Translate this page into:
Cutaneous rhinosporidiosis
2 Department of Otorhinolaryngology, K. S. Hegde Medical Academy, Deralakate, Mangalore, India
Correspondence Address:
Manjunath M Shenoy
Department of Skin and VD, K. S. Hegde Medical Academy, Deralakate, Mangalore - 574160
India
| How to cite this article: Shenoy MM, Girisha B S, Bhandari SK, Peter R. Cutaneous rhinosporidiosis. Indian J Dermatol Venereol Leprol 2007;73:179-181 |
Abstract
Rhinosporidiosis is a chronic granulomatous disease of the mucocutaneous tissue, which clinically presents as polypoidal growths. Cutaneous lesions are infrequent and are generally associated with mucosal lesions. We present a case of cutaneous rhinosporidiosis in association with recurrent nasopharyngeal rhinosporidiosis in a 65-year-old male patient. He presented with dysphagia for solid foods and skin growth on the left side of jaw of 2 years duration. Histopathology of cutaneous and nasopharyngeal lesions revealed numerous thick walled sporangia in a vascular connective tissue along with a granulomatous inflammation confirming the diagnosis of cutaneous and nasopharyngeal rhinosporidiosis. Endoscopic removal of nasopharyngeal polyp was done and he was started on dapsone therapy.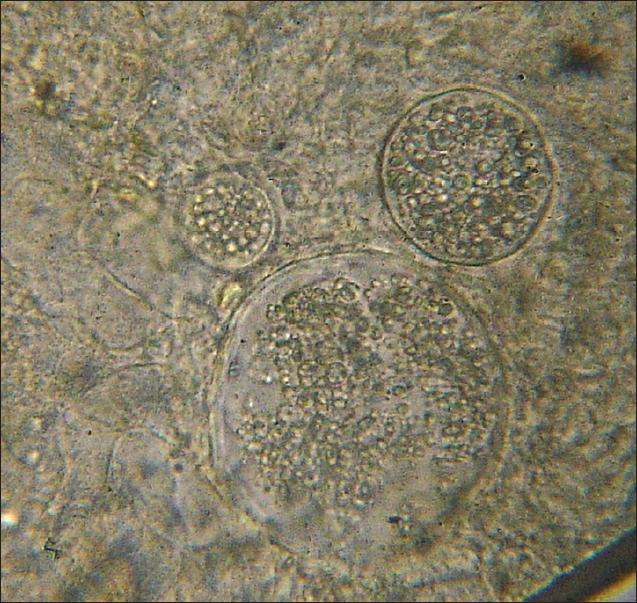 |
| Figure 3: KOH mount showing spherules and endospores |
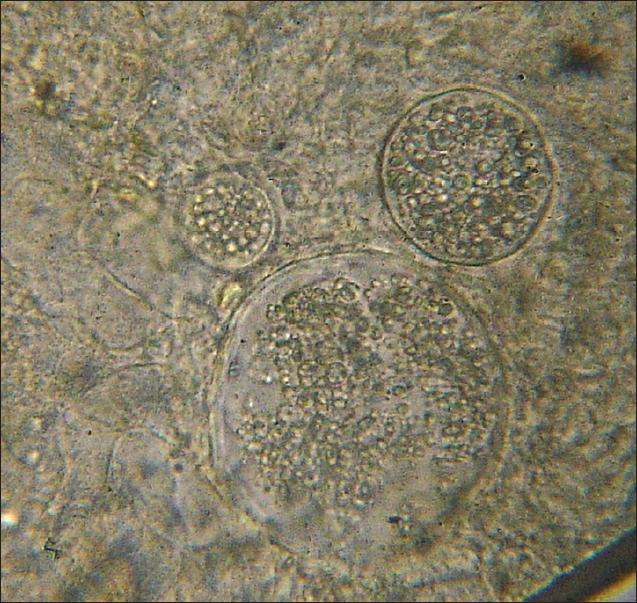 |
| Figure 3: KOH mount showing spherules and endospores |
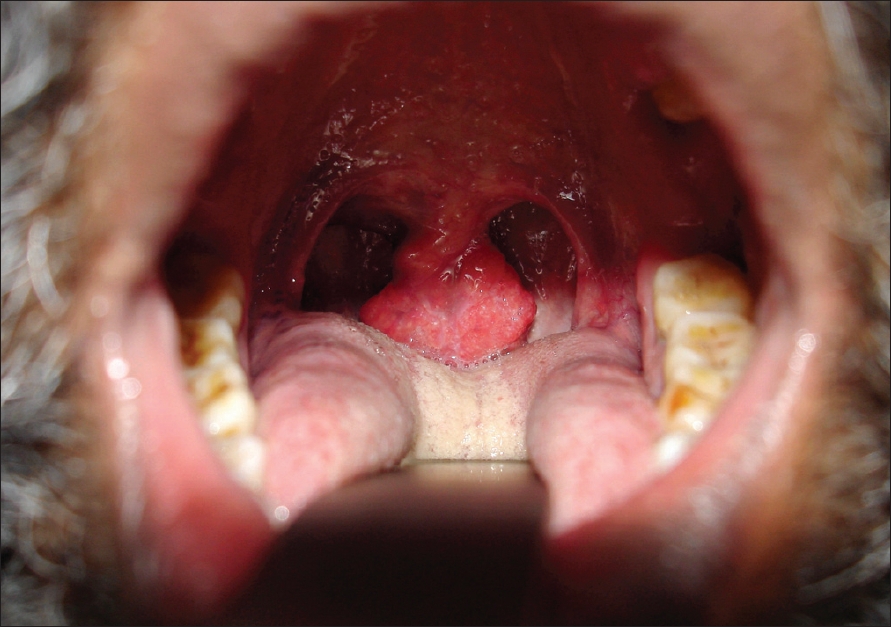 |
| Figure 2: Pedunculated nodule on uvula |
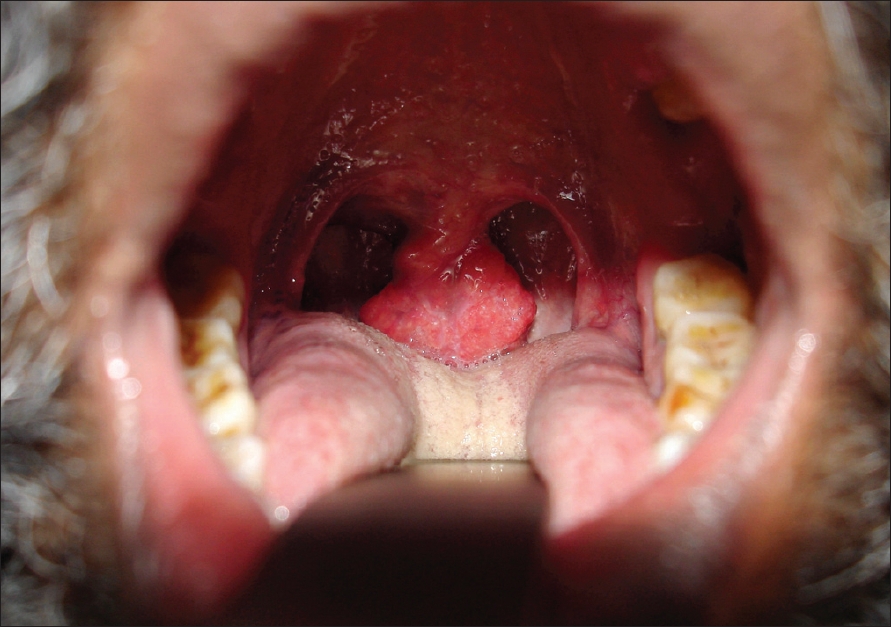 |
| Figure 2: Pedunculated nodule on uvula |
 |
| Figure 1: Cutaneous lesion on the angle of jaw and neck |
 |
| Figure 1: Cutaneous lesion on the angle of jaw and neck |
Introduction
