Translate this page into:
Cutaneous plasmacytosis: A rare entity with unique presentation
2 Department of Dermatology and Venereology, Civil Hospital, Aizol, Mizoram, India
3 Clinical Reference Laboratory, SRL Ltd., Mumbai, Maharashtra, India
4 Department of Pediatric Dermatology, Institute of Child Health, Kolkata, West Bengal, India
Correspondence Address:
Subhra Dhar
Flat 9 C, Palazzo, 35, Panditia Road, Kolkata - 700 029, West Bengal
India
| How to cite this article: Dhar S, Liani L, Patole K, Dhar S. Cutaneous plasmacytosis: A rare entity with unique presentation. Indian J Dermatol Venereol Leprol 2017;83:673-676 |
Abstract
Primary cutaneous plasmacytosis is a rare cutaneous disorder with extensive cutaneous plaques/papules mainly on the trunk and face. Cases have mostly been documented from Japan. We present here a rare case of cutaneous plasmacytosis from India of Mongolian descent. This 50-year-old female from Mizoram had extensive maculo-papular violaceous plaques distributed on the face, axillae, trunk and lower extremities. Initial and repeat skin biopsy revealed dense perivascular and periadnexal mature plasma cells. She also had lymphadenopathy. Serum protein electrophoresis did not reveal any M band and the Bence Jones protein was negative in urine. The patient had multiple superficial lymph nodes and a biopsy from the cervical lymph node showed effacement of normal nodal architecture by sheets of plasma cells. Immuno histochemistry was done from both skin and lymph node biopsies. The kappa and lambda tight chains were not restricted; there by proving the polyclonal nature of the plasma cells. The novelty of the case lies in its classical clinical presentation with histopathological documentation.Introduction
Primary cutaneous plasmacytosis is a rare cutaneous disorder with extensive cutaneous plaques/papules mainly on the trunk and face. This entity is thought to be a reactive process of unknown etiology.[1] The skin lesions may be associated with variable extracutaneous involvement.[2] Cases have mostly been documented from Japan.[3]
We present here a very rare case of cutaneous plasmacytosis from India in a 53- year- old female of Mongolian descent.
Case Report
A 50-year-old female from Mizoram (north-eastern part of India) and of Mongolian ethnicity presented with multiple violaceous plaque lesions of variable size and shapes all over the body, predominantly over trunk, face and neck. Examination revealed reddish brown to purple colored plaques of sizes varying from 3-6 cm in diameter. The shapes were varied, viz., circular, elongated, annular, aciform coalescing at places forming reticulated patches [Figure - 1]. Lesions were found predominantly over the trunk, face and neck [Figure - 2], axillae and back. No hepato splenomegaly was found. Patient was found to be anaemic. A skin biopsy was performed and initial blood tests were ordered. Her Hemoglobin was found to be 7.3 gm/dl and the ESR was 150/hr. Blood for HIV antibodies (1 and 2) were negative and VDRL was non reactive. The histopathology examination of the skin biopsy revealed the following: The epidermis was unremarkable. The dermis shows moderately dense aggregates of plasma cells in the superficial and deep perivascular areas [Figure - 3]. These were admixed with variable number of lymphocytes and histiocytes [Figure - 4].
