Translate this page into:
Dermatological adverse effects of hair dye use: A narrative review
Corresponding author: Dr. Kaliaperumal Karthikeyan, Department of Dermatology, Venereology and Leprosy, Sri Manakula Vinayagar Medical College and Hospital, Madagadipet, Puducherry, India. karthikderm@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Palaniappan V, Karthikeyan K, Anusuya S. Dermatological adverse effects of hair dye use: A narrative review. Indian J Dermatol Venereol Leprol. 2024;90:458-70. doi: 10.25259/IJDVL_745_2022
Abstract
Hair dyeing is a popular practice dating back to ancient Egyptian times. Initially, hair dye use was restricted to concealing grey and white hairs of the elderly population. However, in recent times, its use is common among the younger generation as a fashion statement.
Hair dye contact dermatitis is a common dermatological condition encountered by dermatologists. It is a delayed type of hypersensitivity reaction that commonly affects the scalp and the vicinity of hair line and neck. Para-phenylenediamine (PPD), a synthetic aromatic amine is the most common allergen specifically implicated in hair dye contact dermatitis. Para-phenylenediamine was announced as the allergen of the year in 2006 by the American Contact Dermatitis Society. Contact allergy to para-phenylenediamine can occur in 0.1–2.3% of the general population. Epicutaneous patch testing is the gold standard test for the diagnosis of hair dye contact dermatitis. However, para-phenylenediamine carries a risk of cross-sensitivity and co-sensitization to other allergens.
Apart from contact dermatitis, hair dye use is also associated with various other cutaneous adverse effects such as pigmentary changes, hair loss, skin malignancies and autoimmune disorders. Due to the various adverse effects associated with hair dye use, it is prudent to look for safer alternatives to allergenic hair dyes. In this article, we review the epidemiology, cutaneous and systemic adverse effects associated with hair dye use, patch testing, preventive strategies to minimize the risk of hair dye contact dermatitis, and treatment aspects.
Keywords
Contact dermatitis
cosmetics
hair dye allergy
hair dye dermatitis
occupational dermatitis
Introduction
Hair colour is often linked to attractiveness and dark hair is a sign of youthfulness in most cultures. It is thus not a surprise that hair dyeing has become a multibillion-dollar industry involved in the production of various synthetic and natural dyes. In 2020, the global hair dye and colour industry was valued around 21.4 billion U.S. dollars and projected to be around 36.2 billion U.S. dollars by 2025.1 However, the use of hair dyes is a major source of chemical exposure among the general population and can cause various adverse effects. In this article, we provide an overview of hair dyes and the potential adverse effects associated with their use.
History of hair colouring
The art of hair dyeing has been known since ancient Egyptian times when Ramesses II, pharaoh of the nineteenth dynasty of Egypt, had his hair applied with henna after death.2 In ancient Greece, potassium solution rinse was used to bleach hair and then rubbed with a type of ointment composed of pollen and flower petals.3 Colouring of hair in different shades such as black, green, red, gold were practiced in the past.4 The first artificial hair dye was synthesized in a laboratory in 1856.5 Para-phenylenediamine was initially described by German chemist Hofmann in 1863 and formulated for use in hair dye in the late 19th century.6 Boonnevie recognized the implications of para-phenylenediamine exposure and recommended including it into the first standard series of patch test series allergen screening panel in 1939.7
Classification and composition of hair dyes
Hair dyes are classified into three categories based on their chemical composition, namely, synthetic dyes, vegetable or herbal dyes and metallic dyes. Based on their oxidative nature, they are divided into oxidative dyes and non-oxidative dyes. According to the ability of hair dyes to penetrate the hair shaft, they can be divided into temporary, semi-permanent, demi-permanent and permanent hair dyes [Figure 1]3. The classification and features of various types of hair dyes are summarised in Table 1.4,7,8 The various ingredients of hair dyes along with their functions are mentioned in Table 2.3 The steps involved in different types of hair dyeing processes are depicted in Figure 23. Bleaching is a process that aids in achieving different shades of hair.8 The mechanism of hair damage secondary to bleaching is shown in Figure 33. The process of hair colouring is shown in Figure 4.3 Aromatic compounds derived from benzene substituted by at least two electron donor groups such as NH
2
and OH in
ortho or
para positions for easy oxidation and colour development p-phenylenediamine p-aminophenol Aromatic derivatives of benzene substituted by at least two electron donor groups such as NH
2
and OH in
meta positions which does not present easy oxidation by H
2
O
2
Modifies colours with primary intermediaries and oxidants Determines the final shade of colour Phenols Meta disubstituted phenylenediamines and phenyleneaminophenols Resorcinol (1,3-dihydroxybenzene) derivatives Promotes proper pH value to initiate oxidation reaction Removes the natural pigments present in hair Ammonia (as ammonium hydroxide) Monoethanolamine (for liquid forms) Sodium silicate (for solid forms) Two types of oxidizing agents used Peroxides are unstable, require the stabilizers like sodium stannate and pentasodium pentetate Used in the form of emulsion – creamy hydrogen peroxide Hydrogen peroxide (when vehicle is water) Sodium persulphate (when vehicle is powder) Added to oxidative hair dye formulations to delay the reaction between bases and reaction modifiers To prevent the initiation of the reaction in the packaging tube during storage Sodium metabisulphite Imparts colour to the hair dye Responsible for allergenic reactions in many cases O-nitro anilines Aminonitrophenols and their ethers Azo dyes Nitrophenylamines Nitrophenienediamines Anthroquinone Avoid reaction before the addition of oxidant Water-soluble antioxidant – prevents manipulation of bases and initiation of oxidation reaction by reaction modifiers Oil-based antioxidant – used as a vehicle for emulsion hair dyes as it avoids yellowing of wax Erythorbic acid – water based antioxidant T-butyl quinone Emulsion form of oxidative dyes are the highest selling hair dye product in the market Emulsion Gel Powder Solution (liquid) To thicken the hair dye product solution for better handling, to get homogenous dye results, Increase in concentration of surfactant increases the dye-formation in dye solution To disperse dye molecules Aids in the wetting of hair Sodium lauryl sulphate Sodium laureth sulphate Disodium laureth sulfosuccinate Disodium lauryl sulfosuccinate Capramidopropylbetaine Sodium lauroyl methyl isethionate Cocamidopropyl betaine Capryl/capamidopropyl betaine Sodium cocoamphoacetate Increases the dyeing rate, establishment of equilibrium and hair wetting Dispersion of dye molecules Aids in the wetting of hair Quaternium-80 Benzyl alcohol Glycols The ingredient which holds all other ingredients together Oleth-23 Cetearyl Alcohol Protection of hair against photodamage Homoxalate Octinosate Octocrylene Oxybenzone Protects the product from oxidation Protects against the contaminants such as moulds or bacteria Parabens Phenoxyethanol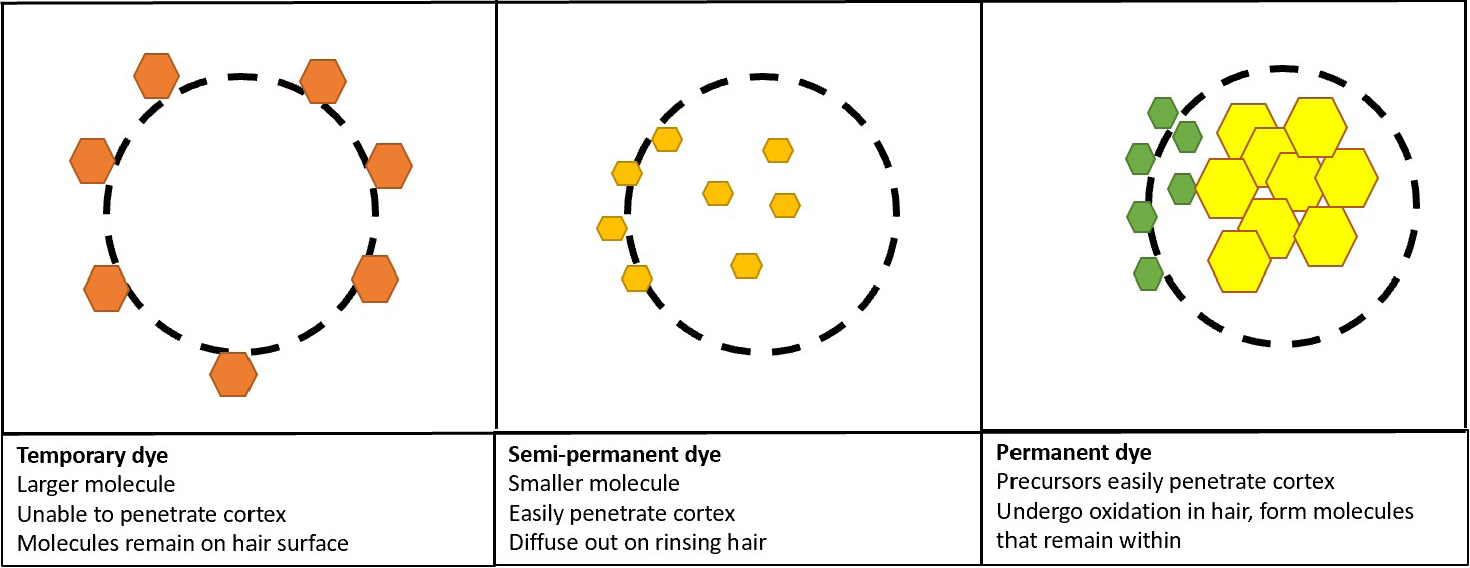
Penetration of hair dye in the hair shaft.