Rhinosporidiosis is a chronic granulomatous infection caused by Rhinosporidium seeberi. Infection is usually caused by contact with stagnant fresh water such as swimming pools. The disease, while being of special interest to oto-rhino-laryngologists, is of interest to dermatologists and ophthalmologists as well because of the cutaneous, subcutaneous and ocular lesions. Mucosal involvement of nose, nasopharynx and soft palate in the form of sessile or pedunculated vascular polyps is the commonest presentation. Cutaneous lesions without mucosal involvement are extremely rare and they present as asymptomatic friable warty growths. We present a case of cutaneous rhinosporidiosis along with nasopharyngeal rhinosporidiosis.
Case Report
A 65-year-old manual laborer from the state of Kerala, India presented with history of a growth on the left side of jaw. It started as a small nodular lesion, which gradually increased in size. There was history of ulceration but no bleeding or discharge of pus. He also complained of dysphagia and hyponasality of voice. Six years ago, he had undergone a surgical excision of nasal polyps diagnosed as rhinosporidiosis in a private hospital.
On examination, there was a single tender, ulcerated, verrucous plaque measuring 5x4cm situated on the left angle of jaw [Figure - 1]. Left cervical lymph nodes were enlarged, firm, mobile and non-tender. FNAC report from an enlarged lymph node done in another hospital revealed reactive lymphadenitis. Examination of the oral cavity revealed a pedunculated polypoidal mass studded with small white dots on the surface hanging from the uvula [Figure - 2]. Diagnosis of cutaneous and nasopharyngeal rhinosporidiosis was considered. However, lupus vulgaris and subcutaneous mycoses were also considered in the differential diagnosis of cutaneous lesion.
