Translate this page into:
Cutaneous neonatal lupus erythematosus with unusual features
Correspondence Address:
Shankar Sawant
Department of Dermatology, TN Medical College and BYL Nair Charitable Hospital, Mumbai - 400008
India
| How to cite this article: Sawant S, Amladi S T, Wadhawa S L, Nayak C S, Nikam B P. Cutaneous neonatal lupus erythematosus with unusual features. Indian J Dermatol Venereol Leprol 2007;73:250-252 |
Abstract
A three month-old boy was brought by his mother with complaints of multiple reddish lesions on his trunk and face since birth. The patient had erythematous annular plaques with scaling on his extremities, palms and soles with periorbital erythema and edema giving the characteristic "eye mask" or "owl's eye" appearance. His mother did not have history of any illness. Hemogram, liver and renal function tests were within normal limits. A skin biopsy was suggestive of subacute cutaneous lupus erythematosus. Immunological work-up was positive for antinuclear antibodies (ANA) (1:40) with anti-Ro titers of 3.4 and 3.47 (>1.1 = clinically significant titre) in the mother and child respectively, although negative for anti-La antibodies. The child's electrocardiogram and 2D echocardiography were normal. We are presenting a case of anti-Ro-positive cutaneous lupus erythematosus with an uncommon skin manifestation.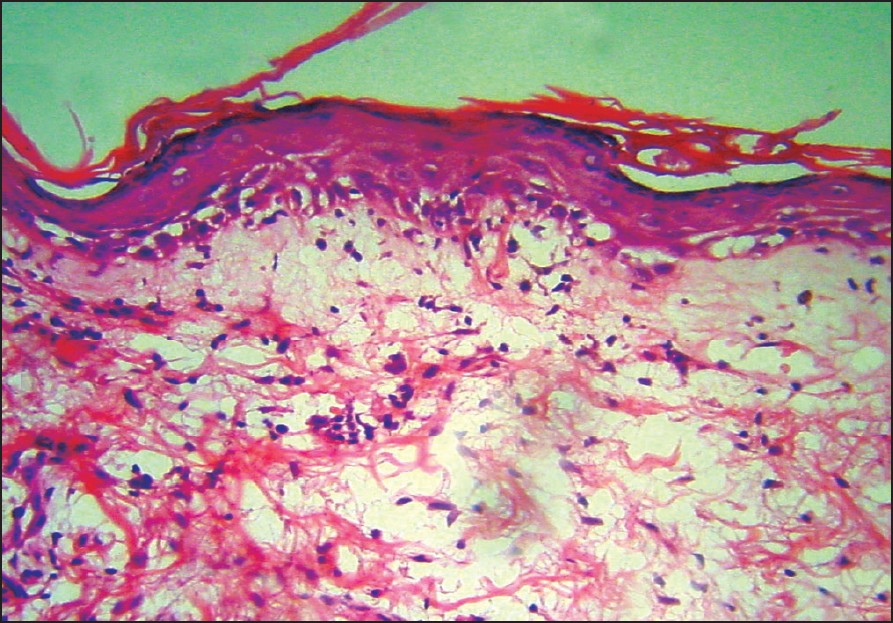 |
| Figure 3: Interface change with smudging of dermoepidermal junction (H and E, x200) |
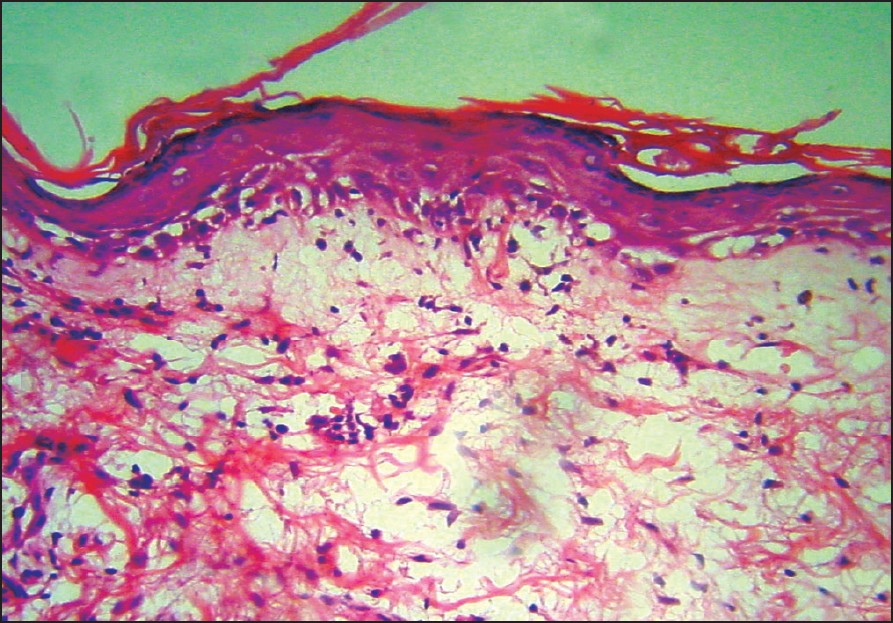 |
| Figure 3: Interface change with smudging of dermoepidermal junction (H and E, x200) |
 |
| Figure 2: Erythematous macules over soles |
 |
| Figure 2: Erythematous macules over soles |
 |
| Figure 1: Hypopigmented erythematous atrophic patches around eyes |
 |
| Figure 1: Hypopigmented erythematous atrophic patches around eyes |
Introduction
Neonatal lupus erythematosus (NLE) is an uncommon manifestation of lupus erythematosus that was first described in 1954. [1],[2] It is caused by transplacental transmission of maternal autoantibodies, typically of Ro / SS-specificity. Infants with NLE usually present with cutaneous lupus erythematosus and / or congenital heart block.
Case Report