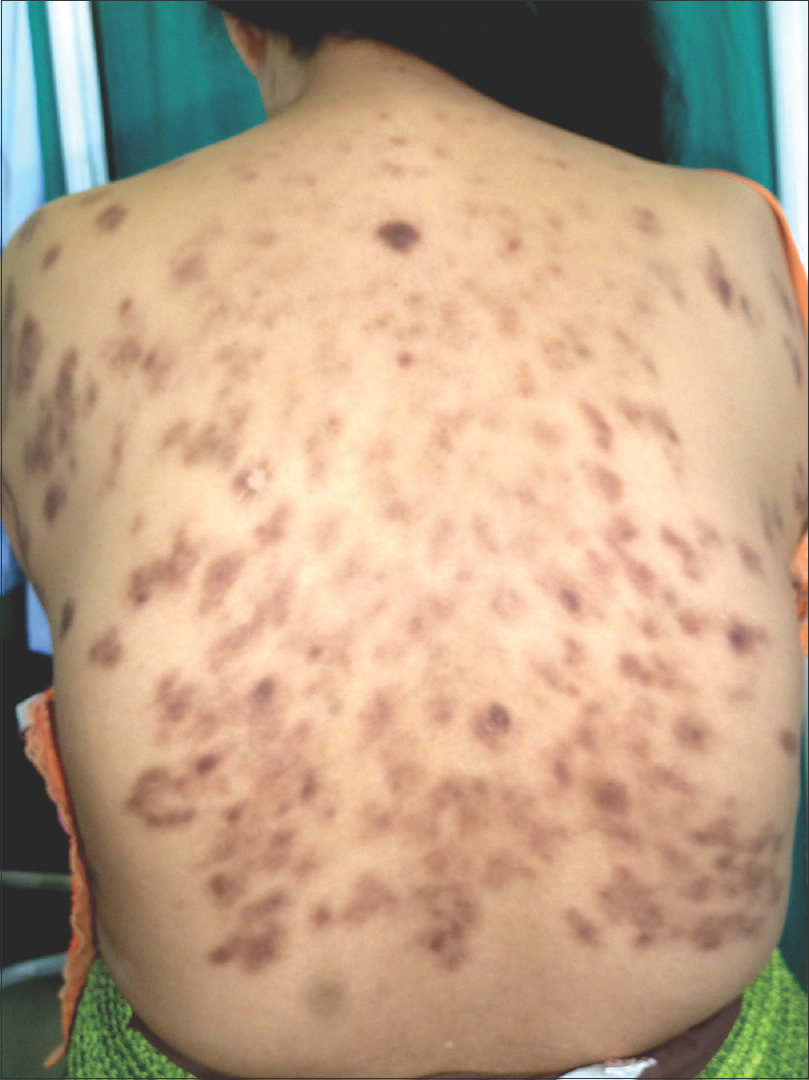 |
| Figure 1: Multiple violaceous coloured plaques of variable sizes and shapes over back |
 |
| Figure 2: Violaceous plaques over face and neck in the same lady |
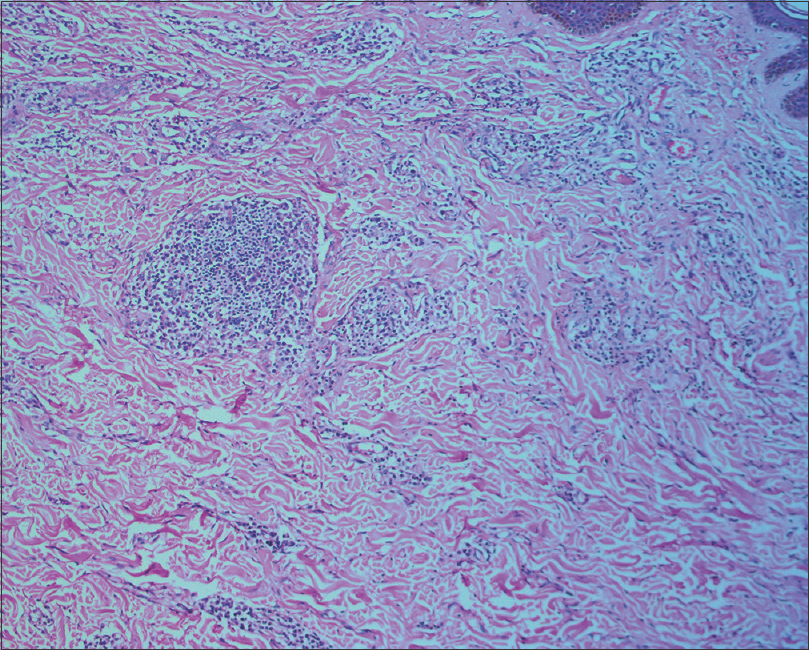 |
| Figure 3: Lymphoplasmacytic infiltrate in the dermis (H and E, ×100) |
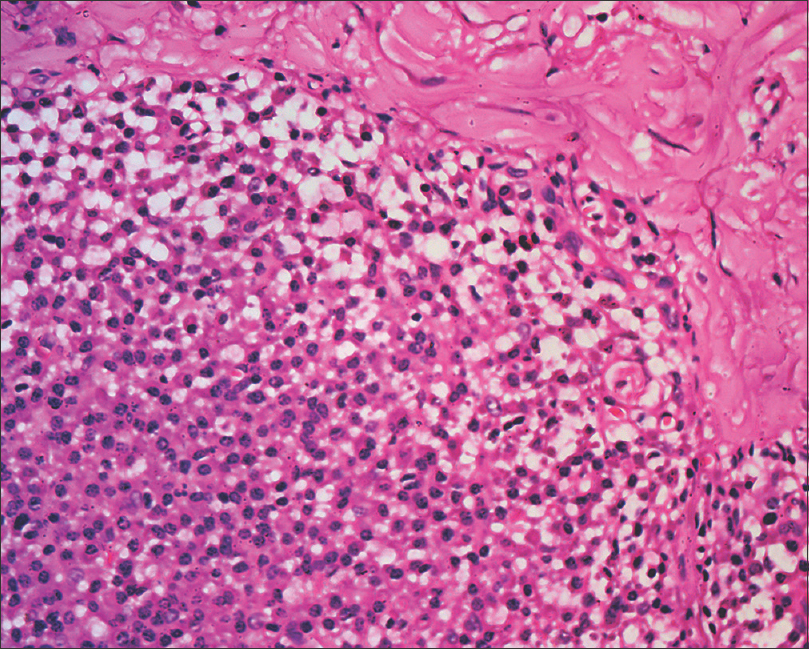 |
| Figure 4: Abundant plasma cells and lymphocytes in dermal infiltrate (H and E, ×400) |
A peripheral smear examined revealed extensive rouleaux formation. Other biochemical parameters were as follows - BUN: 26.8 mg/dl, Creatinine 3.4 mg/dl, total protein was 12.6 g/dl, albumin was 2.6 gm/dl, globulin was 10g/dl, total urinary protein was 15931 mg/dl, LDH was 361 U/L. Serum total IgG was 41 g/dl.