Synthetic hair dyes
Characteristics
Non-oxidative
Oxidative
Temporary
Semi-permanent
Permanent
Molecular weight
High
Low
Low
Nature
Anionic
Cationic
Cationic
Hydrogen peroxide
Absent
Present in lower concentration
Present in higher concentration
Hair penetration
On surface
Diffuse cortex
Diffuse cortex
Contact time
30 mins
10–40 mins
30–45 mins
Hair rinse resistance
3–6 rinses
5–6 rinses
Resist wash
Nature of hair colour
To add nuance
More natural look
Brown to black shade
Constituent
Characteristics and function
Commonly used agents
Coupling bases
Reaction modifiers/couplers
Alkalizing compound
Oxidizing agents
Reducing agents
Dyes
Antioxidants
Vehicles
Surfactants
Solvents
Emulsifiers
Photoprotectors
Preservatives
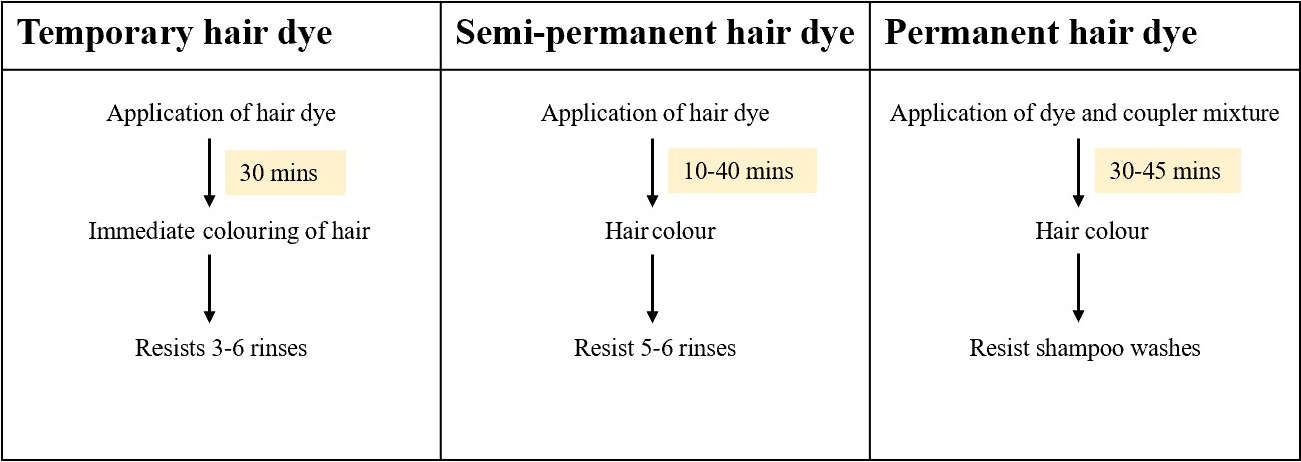
Various steps involved in hair dyeing.
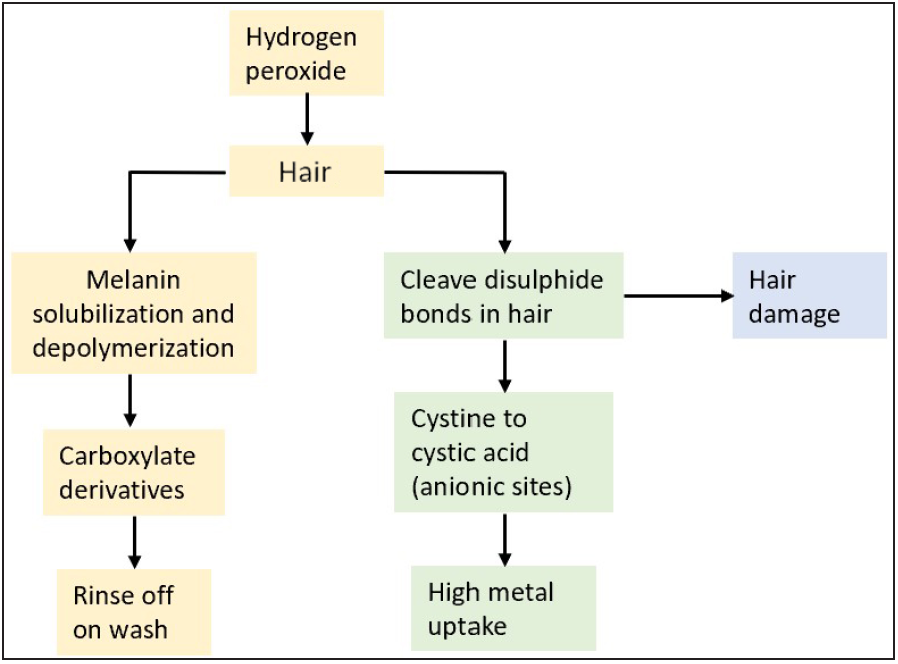
Mechanism of hair damage secondary to bleaching.