A three month-old boy was brought by his mother with complaints of multiple reddish flat lesions on his back since birth. There was a single reddish lesion present on the back at the time of birth. Subsequently new lesions appeared on the face, scalp, trunk and extremities, while older lesions gradually faded in color and became depressed. There was no history of consanguinity, photosensitivity or fluid-filled or mucosal lesions. His birth history was normal and his birth weight was 2.5 kg. His parents and six year-old sister were asymptomatic.
On physical examination, there were multiple hypopigmented and erythematous atrophic patches of varying sizes ranging from 0.5-5 cm, around the eyes [Figure - 1], on the retroauricular area, abdomen and back with prominent telangiectasias mostly on the lesions on the back. Reticulate erythematous, dusky patches forming arcuate and annular lesions on the legs, arms and forearms were also noted. Palms and soles were involved with erythematous patches [Figure - 2]. Scarring and telangiectasias were more evident on the back. Spectacle-like erythema around the eyes was reminiscent of an "owl′s eye" or an "eye mask".
On investigations, his hemogram, liver and renal function tests were normal. Biopsy showed a thinned epidermis with a thickened basement membrane, interface dermatitis [Figure - 3], lymphohistiocytic infiltrate with smudging of the dermoepidermal junction [Figure - 3] and a few scattered necrotic keratinocytes with mucin deposition in the dermis suggestive of subacute cutaneous lupus erythematosus. Immunological work-up revealed both the mother and the child were ANA-positive at a titer of 1:40. Anti-Ro antibodies were present at a significant titer (Mother: 3.40 and child: 3.47, significant titer > 1.1). Anti-La antibodies were not present in the mother or the child. Child′s ECG and 2-D echocardiography revealed no abnormality.
Discussion
NLE is a rare disease. The characteristic periorbital erythema resulting in an "Owl′s eye" appearance is present in a majority of the cases and this cutaneous sign has been emphasized as a diagnostic clue to NLE. [3] However, the absence of the distinctive facial rash does not exclude the diagnosis of NLE. Other sites involved by the rash include the scalp, trunk, arms and legs. Female infants are more commonly affected [4] and this has been attributed to increased SS-A (Anti-Ro) expression by keratinocytes in response to estrogen. Incidence of NLE in subsequent pregnancies is 25%. [5] Although exposure to the sun precipitates skin lesions, lesions may be present on nonexposed areas like the groin.
