Translate this page into:
Dermatophytoma: An under-recognized condition
Correspondence Address:
Chuda Rujitharanawong
Department of Dermatology, Faculty of Medicine Siriraj Hospital, Mahidol University, 2 Wanglang Road, Bangkoknoi, Bangkok 10700
Thailand
| How to cite this article: Leeyaphan C, Bunyaratavej S, Prasertworanun N, Muanprasart C, Matthapan L, Rujitharanawong C. Dermatophytoma: An under-recognized condition. Indian J Dermatol Venereol Leprol 2016;82:188-189 |
Sir,
Dermatophytoma appears as linear, single or multiple white or yellow bands on the nail plate and can be easily diagnosed from external appearances. Biofilm development is proposed for the pathogenesis of this infection that is composed of a fungal ball formed by abundant fungal filaments and large spores. [1],[2],[3] As the fungal mass firmly attaches to the nail plate and produces an extracellular polysaccharide, it leads to decreased antifungal penetration making the condition resistant to standard antifungal therapy. [4],[5] Oral antifungal treatment alone is not enough to treat this condition [6] and either chemical or physical debridement is essential to eliminate dermatophytoma. [7]
General practitioners and non-dermatologist specialists are usually the first to treat fungal nail infections but their knowledge of dermatophytoma treatment is probably limited. As a first step in developing the clinical practice standard for the treatment of dermatophytoma, we evaluated knowledge about this condition in general practitioners and non-dermatologist specialists at the annual meeting of the Dermatological Society of Thailand in February 2013. We used questionnaires and a short answer pretest, composed of a typical picture of toenail dermatophytoma followed by three questions: What is the diagnosis? How would you assess this patient? What is the appropriate management? [Figure - 1]. The questionnaire also asked about the respondent′s level of confidence in the management of dermatologic patients. The study was approved by the hospital ethics committee.
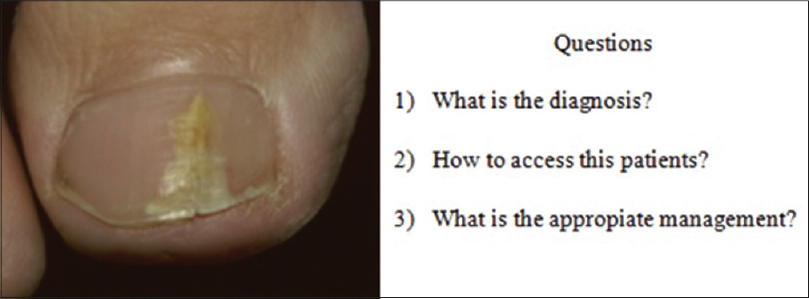 |
| Figure 1: Dermatophytoma. Three short answer questions and typical picture of the toenail dermatophytoma |
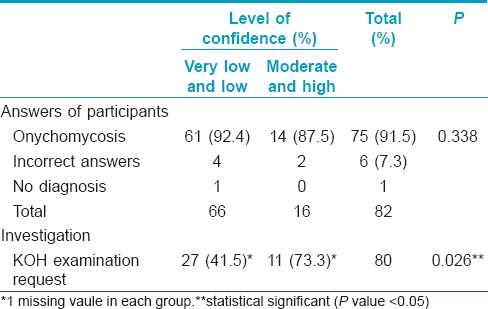
This test was taken by 82 (96.5% of those registered) physicians who voluntarily returned their answer sheets. Sixty-six (80.5%) participants were general practitioners while the rest were non-dermatologist specialists. Among the physicians, 59 (72%) were female. The largest group consisted of 38 (46.3%) physicians aged from 26 to 30 years followed by 24 (29.3%) physicians aged from 20 to 25 years. Our analysis found that 75 (91.5%) physicians provided us with an accurate diagnosis of onychomycosis but 42 (51.2%) physicians did not request a potassium hydroxide (KOH) examination. Interestingly, the self reported level of confidence in managing dermatology cases correlated with the requesitioning of investigations for mycological examination. The group of physicians with low and very low confidence sent fewer samples for confirming mycological disease compared with those in the moderately and highly confident group (P = 0.026) [Table - 1]. Among the 75 physicians who made the right diagnosis, 42 (63.4%) stated they would manage the condition with oral antifungal treatment, 18 (22%) mentioned a combination of topical and oral antifungal treatment and 3 (3.7%) mentioned antifungal drugs but did not specify the route of administration. However, only 2 physicians mentioned the additional requirement of mechanical debridement.
Our study shows that onychomycosis is recognized by both general practitioners and non-dermatologist specialists, but dermatophytoma is not. However, physicians should learn to diagnose dermatophytoma as it requires mechanical debridement in addition to the topical and oral antifungal agents used in regular practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Scher RK, Tavakkol A, Sigurgeirsson B, Hay RJ, Joseph WS, Tosti A, et al. Onychomycosis: Diagnosis and definition of cure. J Am Acad Dermatol 2007;56:939-44.
[Google Scholar]
|
| 2. |
Roberts DT, Evans EG. Subungual dermatophytoma complicating dermatophyte onychomycosis. Br J Dermatol 1998;138:188-203.
[Google Scholar]
|
| 3. |
Martinez-Herrera E, Moreno-Coutiño G, Fernández-Martínez RF, Finch J, Arenas R. Dermatophytoma: Description of 7 cases. J Am Acad Dermatol 2012;66:1014-6.
[Google Scholar]
|
| 4. |
Burkhart CN, Burkhart CG, Gupta AK. Dermatophytoma: Recalcitrance to treatment because of existence of fungal biofilm. J Am Acad Dermatol 2002;47:629-31.
[Google Scholar]
|
| 5. |
Bennett D, Rubin AI. Dermatophytoma: A clinicopathologic entity important for dermatologists and dermatopathologists to identify. Int J Dermatol 2013;52:1285-7.
[Google Scholar]
|
| 6. |
Sigurgeirsson B. Prognostic factors for cure following treatment of onychomycosis. J Eur Acad Dermatol Venereol 2010;24:679-84.
[Google Scholar]
|
| 7. |
Epstein E. How often does oral treatment of toenail onychomycosis produce a disease-free nail? Arch Dermatol 1998;134:1551-4.
[Google Scholar]
|
Fulltext Views
7,111
PDF downloads
2,208