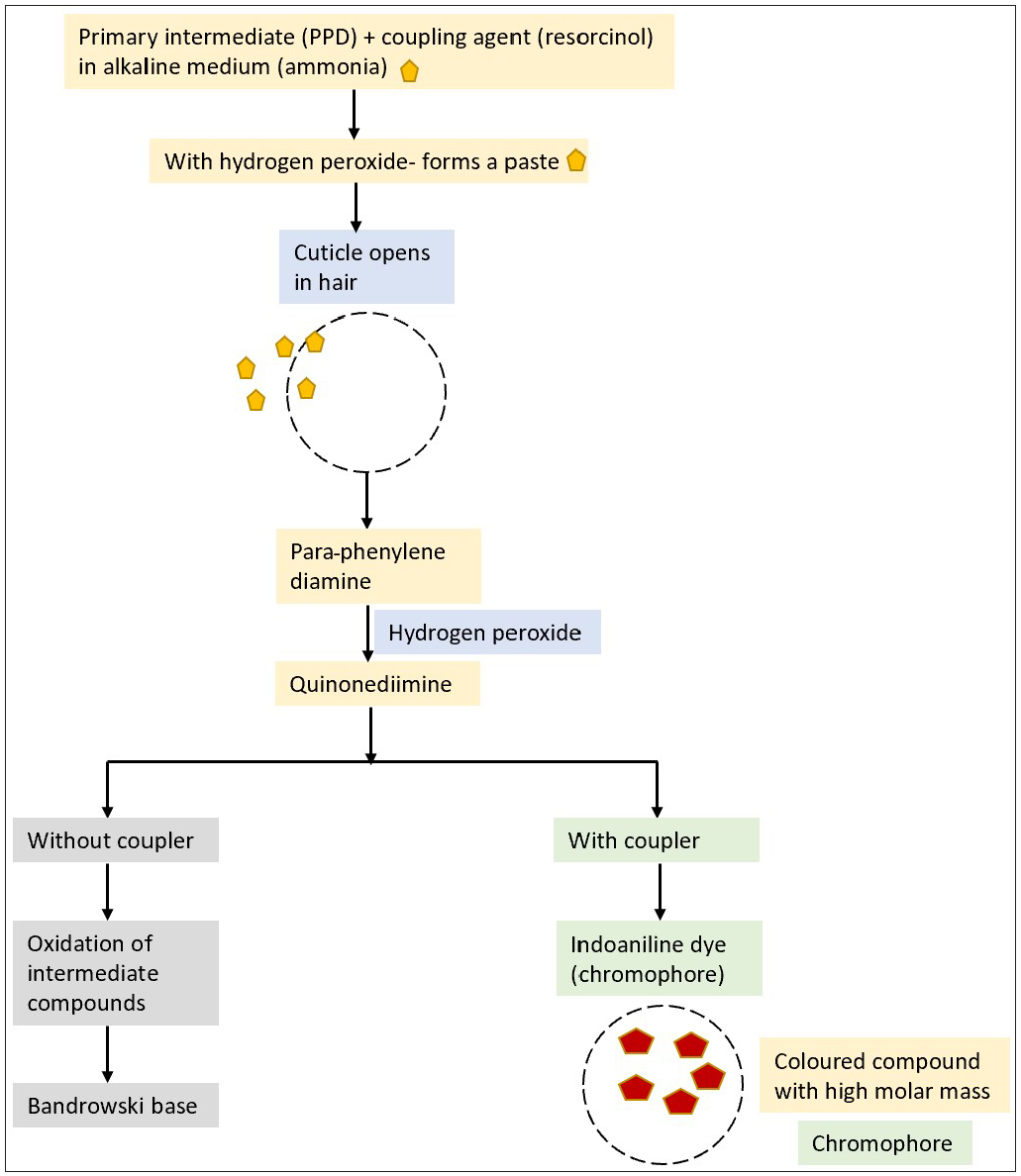
Process of hair colouring.
Epidemiology of hair dye use and contact sensitivity
Population-based epidemiological studies have found para-phenylenediamine sensitivity in the general population to be 0.1–1%.9 The prevalence of positive patch tests for para-phenylenediamine varies among dermatitis patients across the world, amounting to 11.5% in India, 6% in North America, 4.4% in Asia and 4.1% in Europe. Sensitization to para-phenylenediamine is more common in men than women in Asia, whereas it is the reverse in Europe.10,11 In an Indian study, it was found that among hair dye users, the mean age of first-time hair dye use was 27 years, and 42% of respondents reported adverse events following its use.12 Contact allergy to para-phenylenediamine can occur in 0.1–2.3% of the general population.7 Two Indian studies have found para-phenylenediamine to be the commonest sensitizer among cosmetics.13,14
Para-phenylenediamine
Para-phenylenediamine is a synthetic aromatic amine, a derivative of para-nitroaniline (coal–tar derivative) and is found in more than 1000 hair dye formulations.15 It is an effective compound found in nearly 70% of the hair dyes available worldwide owing to its small molecular weight, high protein-binding capacity, potential to penetrate the hair shaft, rapid polymerization when oxidized and due to the natural colour imparted to hair.6,16,17Para-phenylenediamine is a Class I allergen on lymph node assay and a potential contact sensitizer even in low concentrations.16,17
Contact sensitization to para-phenylenediamine often occurs due to various sources. Para-phenylenediamine is often used as a dye or antioxidant in various consumer and industry products such as fur, textiles, leather, rubber, paints, nylon stockings and industrial printing inks. Occupations which carry a high risk of contact with para-phenylenediamine are those of laboratory assistant, leather shop assistant, petrol pump attendant, masseur and jobs in the plastic, paper and cellulose manufacturing industries.18
The metabolism of para-phenylenediamine was studied by Bandrowski and still has not been completely elucidated. The metabolism of para-phenylenediamine in skin roughly involves two major pathways: (1) oxidation pathway and (2) acetylation pathway.19 The oxidative metabolites of para-phenylenediamine are the haptens that are responsible for para-phenylenediamine sensitization. Less than 1% of non-polymerised para-phenylenediamine undergoes acetylation in the epidermis without activating the T-cells and dendritic cells of sensitized individuals. The acetylation pathway gets saturated and increases the oxidative metabolites in the skin with exposure to large doses left for longer than the intended time of application and when carelessly applied, contaminating the nearby skin.17Apart from para-phenylenediamine, agents such as toluene-2,5-diamine, p-aminophenol, m-aminophenol, resorcinol, monoethanolamine, ammonium persulphates, ammonium thioglycolates, glyceryl thioglycolatesand sodium metabisulphite can produce contact dermatitis in hair dye users.7,19
Natural hair dyes
Henna (Lawsonia inermis) is a shrub with an active dye lawsone (2-hydroxy-1,4-naphthoquinone). The dried leaves of henna are powdered and mixed with water or oil and hair dyes are prepared.20,21 Natural henna is often mixed with coffee water or tea water overnight to make the colour more visible. The addition of natural substances such as vinegar, lemon oil and eucalyptus oil imparts different shades.7,8 Brown henna contains indigo plant leaves, black henna has para-phenylenediamine whereas red henna has no additives, hence its lower allergenic potential.20,21
Contact dermatitis to hair dye
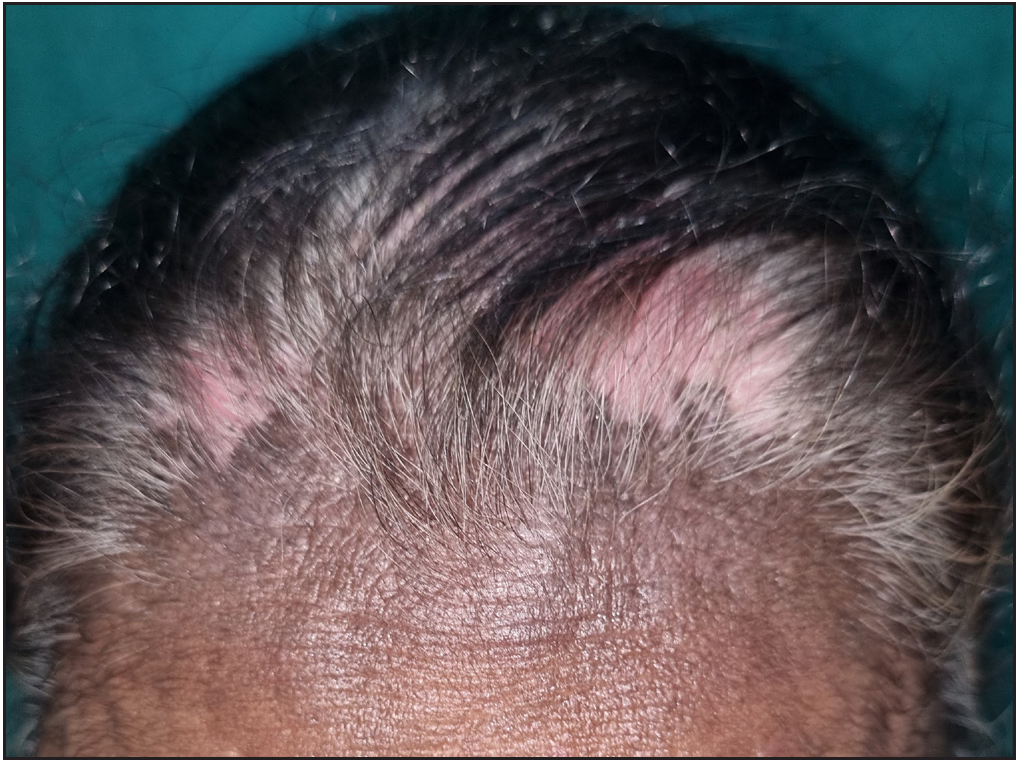
Hair dye contact dermatitis is a delayed hypersensitivity reaction, with signs and symptoms observed after a latent period of several hours to days following the hair dye use.6 It is common in the glabrous skin of the head and neck in the vicinity of the scalp (“rinse off areas”) [Figures 5–8]. Persons with mild hypersensitivity to hair dye can present only with dermatitis of the helices of ears and eyelids without affecting other facial areas or scalp.22 In a study of 105 patients with hair dye contact dermatitis, 64.8% showed lesions over the direct contact sites (scalp, face, neck), while 36.2% had lesions over both direct and indirect contact sites (trunk, hand, upper extremities, lower extremities and feet) [Figures 9 and 10].23

- Allergic contact dermatitis to hair dye extending from anterior hairline to forehead.

