Translate this page into:
Dermatoscopic and high frequency ultrasound evaluation in lupus miliaris disseminatus faciei
Corresponding author: Dr. Yuping Ran, Department of Dermatovenereology, West China Hospital, Sichuan University, Chengdu, Sichuan, China. ranyuping@vip.sina.com
-
Received: ,
Accepted: ,
How to cite this article: Li C, Wang Y, Zhang L-W, Wang W, Ran Y. Dermatoscopic and ultra-high frequency ultrasound evaluation in lupus miliaris disseminatus faciei. Indian J Dermatol Venereol Leprol 2023;89:792
Dear Editor,
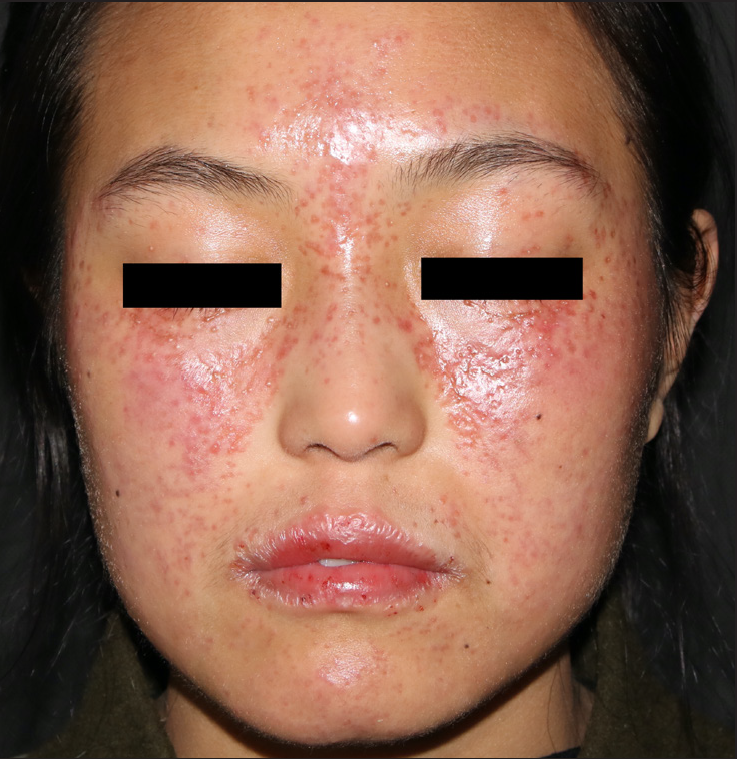
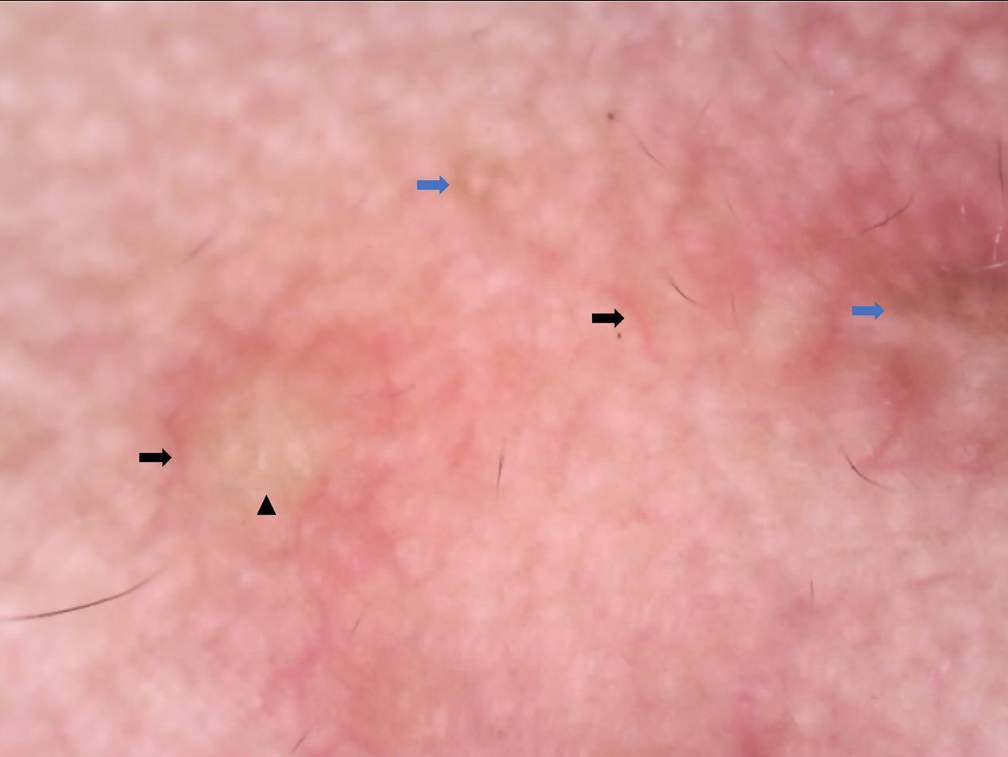
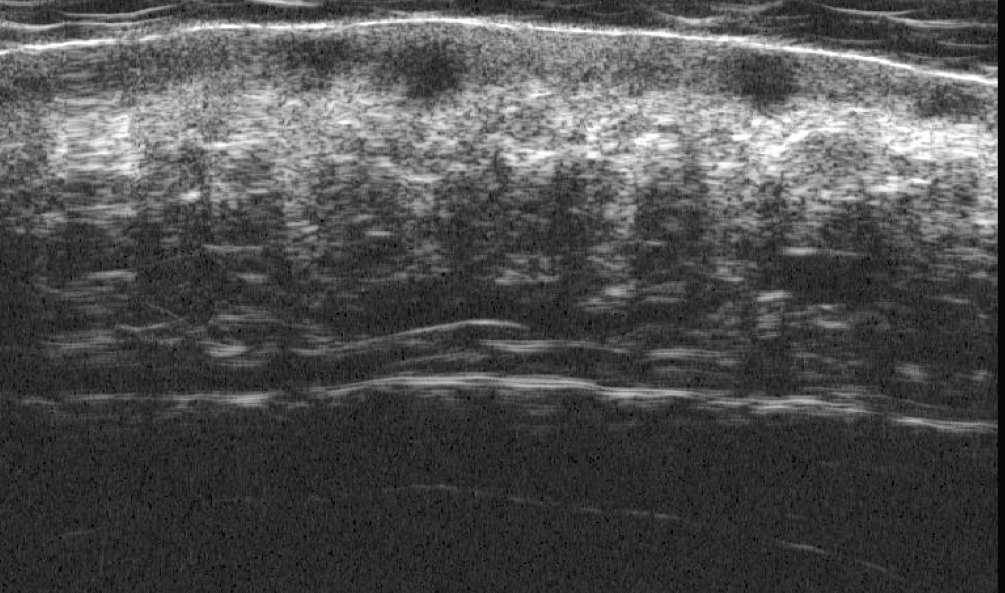
We describe a case of lupus miliaris disseminatus faciei (LMDF) in a 21-year-old woman with a 5-month history. Clinical evaluation revealed multiple, dome-shaped, reddish-yellow papules, distributed symmetrically on nearly the entire face, especially the central area, namely, the glabella, lower eyelids, cheeks and chin [Figure 1]. Dermoscopy showed linear and arborizing vessels on a yellow-reddish background, some with targetoid follicular plugs and several lesions coalescing [Figure 2]. Ultrasonography with a 50 MHz probe showed multiple well-defined peanut-like hypoechoic areas within the dermis [Figure 3]. Histological examination of the papule showed dermal epithelioid cell granulomas, infiltration of dermal lymphocytes, neutrophils and a small number of plasma cells and multifocal tissue cell aggregation perigranulomatous [Figure 4a-b]. The well-defined hypoechoic area on ultrasonography corresponded to the dermal inflammation formed of granulomas and inflammatory cells around them. Blood investigations such as complete blood count, erythrocyte sedimentation rate and hepatic and renal function tests were normal. Chest X-ray was normal and Tuberculous infection of T cells spot (T-SPOT) test was negative. With these clinical, pathological and laboratory findings, a diagnosis of lupus miliaris disseminatus faciei was made.