Serum protein electrophoresis did not reveal any M band and the Bence Jones protein was negative in urine.
The patient also had multiple superficial lymph nodes in the cervical, axillary and inguinal region. Biopsy from the cervical lymph node showed effacement of normal nodal architecture by sheets of plasma cells [Figure - 5].
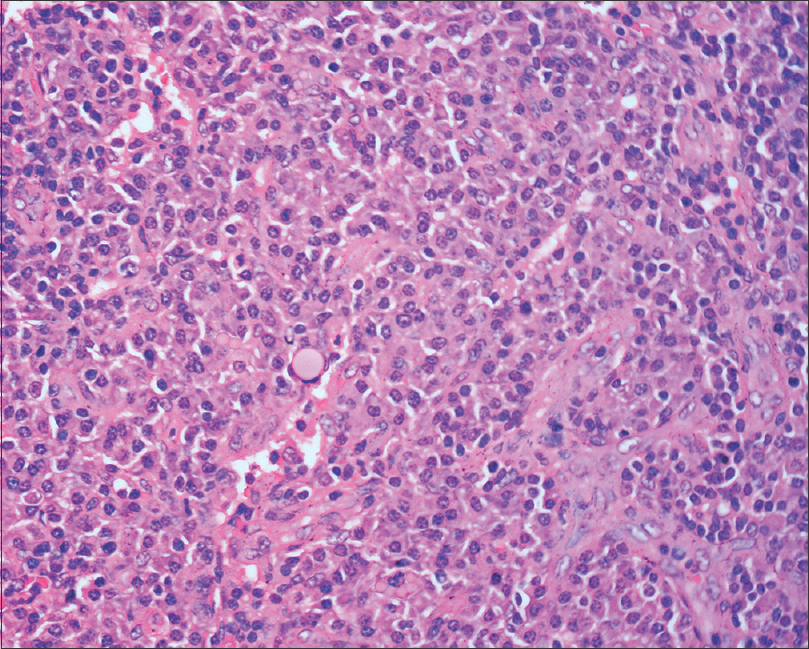 |
| Figure 5: Sheets of plasma cells in lymph node (H and E, ×400) |
Immunohistochemistry was done for kappa and lambda light chains to rule out monoclonality of plasma cells from the lymph node biopsy. The kappa and lambda tight chains were not restricted, there by proving the polyclonal nature of the plasma cells [Figure - 6].