- Allergic contact dermatitis associated with hair loss following hair dye use.

- Lichenoid changes after the use of hair dye.
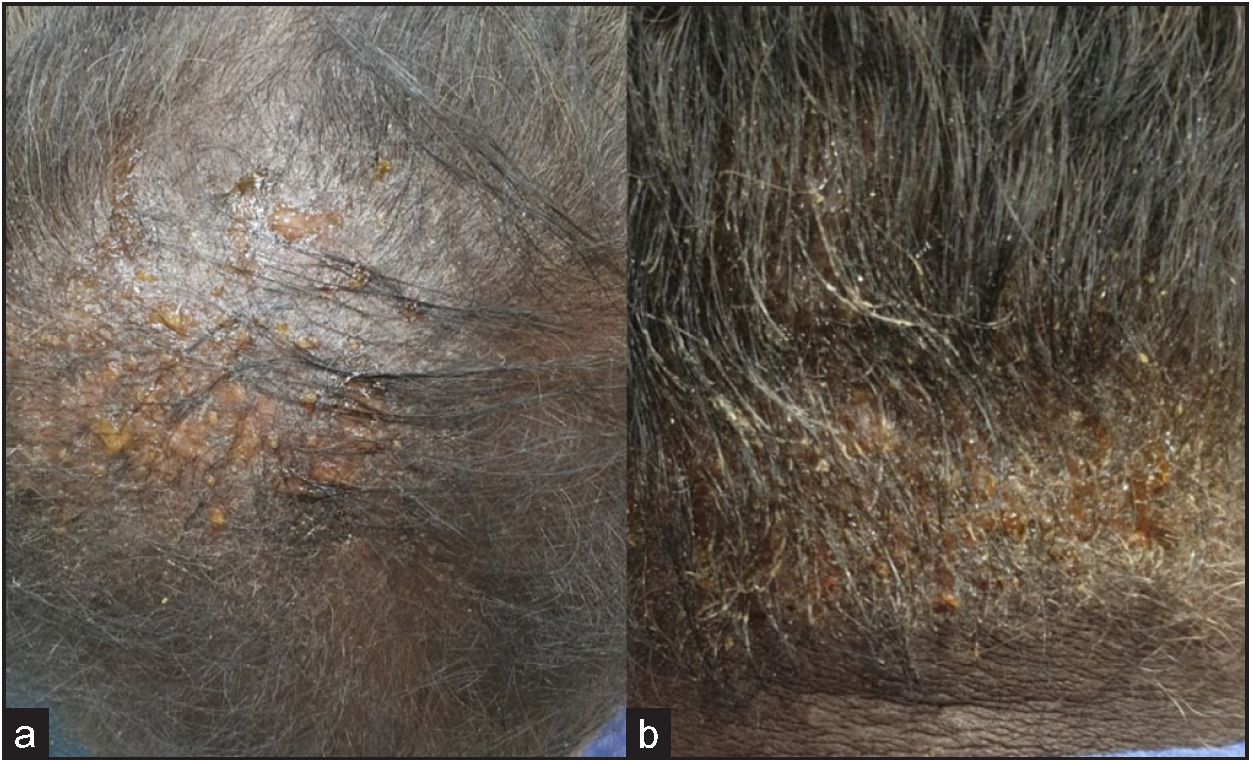
- Vesiculation, oozing and crusting associated with hair dye use.

- A hair dye user with pigmentary changes over the face and prurigo-like lesions over the upper extremities with positive patch test for para-phenylene diamine. Differential diagnoses of Riehl’s melanosis and ashy dermatoses for the face were considered. Prurigo nodularis and hypertrophic lichen planus were considered for the upper limb lesions.

- Disseminated hair dye dermatitis in a 32-year-old female. Patch test was positive for para-phenylenediamine. A differential diagnosis of seborrheic dermatitis and photo-allergic contact dermatitis were also considered.
Even though dyeing is commonly performed on the hair-bearing scalp, the allergen load in that area is grossly decreased due to increased skin thickness, protective sebum production, greater absorption of allergens into scalp hair and moderation by hair follicle regulation which are likely to promote tolerance.24,25 Among hairdressers, the most common sites for allergic contact dermatitis are the hands and arms [Figure 11]. In hairdressers, the cumulative effect from wet work results in irritant contact dermatitis with a defective skin barrier which in turn results in penetration of hair dye allergens.26 The thin stratum corneum of the facial skin and the need for frequent dyeing of the beard make the site more susceptible to contact dermatitis [Figure 12].27

- Hairdresser with allergic contact dermatitis on the dorsa of hands. She showed a positive reaction to para-phenylenediamine on patch testing. A differential diagnosis of polymorphous light eruption was considered.
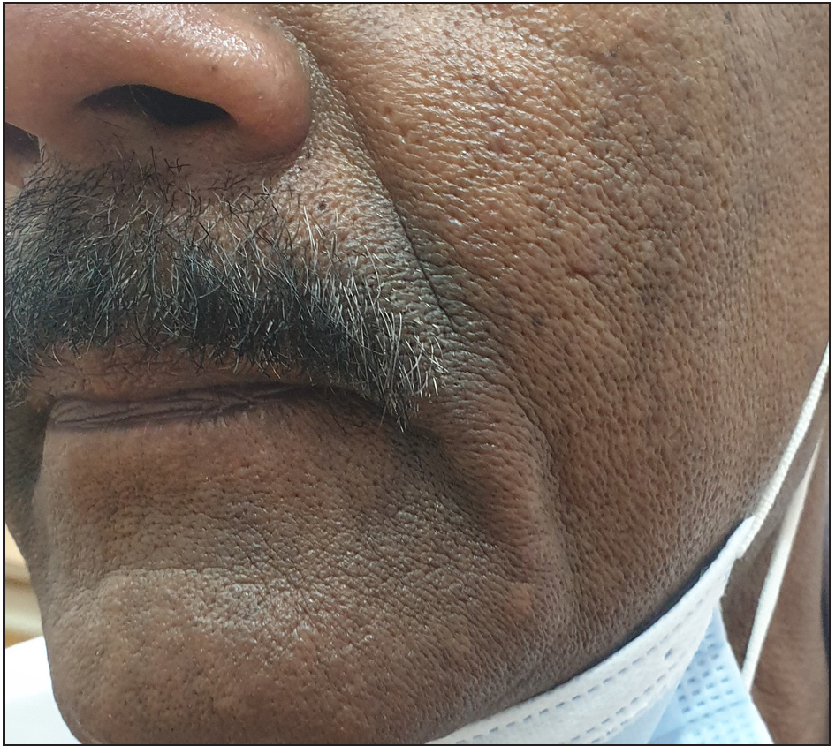
- Pigmentary contact dermatitis over the moustache region.