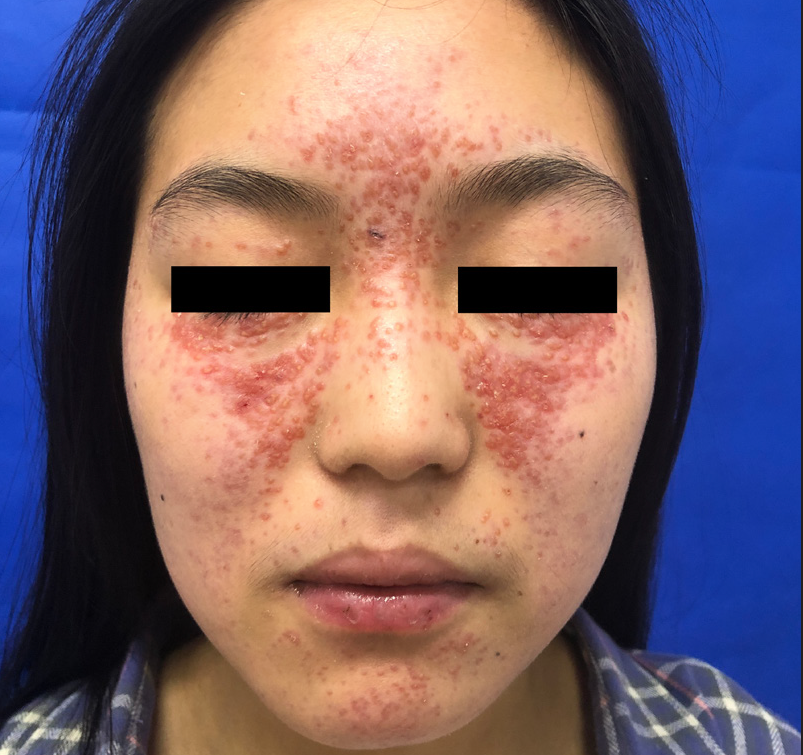
- Clinical evaluation revealed multiple, dome-shaped, reddish-yellow papules, distributed symmetrically on nearly the entire face, especially the central area
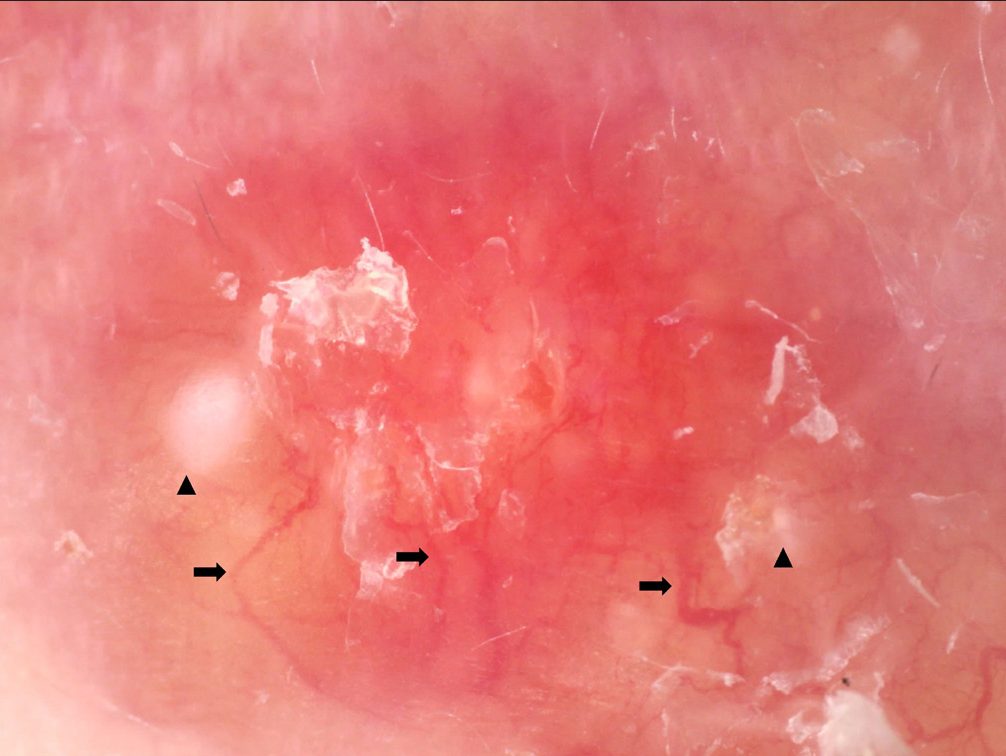
- Dermoscopy showed linear and arborizing vessels (black arrow) on a yellow-reddish background, some with targetoid follicular plugs (black triangle), some lesions coalesce (×50, non-contact, polarized light, JEDA®, Jiangsu, China)
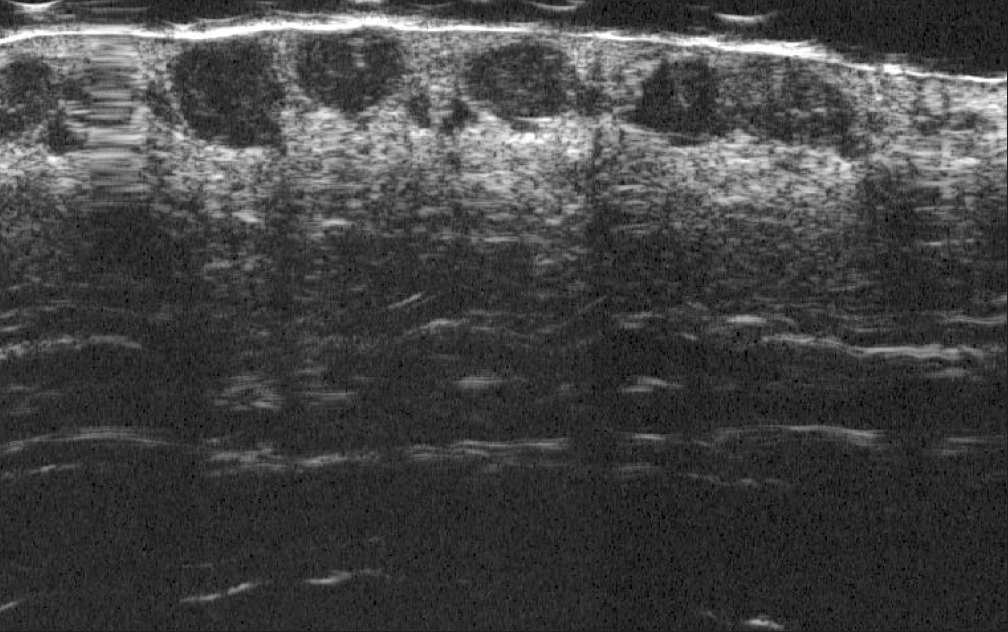
- The ultrasonographic examination revealed multiple well-defined peanut-like hypoechoic 20 MHz areas
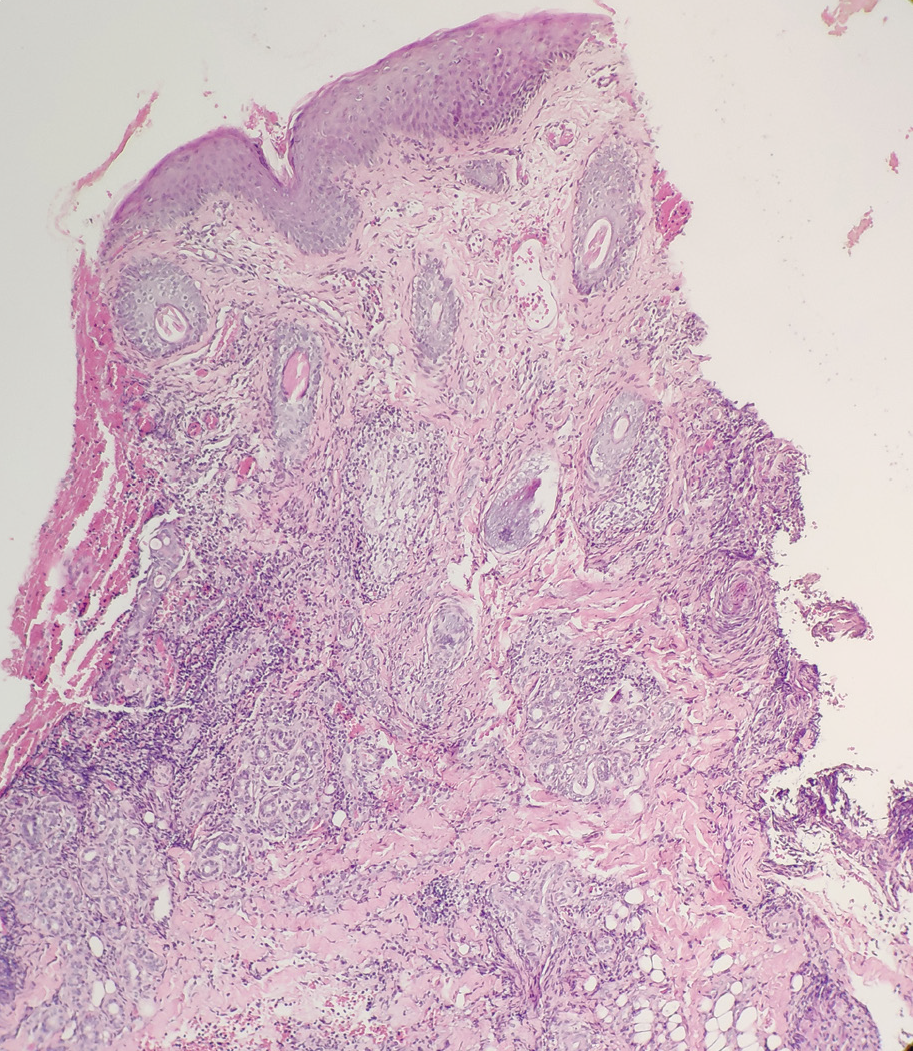
