Translate this page into:
Cutaneous metastasis from pancreatic cancer misdiagnosed as neuropathic foot ulcer
Corresponding author: Dr. Alvaro March-Rodríguez, Department of Dermatology, Hospital del Mar, Parc de Sault Mar, Barcelona, Spain. alvaromarch@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: March-Rodriguez A, Pesqué D, Lobato-Berezo A, Pujol RM. Cutaneous metastasis from pancreatic cancer misdiagnosed as neuropathic foot ulcer. Indian J Dermatol Venereol Leprol 2023;89:883-5.
Sir,
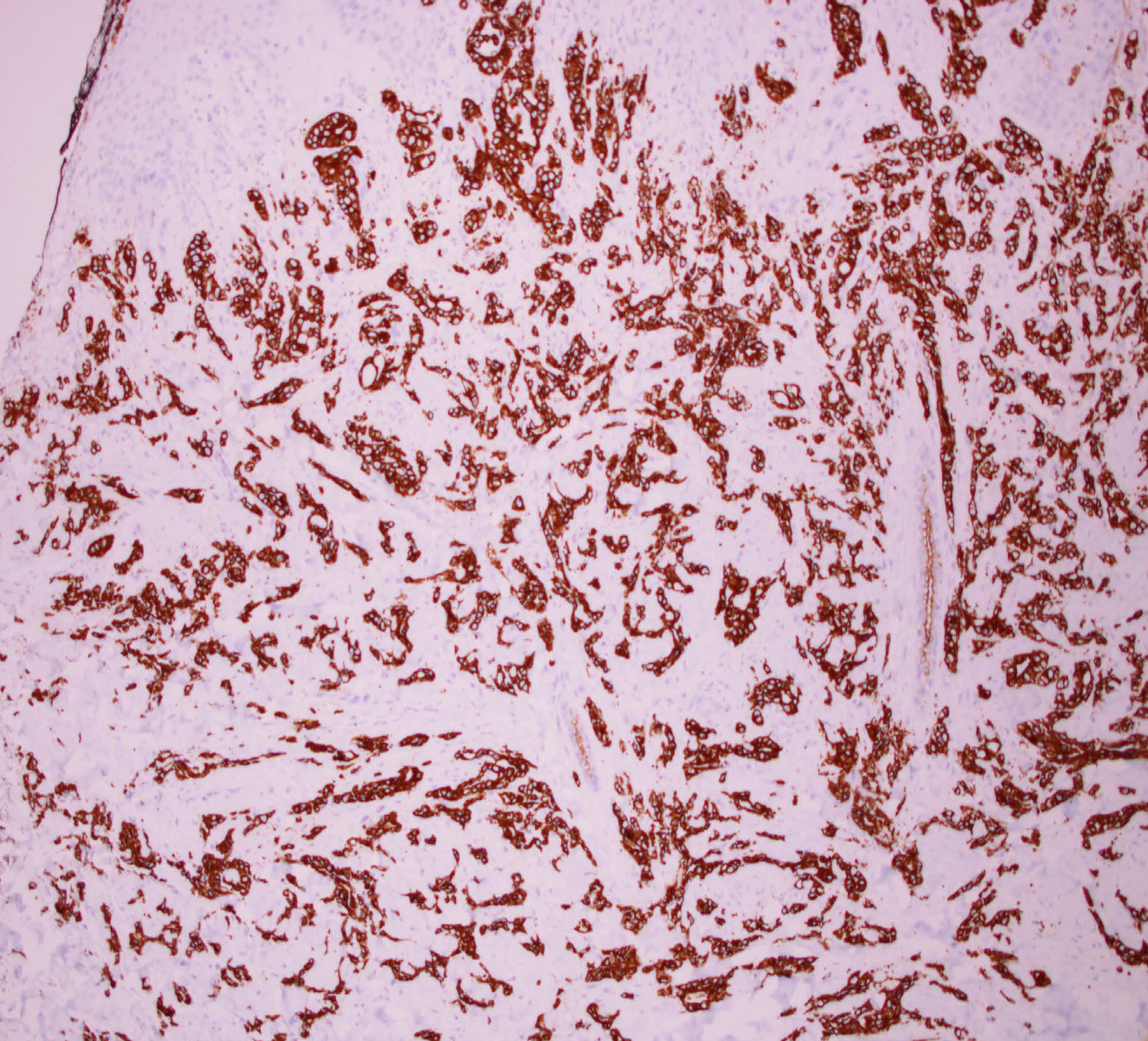
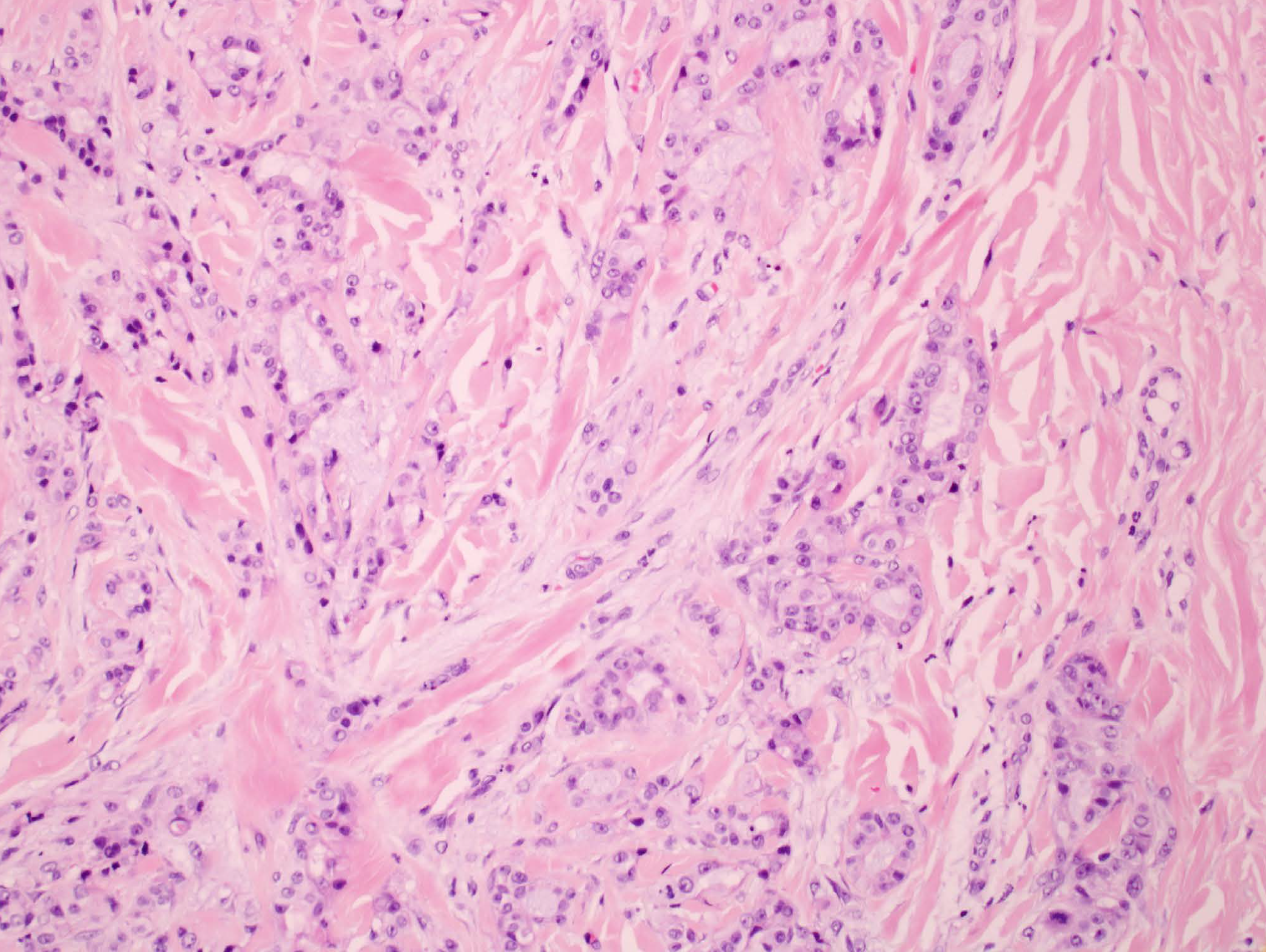
A 63-year-old man was referred to the Department of Dermatology with a one-month history of cutaneous ulceration on the plantar surface of his left foot. The patient’s medical history included long-standing diabetes mellitus, and a pancreatic ductal adenocarcinoma staged as T4N1M0 two years ago, initially treated with paclitaxel and gemcitabine. Disease progression in the form of liver metastases, resulted in a switch to a chemotherapy regimen of oxaliplatin, irinotecan, fluorouracil, and leucovorin (FOLFIRINOX). Several side-effects were attributed to this regimen including severe peripheral neuropathy. Physical examination revealed a painful, 2 cm round-to-oval, non-tender ulcer with undermined borders and central granulating tissue on the metatarsophalangeal area of the first toe [Figure 1]. Two smaller adjacent ulcers were also present. Despite oral antibiotic treatment, wound debridement, daily dressing changes and postural measures during four weeks, no improvement was observed. Furthermore, multiple subcutaneous nodules appeared on the trunk, arms and scalp during the following weeks, associated to severe asthenia [Figure 2]. A punch biopsy from the ulcer was performed. Histopathology disclosed a metastatic moderately differentiated adenocarcinoma involving the dermis and subcutaneous tissue [Figures 3a and b]. Immunohistochemistry analysis revealed intense positivity for CK7, CK19 and negativity for CK 20, features shared with the primary tumor [Figure 4]. Palliative care support was commenced, with a fatal outcome.