Hair dye contact dermatitis can produce symptoms such as redness, soreness, pruritus, dryness, pricking sensation, a burning or tingling sensation and discomfort.23,28 Many patients may experience photosensitivity.7 The signs observed include erythematous macules, patches, papules, plaques, vesicles, oozing, crusting, fissuring, lichenification, oedema, swelling, suppuration and ulceration at the affected sites.23,29 Hair dye use can also produce split ends in hair dryness, lustreless hair, hair loss, paradoxical excessive greying and slowing of hair growth.30 Oxidative hair dyes sometimes induce painful sensory irritation of the scalp.31 The morphological patterns of hair dye contact dermatitis are mentioned in Table 3.7,16 Patients with lichen simplex chronicus (LSC) with weak positive patch test reaction to para-phenylenediamine have shown improvement or complete clearing of the LSC lesions once they stopped using hair dye.32 Hair dye used by a person can produce connubial contact dermatitis in the partner.33 Localized contact dermatitis over scalp, scalp margins, face and neck Disseminated dermatitis Airborne contact dermatitis Eyelid eczema Periorbital eczema Irritant contact dermatitis Photocontact dermatitis Hand eczema Nummular dermatitis Chronic actinic dermatitis Lichenoid lesions Contact leukoderma Lymphomatoid papulosis-like lesions Erythema multiforme-like lesions Prurigo nodularis-like lesions Bullous contact dermatitis Exudative erythema
There is a recent trend of using black henna tattooing as a form of temporary body art in younger individuals. In black henna, para-phenylenediamine is added to natural henna to reduce the application time, increase intensity of the colour, improve pattern recognition and make the tattoo last longer. Some of them are sensitized to para-phenylenediamine in the black henna tattoos, and later when they use hair dye, can develop delayed hypersensitivity reactions to it even at lower concentrations of para-phenylenediamine.34,35
Type 1 hypersensitivity reactions to hair dye appears to occur after the process of oxidation. The reaction can manifest as urticaria, angioedema, rhinitis, asthma, bronchospasm and anaphylaxis [Figure 13].23,36

- Angioedema-like reaction following hair dye use.
Diagnosis of allergic contact dermatitis to hair dye
Patch test
Epicutaneous patch testing is the gold standard modality to confirm the allergy to hair dye.7 The patch test allergens to rule out hair dye allergy provided by Søsted et al. are mentioned in Table 4.37 However, as para-phenylenediamine is the most commonly encountered allergen in hair dye, it is included in the Indian Standard Series of allergens.6,17 The sensitivity of patch testing with para-phenylenediamine was found to be 87%.38 Population-based epidemiological studies have shown that patch testing with the recommended standard concentration of 1% para-phenylenediamine can result in highly delayed patch test reactions from day 7 in 1.5% of patients, probably reflecting iatrogenic sensitizations.39 Para-phenylenediamine Paratoluenediamine p-Methylaminophenol p-Aminophenol 4-Amino-2-hydroxytoulene m-aminophenol 2,4-Diaminophenoxyethanol–HCl 4-Amino-m-cresol 1-Hydroxyethyl-4,5-diaminopyrazole sulphate 2-Amino-3-hydroxypyridine 2-Methylresorcinol 3-Nitro-p-hydroxyethyaminophenol N,N’-Bis(2-hydroxyethyl)-p-phenylenediamine 4-Amino-3-nitrophenol 4-Chlororesorcinol Resorcinol 1-Napthol 2,4,5,6-Tetraaminopyridine 2,7-Naphthalenediol 2-Amino-6-chloro-4-nitophenol 2-Methyl-5-hydroxyethylaminophenol 4-Hydroxypropylamino-3-nitrophenol Acid Violet 43 Disperse Violet 1 HC Blue 2 HC Red 3 Picramic acid
The development of systemic anaphylactoid reaction 16 hours after a closed patch test with para-phenylenediamine has been reported.40 Patients with a history of severe reaction to hair dyes can be tested with para-phenylenediamine 1% pet for 1 hour. The patch test conducted with standard 1% pet para-phenylenediamine in patients previously sensitized to black henna exposure often results in strong reactions. Hence, some centres are recommending tests with 0.3% para-phenylenediamine concentration.6
Para-phenylenediamine may cross-react to other chemicals with an amine group on a benzene ring at the para position [Table 5].19 A retrospective study of 221 para-phenylenediamine patch test-positive patients found that severe patch test reactions (3+ rather than 1+ in international contact dermatitis research group (ICDRG) grading) have increased chances for cross-reactivity.40 Polysensitization is common among para-phenylenediamine-allergic patients with stronger responses (2+ and 3+).17 Carba mix, cobalt chloride, colophonium, methylchloroisothiazolinone, paraben mix and para-tertiary butylphenol formaldehyde resin are known to produce co-sensitization with para-phenylenediamine.41
Chemical
Use
Para-toluenediamine sulphate
Semipermanent hair dye, brown fur dyes, bleach-toner formula
Para-aminobenzoic acid
Sunscreens, pesticides
Para-amino salicylic acid
Antibiotics
N-isopropyl-N’-phenyl-p-phenylenediamine
Antioxidant in rubber
Sulfonylureas, sulfonamides
Medications
Azo dyes
Textiles, food, leather, plastics, rubber, paints
Benzocaine, tetracaine, procaine
Ester local anaesthetics
Thiazides
Diuretic medications
Sesquiterpene-lactone mix
Compositae family plants, cosmetics, topical medicaments
Hydroquinone
Skin depigmentation agent
Pyrogallol
Photographic developing agent
Black rubber mix
Rubber industries
Hair dye manufacturers recommend open testing by applying a small amount of hair dye behind the ear for 48 hours and looking for any allergenic reaction. It is a good screening test, but often misses the late and weak positive reactions.7 Repeated open application test (ROAT) had a sensitivity of 83.33% and specificity of 100% in patients with hair dye dermatitis in comparison to the patch test.42 Para-phenylenediamine-specific lymphocyte activation test (LAT) is a potential alternative in vitro system in patients with severe allergic contact reactions to para-phenylenediamine.39
Management of hair dye contact dermatitis
The withdrawal of the causative hair dye is the initial step in the management of hair dye contact dermatitis. In the case of acute severe hair dye contact dermatitis, the hair and scalp should be washed thoroughly to remove any surplus dye. Corticosteroids form the first-line treatment option in hair dye contact dermatitis.6,7 Short courses of potent topical corticosteroids applied once or twice daily for 2–3 weeks are preferred for localized hair dye contact dermatitis. If more than 10% of the body surface area is involved, systemic prednisolone (1–2 mg/kg) for 7–10 days, followed by tapering over the next 7–10 days, is administered. Wet dressings and oral antihistamines for soothing, relieving pruritus and reducing redness are given. A sunscreen should be advised for patients with photosensitivity.7
Adverse reactions due to hair dye use other than contact dermatitis
Hair dye–induced hyperpigmentation
Hair dyes are implicated in pigmentary alterations such as lichen planus pigmentosus and facial pigmented contact dermatitis [Figure 14].43,44 Earlier, Meghana et al. studied the pigmentary alterations of the face and neck in 118 hair dye users. Blotchy type (66.1%) followed by diffuse type (33.1%) of hyperpigmentation was commonly observed. In that study all the hair dye users had pigmentary alterations. The most frequently affected sites were the lateral forehead (88.3%), ear helix (88.3%) and central forehead (80.8%), an and zygomatic area (6.7%).45 In that study, the most frequently Bishnoi et al. described 108 patients with acquired dermal hyperpigmentation of the face and scalp clinically and interface dermatitis histologically. Of them, 83.3% used hair dye and 36.1% tested positive for para-phenylenediamine.46 Hair dye pigmentation has been reported to produce foreign body skull erosive granuloma.47

- Riehl’s melanosis in a chronic hair dye user.
Leukoderma
Initially, Taylor et al. in 1993 reported the ability of hair dyes to induce depigmentation. They described four patients who developed leukoderma of the scalp and hair following hair dye use.48 In a study of 864 cases of chemical leukoderma, around 27.4% of the patients developed depigmentation at the hair dye application site. It was limited to the contact site in 73.7% of individuals and extended beyond in 26.3% of patients [Figure 15].49
- Contact leukoderma following hair dye use.
