were firm, non-tender, non-pulsatile, and non-compressible with a rough surface and loss of hair. The parietal bone below the tumors appeared depressed because of previous surgeries [Figure - 1]a and b. A differential diagnosis of epidermal cyst, pilar cyst and cutaneous metastasis were considered along with the possibility of meningioma.
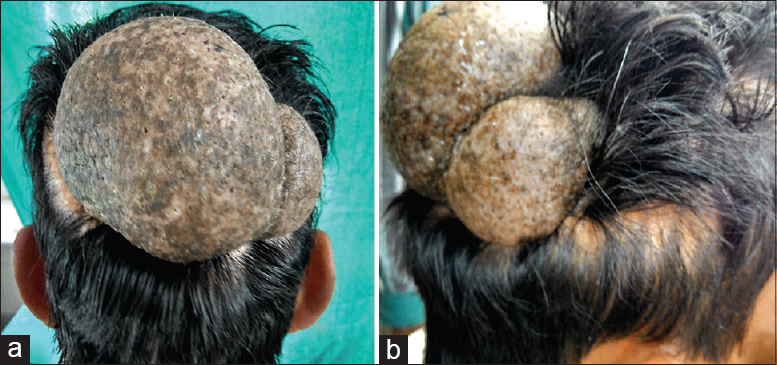 |
| Figure 1: (a and b) Tumors on scalp |
A computed tomography scan with contrast was performed considering the prior diagnosis of a meningioma. It showed a large bony defect in the right parietal region with a bi-lobed scalp lesion in the midline showing moderately enhancing soft tissue density. Although no evidence of an enhancing mass lesion was seen intracranially, there was presence of gliosis, suggestive of a previous intracranial mass. A preliminary diagnosis of postoperative meningocele with a recurrence of meningioma in a meningocele was entertained [Figure - 2]a-d.
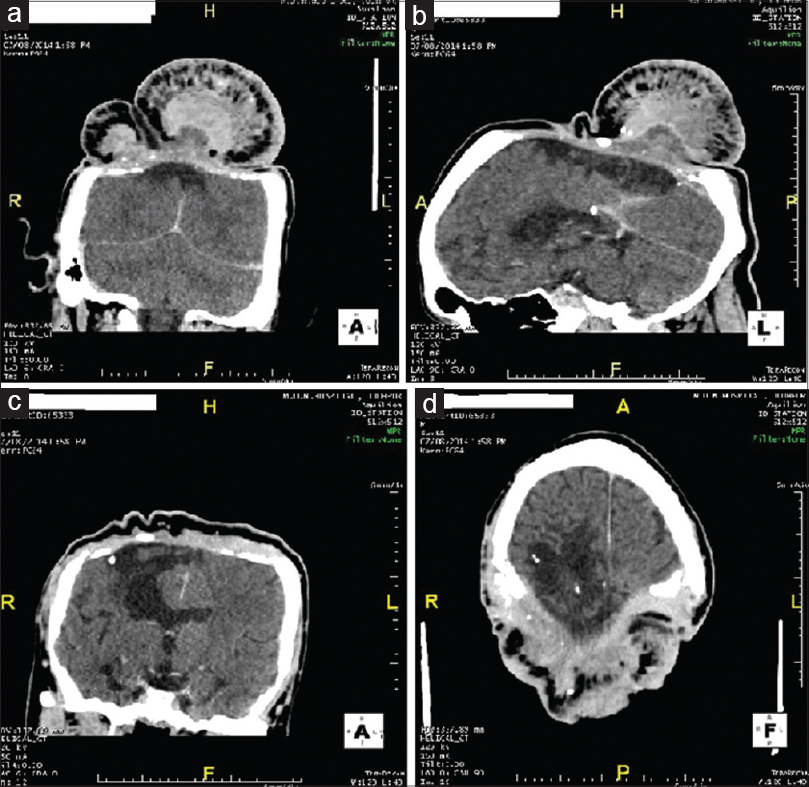 |
| Figure 2: Contrast-enhanced computed tomography image in coronal (a and b), sagittal (c) and axial plane (d) shows bony gap, intracranial gliotic changes in bilateral parafalcine and right occipitoparietal region with dystrophic calcific foci and enhancing soft tissue density mass lesion in midline parietal scalp swelling without any evidence of intracranial enhancing mass |
A punch biopsy from the smaller lesion showed dermal and subcutaneous clusters of meningothelial cells with finely granular chromatin and abundant pale cytoplasm with poorly defined cell margins imparting a syncytial appearance. No mitoses, pleomorphism or necrosis were seen. The background showed whorled collagen bundles. The findings were consistent with a cutaneous meningothelial meningioma.
Immunohistochemistry was positive for vimentin, progesterone receptor and epithelial membrane antigen (weak and focal) while ER, CK, HMB-45, S100, chromogranin and synaptophysin were negative confirming the diagnosis of extracranial meningioma, WHO grade 1, and ruling out metastatic melanocytic and neuroendocrine tumors [Figure - 3]a and b, [Figure - 4]a and b.