- Multiple ulcers and erosions with granulating tissue on the plantar surface of a metatarsophalangeal area of the first toe

- Multiple subcutaneous nodules on the back of the patient
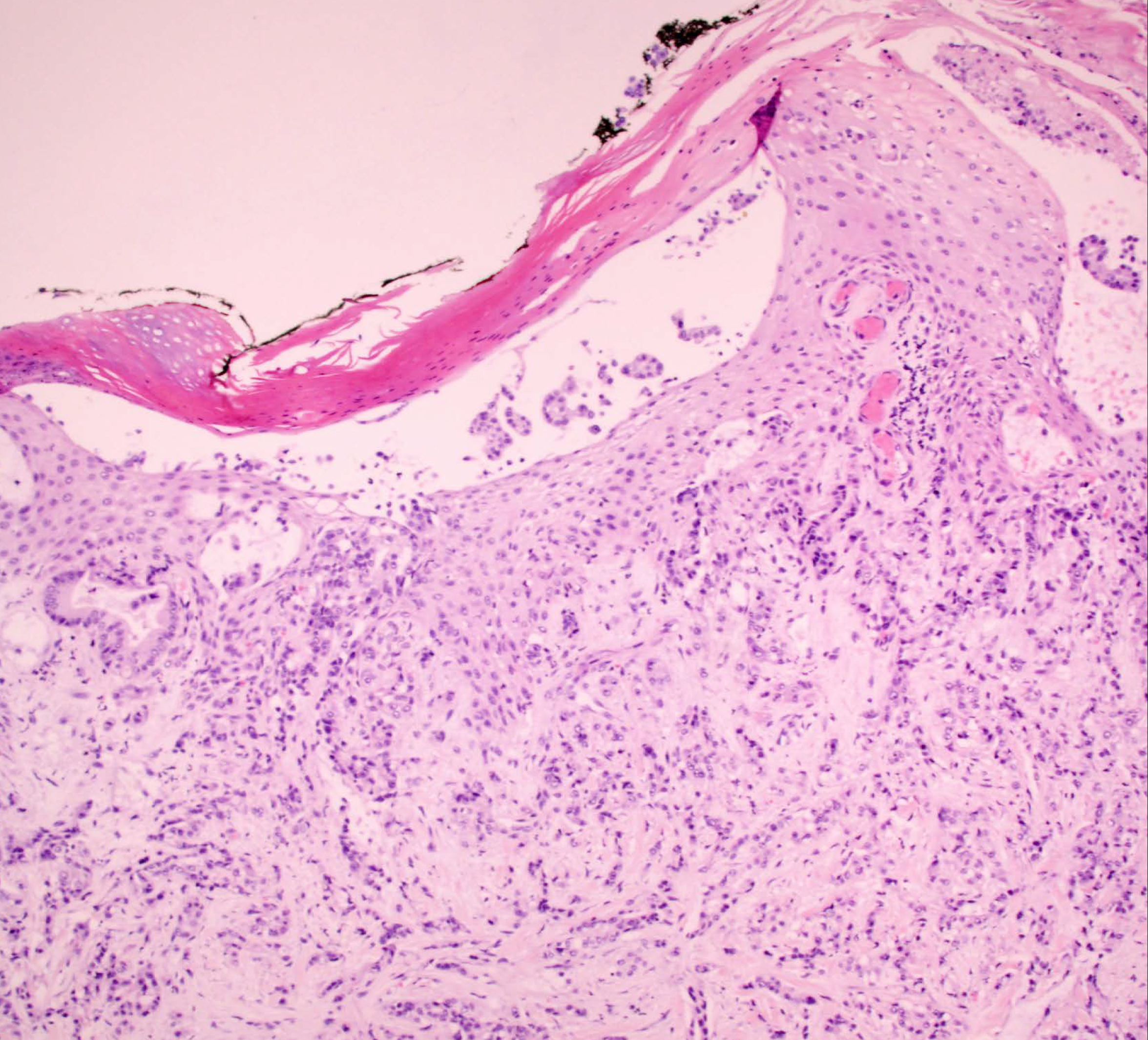
- Epidermal ulceration and diffuse infiltration of the dermis by tumour cells forming glands (Hematoxyline and eosin ×10)
- Detail of the dermal infiltration by tumour cells (Hematoxyline and eosin ×40)
- Immunohistochemistry staining results for CK7 show intensive positivity on neoplastic cells
Cutaneous metastases have been reported to occur in less than 10% of patients with solid organ malignancies.1 Their presence normally entails a poor prognosis. Breast and lung cancer seem to be the most frequent causes of skin infiltration by solid neoplasms, which is probably related to their frequency in the general population, and also due to other factors, including biological features that increase skin tropism.
Although pancreatic cancer is a relatively frequent neoplasm, cutaneous metastases from pancreatic cancer are considered to be extremely rare. In a recent study of 164 patients with skin metastasis, none of them had a pancreatic origin.2 Pancreatic ductal adenocarcinoma metastasises most commonly to the liver and peritoneum, followed by the lungs, bones and brain. The periumbilical region and the so-called “Sister Mary Joseph´s nodules,” are the most commonly reported cases of pancreatic skin metastases. However, a few cases of non-umbilical cutaneous metastasis have been described; with head and neck regions being the most frequently reported locations in a review of 26 cases.3 The most frequent clinical presentation includes nodules, followed by plaques, swelling or thickening of the skin and ulceration being very rare.4 Pancreatic cancer skin metastasis can occur anytime during the evolution of the disease and may be the first clinical manifestation in up to 50 percent of the cases.4 This observation is in accordance with the rapid capacity to metastasize and lethality attributed to pancreatic cancer.