The chemical structure of para-phenylenediamine is similar to that of tyrosine which is probably converted by tyrosine-related protein 1 into compounds that are toxic to melanocytes resulting in its loss within skin and hair follicles, resulting in depigmentation of skin and hair.50 The term “chemical-induced vitiligo” is often used to denote the depigmentation produced by chemicals like para-phenylenediamine. It cannot be clinically or histopathologically differentiated from vitiligo.51
Hair dye–induced hair loss
Hair dye use has been reported to produce telogen effluvium, cicatricial (lichenoid) alopecia, alopecia totalis and milphosis.52–55 An in vivo mouse model identified hydrogen peroxide and monoethanolamine as the key causative ingredients in hair dye–induced hair loss.56
Skin and other malignancies
The aromatic amine derivatives present in hair dyes are considered to be mutagenic. A large cohort study conducted in Sweden observed an increased risk of in situ carcinoma of the skin in the scalp and neck.57 In a study of 160 cases of basal cell carcinoma on the head and neck, it was observed that the odds of developing it were more among hair dye users, particularly those who used darker shades.58 A twofold increased risk of malignant melanoma in women using hair dye was noticed in a 37-year-old follow-up study.59 A case of hair dye-induced intracranial communicating sebaceous carcinoma of the scalp which developed 10 years after hair dyeing has been reported.60
In a large prospective cohort study of 1,17,000 personal hair dye users, increased incidence of breast carcinoma (oestrogen receptor-negative, progesterone receptor-negative, hormone receptor-negative), ovarian carcinoma and basal cell carcinoma was observed. Though evidence remains inadequate, individual or pooled relative risks were increased for malignancies such as lung carcinoma, prostate carcinoma and salivary gland carcinoma.61 An increased incidence of non-Hodgkin’s lymphoma, particularly follicular lymphoma is also associated with permanent hair dye use.62
Chemical burns
Severe chemical burns of the scalp following the application of hair dye requiring split-thickness skin graft are known.63 In the United Kingdom, hairdressers have noticed chemical burns in their clients following hair dye application in those who recently recovered from COVID-19.64
Hair dye use and systemic diseases
Exposure to para-phenylenediamine is postulated in the development of autoimmune phenomena, through various mechanisms such as apoptosis-mediated autoimmunity, molecular mimicry, immunological cross-reactivity and others, causing increased production of pro-inflammatory cytokines and immune complex formation.65,66 Exacerbation of discoid cutaneous lupus erythematosus following hair dyes have been reported.67 In addition, hair dye use has been associated with the development of systemic lupus erythematosus, rheumatoid arthritis, symmetrical polyarthritis and antinuclear antibody (ANA) positivity.68–71
Severe systemic toxicities following topical para-phenylenediamine exposure, resulting in rhabdomyolysis, kidney failure requiring haemodialysis, severe electrolyte derangements, severe anaphylaxis and myocardial infarction even resulting in death are reported.72,73 A study on the effects of long-term para-phenylenediamine exposure among hairdressers found a high prevalence of haematuria (41.1%), proteinuria (26.4%), renal impairment (14%), hypertension (19.4%) and bronchospasm (22%).74 In a case-control study, lenticular changes and early presbyopia were observed respectively in 89% and 7% of 200 hair dye users.75 Gestational maternal hair dye use has been associated with low birth-weight children and the development of neuroblastoma, leukaemia and allergic rhinitis in the children at a later age.76–78
Hair dye poisoning
Para-phenylenediamine has been reported to be a suicidal poisoning agent owing to its easy availability in households, low cost and tolerable taste. It is associated with a high mortality rate (12 to 42%) due to the non-availability of specific antidotes.79 The characteristic triad of hair dye poisoning is: (1) early angioneurotic oedema with stridor, (2) acute renal failure, and (3) rhabdomyolysis with chocolate-coloured urine. It can manifest as asphyxia, anuria or oliguria, metabolic acidosis, coagulation derangements, intravascular haemolysis, toxic myocarditis, arrhythmias, flaccid paralysis and gastrointestinal manifestations.80
Preventive measures and safety regulations
Oxidative processes in the skin play a vital role in the activation of para-phenylenediamine and its derivatives. Hence, pre-treatment of the glabrous skin surrounding the scalp with topical anti-oxidants like vitamin C cream or emulsion and 0.07% astaxanthin emulsion (with >6000-fold stronger antioxidant action than vitamin C) has been reported to decrease the incidence of hair dye allergy in para-phenylenediamine-sensitive patients.81,82 Patients with early, mild hair dye dermatitis have been advised in an article to use 0.05% clobetasol propionate foam applied twice daily over the affected area for 3 days before the next episode of hair colouring.83
Hairdressers should be advised not to use disposable natural rubber latex gloves and polyvinylchloride gloves while handling hair dye products for more than 1 hour. However, neoprene gloves and 4-H gloves are recommended as they protect hairdressers from hair dyes and perm chemicals.22,84 The strategies that can minimize the risk of development of contact dermatitis to hair dye are mentioned in Table 6. The recommended concentrations of para-phenylenediamine and toluene-2,5-diamine in hair dyes according to various regulations are mentioned in Table 7.16,39 Hair dye should be applied meticulously with minimal contact time Patients should not get misled by the high-pitched advertisements and should look at all the contents of the hair dye Use of hair foils or a highlight cap can minimize the risk of sensitization The scalp should be rinsed well after hair dyeing Immediate removal of hair dye if the adjacent area is contaminated Application of petrolatum to prevent the lateral spread of hair dye and to shield scalp margins Using lighter shades and less frequent dyeing will reduce the cumulative dose of dye on skin At production levels, manufacturers should keep the para-phenylenediamine concentration at a minimal level In patients with previous history of hair dye allergy, clear written advice should be given to look for allergenic ingredients Patients with para-phenylenediamine allergy should be warned regarding potential cross reaction to other substances with para-group Attention should be paid to all the “Caution” and “Warning” statements Different hair dye products should never be mixed Hair dressers should be educated about appropriate glove use and emollient use after work General population should be encouraged to perform open patch testing before using hair dye Pre-treatment of glabrous skin surrounding the scalp with topical antioxidants can minimise contact dermatitis Silver nitrate as the colour additive is recommended to colour eyebrows and eyelashes. Hair colouring should be carried out only by professional hairdressers. Application of petrolatum on surrounding areas before dyeing the beard can prevent contact dermatitis in that region. Para-phenylenediamine use in humans in “rinse off” products such as black hair dyes are approved for the US by the Food and Drug Administration irrespective of the concentration The European Union Cosmetic Directive (EUCD) allows a maximum concentration of 6% para-phenylenediamine in hair dyes EUCD allows a maximum concentration of 10% toluene-2,5-diamine in hair dyes Bureau of Indian Standards (BIS) has set a maximum permissible limit of 30% and not less than 3% para-phenylenediamine after dilution of the powder form BIS has set a maximum permissible limit of 4% and not less than 1.2% para-phenylenediamine after dilution of the oxidation liquid type. In Australia, a warning label is required for para-phenylenediamine concentrations higher than 5%.
Safe alternatives to hair dye
In recent times, a newer para-phenylenediamine derivative 2-methoxymethyl-para-phenylenediamine (2-methoxymethyl-para-phenylenediamine) has been formulated and investigated for safer hair dye use.85 The salient features of 2-methoxymethyl-para-phenylenediamine-based hair dyes are mentioned in Table 8. Venkatesan et al. introduced non-allergenic aromatic amine hair dyes as safe and efficient alternatives to para-phenylenediamine by introducing novel side chains to it.86 One report has suggested hydroxyethyl-p-phenylenediamine sulphate (HPPS) as a potential alternative to para-phenylenediamine.87 Natural botanical products that can be used for hair colouring are listed in Table 9.88 Less allergenic para-phenylenediamine derivative secondary to its methoxy-methyl side chain The peculiar side chain inhibits binding to the CD86 costimulatory molecule on antigen-presenting cells which is needed for T-cell activation It creates a hapten complex that is poorly recognized by para-phenylenediamine-specific T cells Attenuates the innate and adaptive immune response triggered by para-phenylenediamine Maintains an equivalent hair colouring performance to para-phenylenediamine and toluene-2,5-diamine sulphate-based dyes The concentration of ME-PPD needed to induce a local lymph node immune response is high (3–4%) as opposed to para-phenylenediamine (0–1%) Relatively safe permanent hair dye for para-phenylenediamine-allergic patients Allergic reaction even if encountered is expected to be less severe than that of para-phenylenediamine-based contact dermatitis Minimal cross reaction rate (30%) in para-phenylenediamine patch test positive individuals
Colourant
Plant origin
Lawsone
Leaves of Lawsonia inermis L
Juglone
Husk of Juglans regia L
Shikonin
Roots of Lithospermum erythrorhizon
Alizarin
Roots of Rubia tinctoria L
Benzoquinone
Pyrus lindleyi Rehd
Gallotannin
Parasitic aphids of Rhus chinensis Mill
Catechin
Matcha tea
Cyanidin-3-o-rutinoside
Fruit skins of Ribes nigrum L
Cyanidin-3-o-rutinoside
Fruit of Morus nigra L
Cyanidin-3-o-rutinoside
Beans of Phaseolus mungo
Cyanidin-3-o-rutinoside
Fruit of Cleistocalyx nervosum Var. Paniala
Cyanidin-3-o-rutinoside
Corn cobs of Zea mays L. Var.