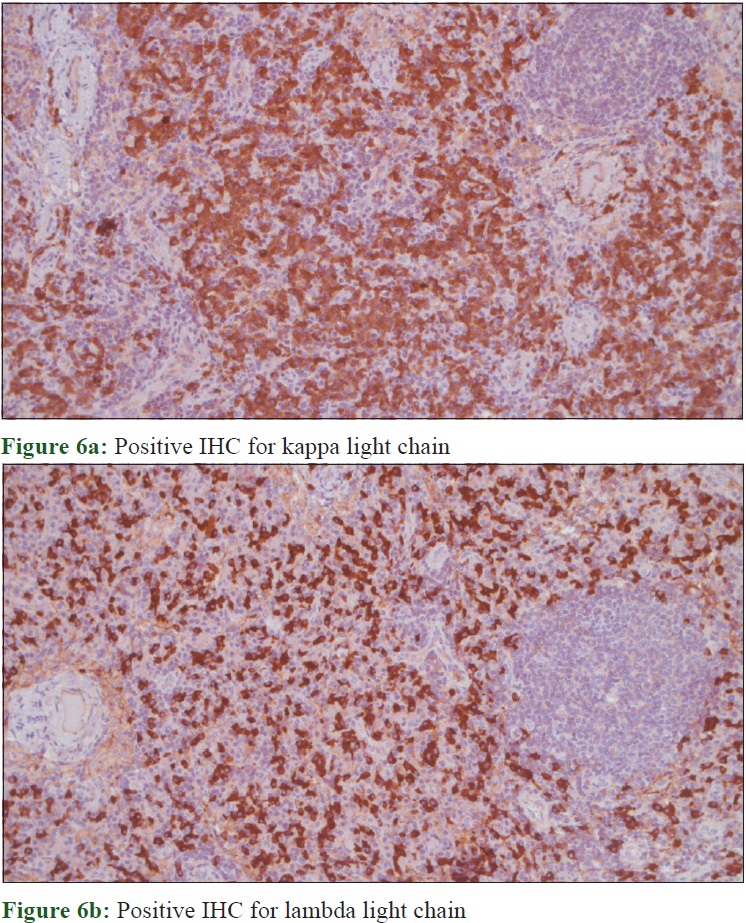 |
| Figure 6 |
Discussion
Cutaneous and systemic plasmacytosis is a rare reactive lympho-plasmacytic disorder. It was first described in Asia by Yashiro in 1976 who described it as a type of plasmacytosis. Kitamura further characterised it in 1980. Since then it has been described in Asian patients, specially amongst the Japanese.[4] As most patients of cutaneous plasmacytosis are found to have some form of systemic symptoms,[5] some authors prefer the term “cutaneous and systemic plasmacytosis” to account for the extracutaneous involvement.[6]
The cutaneous plasma cell infiltrate are polyclonal and the most common extracutaneous involvement is lymphadenopathy.
Clinical manifestations include fever, anaemia and hypergammaglobulinaema. The cutaneous presentation is very characteristic comprising of multiple reddish-brown infiltrated macules, plaques and nodules, chiefly on the trunk.[2]
The etiopathogenesis is poorly understood. Dysregulated production of IL-6 which is a cytokine that induces B - cell proliferation and differentiation to plasma cells which in turn causes immunoglobulin secretion and angiogenesis is thought to play a role. Genetic polymorphism in the IL-6 gene may possibly explain the propensity of the disease to manifest in particular geographic regions.[7],[8]
Recently a similar case of primary cutaneous plasmacytosis has been reported from India.[9] We are not aware of any such case where Hidradenitis Suppurativa has been a manifestation of primary cutaneous plasmacytosis as reported in the case. This is to our mind, certainly an unusual manifestation.
Histologic features include a moderately dense infiltrate of mature plasma cells in perivascular areas of both superficial and deep dermis. Admixture of lymphocytes may be present and lymphoid follicles with reactive germinal centres can also be seen.