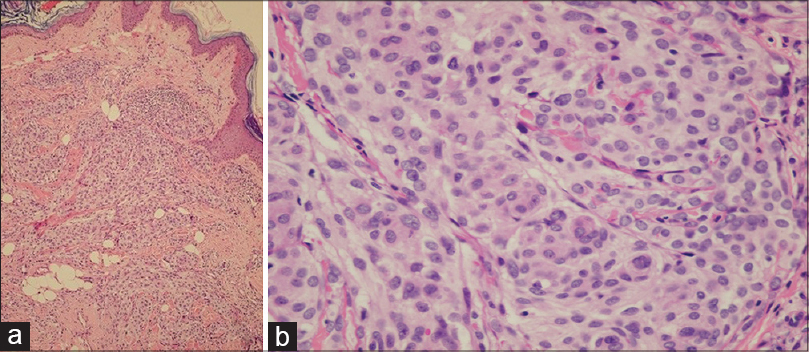 |
| Figure 3: (a and b) Meningothelial cells in dermis and subcutaneous tissue (H and E, ×100 and ×400) |
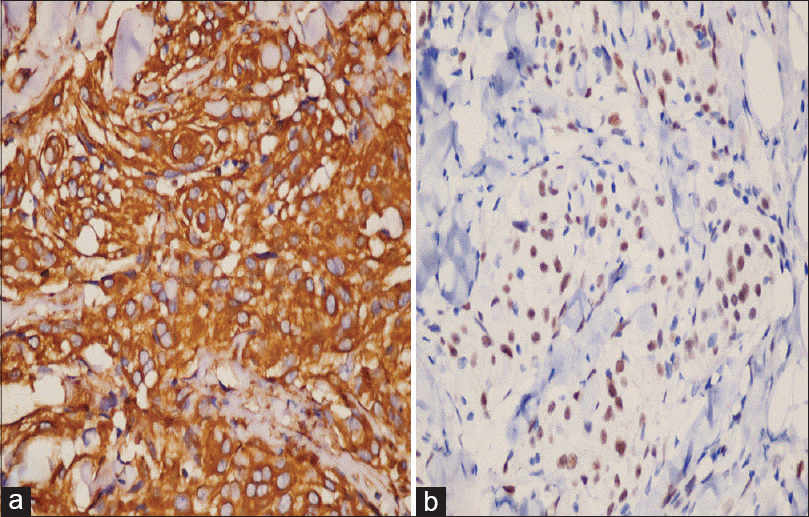 |
| Figure 4: Immunohistochemistry (a) strong positive for vimentin and (b) weak and focal positive for epithelial membrane antigen (×400) |
A diagnosis of cutaneous meningioma was established and the patient was referred to the neurosurgery department for excision but he declined surgery.
Intracranial meningiomas are common whereas extracranial ones are rare. Walters et al. explained their extracranial location by three mechanisms (1) direct extension of an intracranial meningioma through bone foramina (2) metastasis (3) primary ectopic meningioma. [3] There are reports of cutaneous meningioma occurring in a rudimentary meningocele [4] and due to the seeding of meningial cells into the skin and soft tissue following mechanical or surgical trauma. [3],[5],[6]
In a simple classification by Lopez et al., cutaneous meningiomas are classified into 3 types. Type 1 are congenital, arise from ectopic extracranial arachnoid cells and occur at a younger age. Type 2 are ectopic soft tissue meningiomas that are derived from arachnoid cells lining cranial and spinal nerves. They are commonly seen in adults. Type 3 are a direct extension of intracranial meningiomas to the exterior of the skull. [1],[7]
These tumors can be confused with various cysts, fibromas, hidradenomas, epithelioid sarcoma and metastatic tumors. [8] Histopathology and immunohistochemistry are needed to confirm the diagnosis. Magnetic resonance imaging and computed tomography imaging are helpful to diagnose type 3 cutaneous meningioma with intracranial involvement.
In our case, the initial tumor probably developed due to the seeding of meningeal cells of an asymptomatic intracranial meningioma through a post-traumatic defect in the skull or because of seeding of meningeal cells into a post-traumatic meningocele. Extracranial recurrences could be due to iatrogenic seeding of tumor cells extracranially into the skin and soft tissue. Moreover, after the first excision, the dura mater was probably coagulated and not excised which could explain the absence of intracranial recurrences. The neurological deficit in our patient could be because of a post-surgical complication of excision of intracranial meningioma during the surgery of the initial tumor, or because of post-surgical gliosis.
Acknowledgment
Dr. R. C. Purohit, Consultant Pathologist, Metropolis Healthcare C/o R P diagnostic center, Jodhpur, Rajasthan.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Lopez DA, Silvers DN, Helwig EB. Cutaneous meningiomas - A clinicopathologic study. Cancer 1974;34:728-44.
[Google Scholar]
|
| 2. |
Rushing EJ, Bouffard JP, McCall S, Olsen C, Mena H, Sandberg GD, et al. Primary extracranial meningiomas: An analysis of 146 cases. Head Neck Pathol 2009;3:116-30.
[Google Scholar]
|
| 3. |
Walters GA, Ragland RL, Knorr JR, Malhotra R, Gelber ND. Posttraumatic cutaneous meningioma of the face. AJNR Am J Neuroradiol 1994;15:393-5.
[Google Scholar]
|
| 4. |
Brantsch KD, Metzler G, Maennlin S, Breuninger H. A meningioma of the scalp that might have developed from a rudimentary meningocele. Clin Exp Dermatol 2009;34:e792-4.
[Google Scholar]
|
| 5. |
Tahir MZ, Shamim MS, Chishti KN. Recurrent atypical meningioma seeding to surgical scar. Neurol India 2009;57:222-4.
[Google Scholar]
|
| 6. |
Borggreven PA, de Graaf FH, van der Valk P, Leemans CR. Post-traumatic cutaneous meningioma. J Laryngol Otol 2004;118:228-30.
[Google Scholar]
|
| 7. |
Singh SK, Ojha BK, Chandra A, Rastogi M, Husain M, Husain N. Scalp meningioma. Indian J Dermatol 2008;53:196-8.
[Google Scholar]
|
| 8. |
Garcia-Zuazaga J, Ke MS, Willen M. Epidermoid cyst mimicry: Report of seven cases and review of the literature. J Clin Aesthet Dermatol 2009;2:28-33.
[Google Scholar]
|
Fulltext Views
4,609
PDF downloads
1,765