Haematoxylin
Heartwood of Haematoxylon campechianum
Quercetin
Leaves of Tectona grandis Linn. F.
Acacetin
Barque of Acacia farnesiana (Linn.) Willd
Indigo
Leaves of Indigofera tinctorium
Curcumin
Root of Curcuma longa Linn
Zeaxanthin
Aerial parts of Eclipta alba L
Peridinin
Fruit of Terminalia belerica Roxb
Lutein
Flower of Tagetes erecta Linn
Conclusion
The use of hair dye has become quite common over the last few decades. It is a common sight for dermatologists to observe that many people continue to apply hair dye for various personal and social reasons even after developing an allergy to it. More scientific research should be carried out for the development of safer hair dyes. Till then, hair dyes will continue to be one of the most hazardous cosmetics used by mankind.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Market value of hair dye/color worldwide in 2020 and 2027. Statista. (May 25, 2022). Available from: https://www.statista.com/statistics/972997/global-hair-color-market-value/ [Last accessed on 2022 Aug 01].
- Henna as a hair dye: A current fashion trend with ancient roots. Dermatology. 2019;235:442-4.
- [CrossRef] [PubMed] [Google Scholar]
- Secrets in beautifying the head and face. In: Wecker J, Read R, eds. Eighteen books of the secrets of art and nature. London: St Paul Church-yard; p. :1661.:83.
- [Google Scholar]
- Bleaches, hair colorings and dye removers. In: Sagarin E, ed. Cosmetics science and technology. New York: Interscience Publishers Inc; 1957. p. :479-530.
- [Google Scholar]
- Para-phenylenediamine allergy: Current perspectives on diagnosis and management. J Asthma Allergy. 2017;10:9-15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Contact dermatitis to hair dye: An update. Indian J Dermatol Venereol Leprol. 2012;78:583-90.
- [CrossRef] [PubMed] [Google Scholar]
- Hair colouring: What a dermatologist should know? Int J Res Dermatol. 2021;7:496-502.
- [Google Scholar]
- Epidemiology of contact allergy in adults. Allergy. 2001;56:1192-6.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiological data on consumer allergy to p-phenylenediamine. Contact Dermatitis. 2008;59:327-43.
- [CrossRef] [PubMed] [Google Scholar]
- Common contact sensitizers in Chandigarh, India. A study of 200 patients with the European standard series. Contact Dermatitis. 1998;38:127-31.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in use of hair dye: A cross-sectional study. Int J Trichology. 2013;5:140-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Adverse reactions to cosmetics. Indian J Dermatol Venereol Leprol. 2003;69:165-7.
- [PubMed] [Google Scholar]
- Sensitizers commonly causing contact dermatitis from cosmetics. Contact Dermatitis. 2000;43:311-3.
- [PubMed] [Google Scholar]
- The effects of para-phenylenediamine (PPD) on the skin fibroblast cells. Xenobiotica. 2019;49:1143-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hair dye dermatitis and p-phenylenediamine contact sensitivity: A preliminary report. Indian Dermatol Online J. 2015;6:241-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Allergic contact dermatitis to para-phenylenediamine. Australas J Dermatol. 2015;56:40-3.
- [CrossRef] [PubMed] [Google Scholar]
- Side-effects of henna and semi-permanent ‘black henna’ tattoos: A full review. Contact Dermatitis. 2013;69:1-25.
- [CrossRef] [PubMed] [Google Scholar]
- Two cases of pigmented contact dermatitis caused by pure henna hair dyes. Ann Dermatol. 2018;30:735-7.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired diffuse slate-grey facial dyspigmentation due to henna: An unrecognized cause of pigment contact dermatitis in Korean patients. Eur J Dermatol. 2018;28:644-8.
- [CrossRef] [PubMed] [Google Scholar]
- Rietschel RL, Fowler Jr JF, eds. Fisher’s Contact Dermatitis (6th ed). Hamilton: BC Decker Inc; 2008.
- P-Phenylenediamine hair dye allergy and its clinical characteristics. Ann Dermatol. 2018;30:316-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Influence of vitamin C on the elicitation of allergic contact dermatitis to p-phenylenediamine. Contact Dermatitis. 2016;74:368-72.
- [CrossRef] [PubMed] [Google Scholar]
- Currently relevant p-phenylenediamine patch test reactions associated with hair dye and nonscalp anatomic areas: Retrospective cross-sectional analysis of North American Contact Dermatitis Group data, 2001 to 2016. J Am Acad Dermatol. 2021;84:175-7.
- [CrossRef] [PubMed] [Google Scholar]
- Contact dermatitis to hair cosmetics: Current diagnostic recommendations. J Dtsch Dermatol Ges. 2021;19:1729-34.
- [Google Scholar]
- Beard dermatitis due to para-phenylenediamine use in Arabic men. J Am Acad Dermatol. 2001;44:867-9.
- [CrossRef] [PubMed] [Google Scholar]
- Occupational asthma, rhinitis and contact urticaria from indigo (Indigofera tinctoria) hair dye. J Allergy Clin Immunol Pract. 2021;9:3500-2.
- [CrossRef] [PubMed] [Google Scholar]
- 55 cases of allergic reactions to hair dye: A descriptive, consumer complaint-based study. Contact Dermatitis. 2002;47:299-303.
- [CrossRef] [PubMed] [Google Scholar]
- Local side effects caused by hair dye use in females: cross-sectional survey. J Cutan Med Surg. 2012;16:39-44.
- [CrossRef] [PubMed] [Google Scholar]
- Significance of hair-dye base-induced sensory irritation. Int J Cosmet Sci. 2010;32:217-24.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic contact dermatitis from hair dye and development of lichen simplex chronicus. Contact Dermatitis. 2004;51:5-8.
- [CrossRef] [PubMed] [Google Scholar]
- Allergic contact connubial dermatitis caused by hair products. Contact Dermatitis. 2019;80:186-7.
- [CrossRef] [PubMed] [Google Scholar]
- Temporary holiday “tattoos” may cause lifelong allergic contact dermatitis when henna is mixed with PPD. J Cosmet Dermatol. 2003;2:126-30.
- [CrossRef] [PubMed] [Google Scholar]
- Hypersensitivity reactions due to black henna tattoos and their components: Are the clinical pictures related to the immune pathomechanism? Clin Mol Allergy. 2017;10:15:8.
- [Google Scholar]
- Allergic contact urticaria secondary to hair dye use. Contact Dermatitis. 2017;77:257-9.
- [CrossRef] [PubMed] [Google Scholar]
- Contact allergy to common ingredients in hair dyes. Contact Dermatitis. 2013;69:32-9.
- [CrossRef] [PubMed] [Google Scholar]
- Patch test dose-response study of p-phenylenediamine: Thresholds and anatomical regional differences. Contact Dermat. 2006;54:145-9.
- [Google Scholar]
- Para-phenylenediamine-specific lymphocyte activation test: A sensitive in vitro assay to detect para-phenylenediamine sensitization in patients with severe allergic reactions. Exp Dermatol. 2010;19:435-41.