- Histological examination of the papule showed dermal epithelioid cell granulomas, infiltration of dermal lymphocytes, neutrophils and a small amount of plasma cells and multifocal tissue cell aggregation (HE×100)
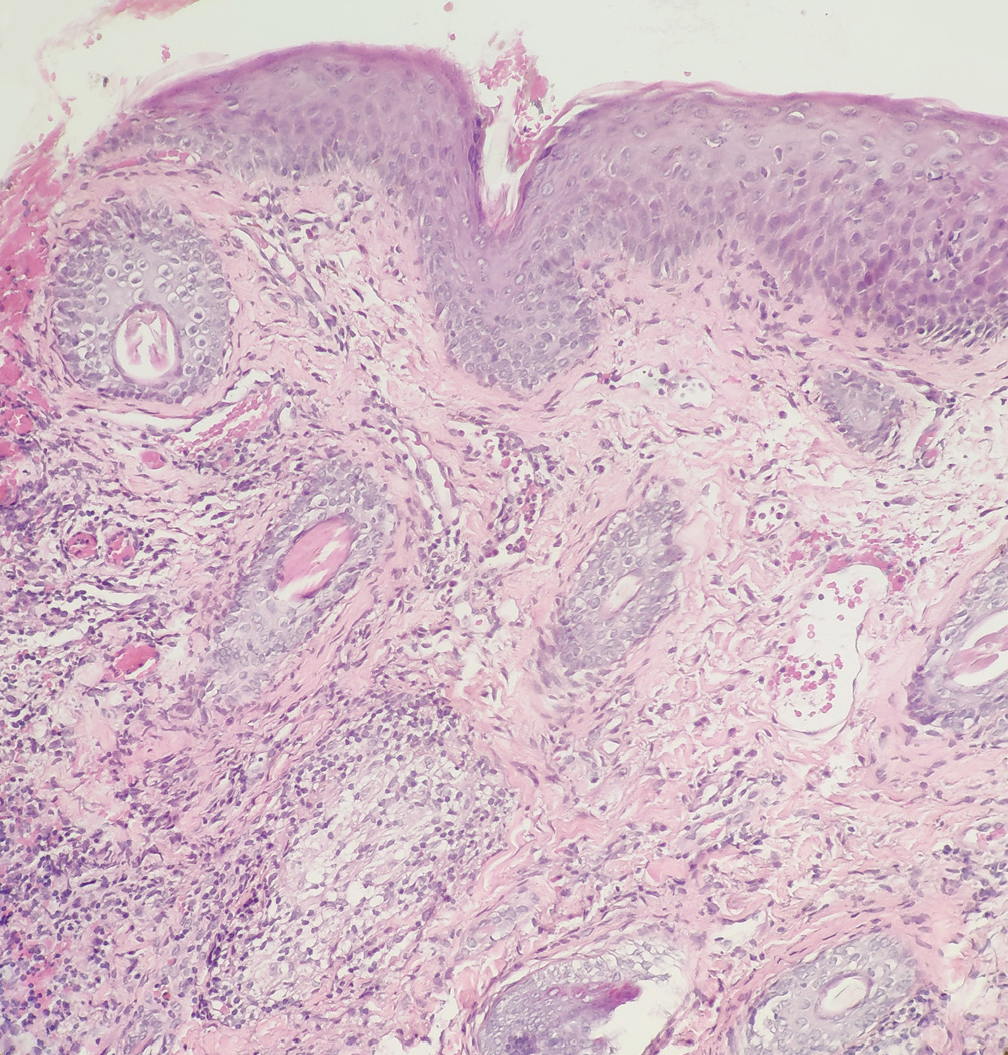
- Histological examination of the papule showed dermal epithelioid cell granulomas, infiltration of dermal lymphocytes, neutrophils and a small amount of plasma cells and multifocal tissue cell aggregation (HE×200)
The patient was treated with oral minocycline 50 mg twice daily for a period of 2 months along with hydroxychloroquine 200 mg twice daily with a little improvement. Minocycline was discontinued and isotretinoin 10 mg was given thrice daily. She was reviewed every month and showed progressive improvement. After 8 months of