His blood counts, ESR, blood sugar, liver and renal function tests, chest X-ray and abdominal ultrasonography were within normal limits. Serology for HIV was negative. Excised macerated tissue from the skin lesion was mounted in 10% KOH which revealed spherules and large numbers of endospores [Figure - 3] on microscopy. Wedge biopsy was done from the cutaneous lesion and endoscopic removal with cauterization of base was done for the nasopharyngeal masses. The tissues were sent for histopathological examination. Cutaneous and nasopharyngeal lesions microscopically revealed numerous thick walled sporangia in a vascular connective tissue along with a granulomatous inflammation. It confirmed the diagnosis of cutaneous and nasopharyngeal rhinosporidiosis. Endoscopic removal of nasopharyngeal polyp was done and he was started on dapsone therapy (100 mg/day). He was also advised regular follow up to assess response to dapsone.
Discussion
Rhinosporidiosis is known for over a hundred years and was first described in Argentina. [1] The etiologic agent, Rhinosporidium seeberi, is closely related to several fish pathogens. It is an aquatic protozoan and was previously considered to be a fungus, however its taxonomic position is unclear. [2] The infection commonly affects nasal mucous membranes and ocular conjunctivae of humans and animals, producing slowly growing masses that degenerate into pink to purple and friable polyps. Four forms of the disease are recognized viz. nasal, ocular, cutaneous and disseminated (rare). Infection of the nose and nasopharynx is observed in 70% of patients of rhinosporidiosis; infection of the palpebral conjunctivae or associated structures (including the lacrimal apparatus) is observed in 15%. Cutaneous lesions are infrequent and are generally associated with mucosal lesions. [3] A case of disseminated cutaneous rhinosporidiosis in an HIV sero-positive patient has been described. [4]
Rhinosporidiosis has been reported from several countries but is most commonly reported from India and Sri Lanka. Apart from the human, this aquatic microorganism can also cause disease among the farm, domestic and wild animals. Inoculation of injured epithelia from the natural habitat seems to be the mode of transmission. Some individuals are more prone to develop this infection than others due to some unknown host factors. [1]
Several modes of spread have been postulated for cutaneous rhinosporidiosis. Surrounding cutaneous surfaces may be involved due to a contiguous spread from nasal mucosa. Hematogenous dissemination can lead to generalized cutaneous lesions. Direct inoculation of the organism results in primary cutaneous type. [2] Apart from these a possibility of lymphatic spread has also been considered. [1]
Spontaneous regression of lesions can rarely occur, however it should be treated early in order to prevent extension of lesions or dissemination. It is difficult to determine the drug sensitivity since growing the organisms in vitro or in vivo has been a failure. [1] Diathermy excision is the treatment of choice, but in spite of this recurrences have occurred. [5] Several drugs have been tried but dapsone alone is proven to be somewhat effective. Its probable mode of action is to arrest the maturation of the sporangia and inducing stromal fibrosis.
Our patient had cutaneous rhinosporidiosis in association with recurrent nasopharyngeal lesions. He had dysphagia due to the hanging uvular lesion and change in the quality of voice (hypo nasality) probably due to fibrosis resulting from recurrent nasal and nasopharyngeal lesions. Development of cutaneous lesion may be an early sign of dissemination; however our thorough search for involvement of other cutaneous sites and systems did not reveal any other lesions.
The case highlights rare occurrence of cutaneous rhinosporidiasis, the possibility of which should be kept in mind particularly when polypoidal growths in nasal cavity are associated with cutaneous lesions.
| 1. |
Arseculeratne SN. Recent advances in rhinosporidiosis and Rhinosporidium seeberi . Indian J Med Microbiol 2002;20:119-31.
[Google Scholar]
|
| 2. |
Kumari R, Laxmisha C, Thappa DM. Disseminated cutaneous rhinosporidiosis. Dermatology Online Journal 11 (1). [Last updated on 2005 Mar 5]. [Last accessed on 2006 Apr 9].
[Google Scholar]
|
| 3. |
Rivard R, Hospenthal DR. Rhinosporidiosis. Last updated on 2006 Jun 29. Available from: www.emedicine.com/med/topic2029.htm, Last accessed on 2006 Apr 9.
[Google Scholar]
|
| 4. |
Padmavathy L, Lakshmana L, Selvam Siva S, Sahoo CG. Disseminated cutaneous rhinosporidiosis in a HIV sero - positive patient. Indian J Dermatol Venereol Leprol 2001;67:332-3.
[Google Scholar]
|
| 5. |
Shah AK, Ingle MV. Tracheal rhinosporidiosis: A case report. J Postgrad Med 1985;31:210-1.
[Google Scholar]
|
Fulltext Views
5,297
PDF downloads
1,429