Light chain restriction is absent which goes with the polyclonal nature of the plasma cell infiltrate.[10]
Approximately 58% of cases of cutaneous plasmacytosis have associated lymphadenopathy which forms the commonest extracutaneous manifestation. Liver, spleen, lungs and kidney are less frequently affected organs.[1],[11] Our patient had no history of recurrent infections, chronic inflammatory disease or neoplasm and tested negative for autoimmune markers. Although creatinine was raised in our patient, the kidneys could not be assessed as the patient refused kidney biopsy.
Most cases of plasmacytosis run a benign indolent course without spontaneous remissions. There are reports of plasmacytosis developing malignant lymphoma. However the rate of transformation to malignant neoplasm is quite low in Asian literature.[2]
Cases are recalcitrant to treatment. Treatment modalities like topical and systemic steroid, antibiotics and systemic chemotherapy have shown to have some beneficial effects. Topical 0.1% tacrolimus, thalidomide, photodynamic therapy, combining corticosteoid with cyclophosphamide, topical PUVA, radiotherapy have been tried with variable outcome.[12]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Chantachaeng W, Chularojanamontri L. Cutaneous plasmacytosis: A case report and review of pulmonary findings. Dermatol Reports 2011;3:e39.
[Google Scholar]
|
| 2. |
Lee TG, Jeong WS, Moon SH, Hwangbo H, Lee SK, Lee DR, et al. Cutaneous and systemic plasmacytosis associated with renal amyloidosis. Ann Dermatol 2015;27:759-62.
[Google Scholar]
|
| 3. |
Uhara H, Saida T, Ikegawa S, Yamazaki Y, Mikoshiba H, Nijoh S, et al. Primary cutaneous plasmacytosis: Report of three cases and review of the literature. Dermatology 1994;189:251-5.
[Google Scholar]
|
| 4. |
Hjira N, Baba N, Boudhas A, Al Bouzidi A, Boui M. Cutaneous plasmacytosis: Report of a Moroccan case. J Dermatol Dermatolog Surg 2014;18:27-30.
[Google Scholar]
|
| 5. |
Tada Y, Komine M, Suzuki S, Kikuchi K, Sasaki M, Kaneko N, et al. Plasmacytosis: Systemic or cutaneous, are they distinct? Acta Derm Venereol 2000;80:233-5.
[Google Scholar]
|
| 6. |
Honda R, Cerroni L, Tanikawa A, Ebihara T, Amagai M, Ishiko A. Cutaneous plasmacytosis: Report of 6 cases with or without systemic involvement. J Am Acad Dermatol 2013;68:978-85.
[Google Scholar]
|
| 7. |
Kodama A, Tani M, Hori K, Tozuka T, Matsui T, Ito M, et al. Systemic and cutaneous plasmacytosis with multiple skin lesions and polyclonal hypergammaglobulinaemia: Significant serum interleukin-6 levels. Br J Dermatol 1992;127:49-53.
[Google Scholar]
|
| 8. |
Fang S, Shan K, Chen AJ. Cutaneous and systemic plasmacytosis on the face: Effective treatment of a case using thalidomide. Oncol Lett 2016;11:1923-5.
[Google Scholar]
|
| 9. |
Goyal T, Varshney A, Zawar V, Sharma V. Primary cutaneous plasmacytosis: Masquerading as hidradenitis suppurativa. Indian J Dermatol 2016;61:213-5.
[Google Scholar]
|
| 10. |
Amin HM, McLaughlin P, Rutherford CJ, Abruzzo LV, Jones D. Cutaneous and systemic plasmacytosis in a patient of Asian descent living in the United States. Am J Dermatopathol 2002;24:241-5.
[Google Scholar]
|
| 11. |
Yang YW, Hu S, Kuo TT, Hong HS. Cutaneous plasmacytosis-Report of a case. Dermatol Sin 2003;21:97-101.
[Google Scholar]
|
| 12. |
Wong KF, Chan JK, Li LP, Yau TK, Lee AW. Primary cutaneous plasmacytoma – Report of two cases and review of the literature. Am J Dermatopathol 1994;16:392-7.
[Google Scholar]
|
Fulltext Views
6,380
PDF downloads
1,575