Skin lesions may be present at birth but often develop within a few weeks after delivery. They begin as erythematous macules that enlarge into round, elliptical or annular plaques, often accompanied by fine overlying scale, which sometimes heal with hyperpigmentation or hypopigmentation. Telangiectasias may be prominent. [3] It has been believed that cutaneous lesions of NLE do not result in permanent scarring and other significant cutaneous sequelae. In one of the largest series to date, [3] Weston et al. followed up 18 NLE patients and noted that while four patients had residual hyperpigmentation, which did not persist beyond 22 months, two patients had residual hypopigmentation, which persisted beyond 4-5 years. Scarring and atrophy were not observed in any child.
Crowley and Frieden [6] reported an unusual case of NLE with erosions and atrophy with slight hypopigmentation as cutaneous sequelae after five years. In contrast to these reports, in 2003, Whitney et al. [6] reported a case of 12 year-old girl having persistent scarring and atrophy due to NLE. In our case, lesions were erythematous scaly patches initially and became hypopigmented and atrophic. Scarring and telangiectasias were more evident on the back. Reticulate, erythematous, dusky patches were present not only on the legs and hands but also on the palms and soles.
Recently, in August 2005, See et al. [7] described a case of NLE with an initial presentation of nodules and papules on the plantar surfaces of the feet, the histopathology of which was consistent with lupus erythematosus, while typical annular lesions appeared later. The affliction of both palms and soles has not been previously reported in any of the above series or cases. Alhough the mother did not have any features suggestive of lupus erythematosus, her ANA and Anti-Ro titers were positive, being almost equal to the ANA and Anti-Ro titers of the child, while the elder sister of the child was not affected at all. Biopsy of the atrophic patch showed changes suggestive of subacute cutaneous lupus erythematosus.
In 2003, Awasthy et al. reported a case of neonatal lupus erythematosus presenting with third degree congenital heart block as well as depigmented skin lesions affecting face and upper body. [8] In our case, no systemic involvement was seen. Thus, our case is unique in the appearance of typical lesions of NLE at classical sites with affection of both the palms and soles and the presence of scarring and atrophy at the time of presentation. However, long-term follow-up is needed to check for the final cutaneous sequelae.[9]
| 1. |
Rebecca YV, Marshall AG, John C. Atrophic plaques in neonates. Arch Dermatol 1992;128:681-6.
[Google Scholar]
|
| 2. |
McCuiston CH, Schoch EP Jr. Possible discoid lupus erythematosus in a newborn infant: Report of a case with subsequent development of acute systemic lupus erythematosus in mother. AMA Arch Derm Syphilol 1954;70:781-5.
[Google Scholar]
|
| 3. |
William LW, Joseph GM, Lela AL. The clinical spectrum of anti-Ro-positive cutaneous neonatal lupus erythematosus. J Am Acad Dermatol 1999;40:675-81.
[Google Scholar]
|
| 4. |
Miyagawa S, Dohi K, Yoshioka A, Shirai T. Female predominance of immune response to SSA/Ro antigens and risk of neonatal lupus erythematosus. Br J Dermatol 1990;123:233-7.
[Google Scholar]
|
| 5. |
Lee LA, Lillis PJ, Fritz KA, Huff JC, Norris DA, Weston WL. Neonatal Lupus Erythematosus in successive pregnancies. J Am Acad Dermatol 1983;9:401-6.
[Google Scholar]
|
| 6. |
Crowley E, Frieden IJ. Neonatal lupus erythematosus: An unusual congenital presentation with cutaneous atrophy, erosions, alopecia and pancytopenia. Pediatr Dermatol 1998;15:38-42.
[Google Scholar]
|
| 7. |
High WA, Costner MI. Persistent scarring, atrophy and dyspigmentation in a preteen girl with neonatal lupus erythematosus. J Am Acad Dermatol 2003;48:626-8.
[Google Scholar]
|
| 8. |
See A, Wargon O, Lim A, Suqo E, Le K. Neonatal lupus erythematosus presenting as papules on the feet. Australas J Dermatol 2005;46:172-6.
[Google Scholar]
|
| 9. |
Awathy N, Paul P, Mehta R. Neonatal lupus erythematosus. Indian Pediatr 2003;41:1048-50.
[Google Scholar]
|
Fulltext Views
2,626
PDF downloads
1,601