This case illustrates the challenging diagnosis of pancreatic skin metastasis, which has presented as ulceration in the plantar region, in a setting of a patient with secondary peripheral neuropathy due to several chemotherapy cycles and long-standing diabetes mellitus. The diagnostic assumption of ulcers due to peripheral neuropathy when suggestive clinical history is found (poorly controlled diabetes, peripheral neuropathy and/or peripheral arterial disease) is daily-basis practice, but it is to be emphasised that many skin neoplasms can be misdiagnosed as chronic ulcers in predisposed patients, delaying diagnosis and treatment. Interestingly, melanoma, Kaposi’s sarcoma and squamous cell carcinoma are the main causes of malignant ulceration on the feet, but the differential diagnoses include many other tumours.5
We report the case of a patient with pancreatic skin metastasis mimicking a trophic ulcer. This case illustrates that, in the setting of internal malignancy, any skin lesion with a torpid course needs to be histologically studied.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Cutaneous metastases from different internal malignancies: A clinical and prognostic appraisal. J Eur Acad Dermatol Venereol. 2008;22:735-40.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous metastases from solid neoplasms in the 21st century: A retrospective study from a Portuguese tertiary care center. J Eur Acad Dermatol Venereol. 2020;34:1218-24.
- [CrossRef] [PubMed] [Google Scholar]
- Extensive cutaneous metastases of pancreatic adenocarcinoma: A case report and review of the literature. Clin Case Rep. 2017;5:51-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous metastasis from pancreatic cancer: A case report and systematic review of the literature. Oncol Lett. 2014;8:2654-60.
- [CrossRef] [PubMed] [Google Scholar]
- Misdiagnosis of diabetic foot ulcer in patients with undiagnosed skin malignancies. Int Wound J. 2022;19:871-87.
- [CrossRef] [PubMed] [Google Scholar]