- [CrossRef] [PubMed] [Google Scholar]
- Anaphylactoid reaction during patch testing for hair dye: A risk of skin testing. Contact Dermatitis. 2021;84:123-4.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of concordance between labelling and content of 52 hair dye products: overview of the market of oxidative hair dye. Eur J Dermatol. 2017;27:123-31.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of patch test with repeated open application test in patients with suspected hair-dye dermatitis. Indian J Dermatol Venereol Leprol. 2020;86:733-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy and patch testing in patients with lichen planus pigmentosus on face: A cross-sectional observational study in fifty Indian patients. Ind J Dermatol Venereol Leprol. 2017;83:656-62.
- [Google Scholar]
- Face and neck pigmentary alterations in hair dye users: A cross-sectional study from South India. Indian Dermatol Online J. 2020;11:760-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Contact sensitization to hair colors in acquired dermal macular hyperpigmentation: Results from a patch and photo patch-test study of 108 patients. J Eur Acad Dermatol Venereol. 2019;33:1349-57.
- [CrossRef] [PubMed] [Google Scholar]
- Caution with hair dye: Foreign body skull erosive granuloma from exogenous hair pigmentation. Ann Acad Med Singap. 2020;49:340-2.
- [PubMed] [Google Scholar]
- Contact leukoderma associated with the use of hair colors. Cutis. 1993;52:273-80.
- [PubMed] [Google Scholar]
- Chemical leucoderma: a clinico-aetiological study of 864 cases in the perspective of a developing country. Br J Dermatol. 2009;160:40-7.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical leukoderma from hair dye containing para-phenylenediamine. Dermatitis. 2012;23:181-2.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical-induced vitiligo. Dermatol Clin. 2017;35:151-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Severe hair loss of the scalp due to a hair dye containing para phenylenediamine. ISRN Dermatol. 2011;2011:947284.
- [CrossRef] [PubMed] [Google Scholar]
- Cicatricial alopecia following allergic contact dermatitis from hair dyes: A rare clinical presentation. Contact Dermatitis. 2022;86:59-61.
- [CrossRef] [PubMed] [Google Scholar]
- A case report of alopecia totalis associated with permanent hair dye use. J Am Acad Dermatol. 2020;6:801-3.
- [Google Scholar]
- Loss of eyelashes after use of a tinting mascara containing PPD. Contact Dermatitis. 2006;54:169-70.
- [Google Scholar]
- Hydrogen peroxide and monoethanolamine are the key causative ingredients for hair dye-induced dermatitis and hair loss. J Dermatol Sci. 2012;66:12-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cancer risks in hairdressers: assessment of carcinogenicity of hair dyes and gels. Int J Cancer. 2003;105:108-12.
- [CrossRef] [PubMed] [Google Scholar]
- Relation of basal cell carcinoma to hair dye use. J Am Acad Dermatol. 2009;61:532-3.
- [CrossRef] [PubMed] [Google Scholar]
- Morbidity and mortality in 7,684 women according to personal hair dye use: The copenhagen city heart study followed for 37 years. PLoS One. 2016;11:e0151636.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Intracranial infiltration of a scalp neoplasm after hair dyeing 10 years ago. J Craniofac Surg. 2021;32:790-2.
- [Google Scholar]
- Personal use of permanent hair dyes and cancer risk and mortality in US women: prospective cohort study. BMJ. 2020;370:m2942.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Is there a true concern regarding the use of hair dye and malignancy development?: A review of the epidemiological evidence relating personal hair dye use to the risk of malignancy. J Clin Aesthet Dermatol. 2013;6:39-46.
- [Google Scholar]
- Hair bleaching and skin burning. Ann Burns Fire Disasters. 2012;25:200-2.
- [PubMed] [PubMed Central] [Google Scholar]
- Burns from hair dye in recovered COVID-19 patients, a new presentation for further investigation. Burns. 2022;48:481-2.
- [CrossRef] [PubMed] [Google Scholar]
- Viral triggers for autoimmunity: is the ‘glass of molecular mimicry’ half full or half empty? J Autoimmun. 2010;34:38-44.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Role of regulatory T cells in rheumatoid arthritis: facts and hypothesis. Auto Immun Highlights. 2010;1:45-51.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Discoid lupus triggered by allergic contact dermatitis caused by a hair dye. Contact Dermatitis. 2016;74:61-4.
- [CrossRef] [PubMed] [Google Scholar]
- N-acetyl transferase genotypes in relation to risk of developing systemic lupus erythematosus. J Rheumatol. 2004;31:76-80.
- [PubMed] [Google Scholar]
- Smoking and use of hair treatments in relation to risk of developing systemic lupus erythematosus. J Rheumatol. 2001;28:2653-6.
- [PubMed] [Google Scholar]
- Occupational mimics of rheumatoid arthritis: hair dye-induced arthritis. Rheumatol Int. 2021;41:795-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Occupational and environmental associations with antinuclear antibodies in a general population sample. J Toxicol Environ Health A. 2006;69:2063-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fatal anaphylactic reaction to hair dye. Am J Forensic Med Pathol. 1997;18:290-2.
- [CrossRef] [PubMed] [Google Scholar]
- Systemic anaphylaxis due to an oxidation product of p-phenylenediamine in a hair dye. Ann Allergy. 1987;58:205-8.
- [PubMed] [Google Scholar]
- The association between prolonged occupational exposure to paraphenylenediamine (hair-dye) and renal impairment. Arab J Nephrol Transplant. 2011;4:21-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cataractogenous effect of hair dyes: A clinical and experimental study. Ann Ophthalmol. 1979;11:1681-6.
- [PubMed] [Google Scholar]
- Association between gestational hair dye use and allergies at 3 years old: the Japan environment and Children’s study. Environ Res. 2021;201:111530.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal hair dye use and risk of neuroblastoma in offspring. Cancer Causes Control. 2005;16:743-8.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of pre-pregnancy hair dye exposure on infant birth weight: a nested case-control study. BMC Pregnancy Childbirth. 2018;18:144.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Paraphenylenediamine containing hair dye: An emerging household poisoning. Am J Forensic Med Pathol. 2015;36:167-71.
- [CrossRef] [PubMed] [Google Scholar]
- Fatal poisoning caused by oral ingestion of a hair dye. Internet J Emerg Intensive Care Med. 2008;11:2.
- [Google Scholar]
- Influence of vitamin C on the elicitation of allergic contact dermatitis to p-phenylenediamine. Contact Dermatitis. 2016;74:368-72.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of astaxanthin on allergic contact dermatitis in response to hair dye containing p-phenylenediamine. Eur J Dermatol. 2019;29:647-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mitigation or prevention of mild hair dye contact dermatitis after pretreatment with clobetasol foam. J Am Acad Dermatol. 2017;77:129.
- [Google Scholar]
- Permeation of hair dye ingredients, p-phenylenediamine and aminophenol isomers, through protective gloves. Ann Occup Hyg. 2009;53:289-96.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-elicitation responses to 2-methoxymethyl-p-phenylenediamine under hair dye use conditions in p-phenylenediamine-allergic individuals. Br J Dermatol. 2015;172:976-80.
- [CrossRef] [PubMed] [Google Scholar]
- Development of novel alternative hair dyes to hazardous para-phenylenediamine. J Hazard Mater. 2021;402:123712.
- [CrossRef] [PubMed] [Google Scholar]
- Patch testing with hydroxyethylp-phenylenediamine sulfate - cross-reactivity with p-phenylenediamine. Contact Dermatitis. 2011;65:96-100.
- [CrossRef] [PubMed] [Google Scholar]
- Recent advancements in natural plant colorants used for hair dye applications: A review. Molecules. 2022;27:8062.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hair colouring: What a dermatologist should know? Int J Res Dermatol. 2021;7:496-502.
- [Google Scholar]
- U.S. Food and Drug Administration. Hair dyes. Accessed 18 July 2023. Available from: https://www.fda.gov/cosmetics/cosmetic-products/hair-dyes [Last accessed on 2022 Feb 25].