therapy, most papules flattened and diminished, leaving atrophic scars [Figure 5]. Dermatoscopically, the background became whitish-pink, telangiectasia decreased and white homogeneous unstructured area and brown pigmentation were revealed [Figure 6]. Ultrasonography showed a diminution of hypoechoic areas [Figure 7].
- Most papules flattened and diminished leaving some scars after 8 months of therapy
- Under dermatoscopic examination, the background becomes whitish-pink, angiectasis (black arrow) were decreased and white homogeneous unstructured area (black triangle) and brown pigmentation (blue arrow) were revealed (×50, non-contact, polarized light, JEDA®, Jiangsu, China)
- Ultrasonography presented dimunation of dermal granulomas
Lupus miliaris disseminatus faciei is a rare, inflammatory and granulomatous eruption of unknown aetiology. Although it was originally considered a variation of lupus vulgaris or a form of tuberculid, the association with mycobacteria is controversial. This is due to the self-healing nature of the disease, the inability to identify bacilli and the lack of response to anti-tuberculosis treatment. It needs to be differentiated from other facial granulomatous papules such as cutaneous sarcoidosis, granulomatous rosacea, cutaneous leishmaniasis, granuloma faciale and pseudolymphomas. 1
The most characteristic dermatoscopic feature of lupus miliaris disseminatus faciei is discrete focal orange structureless areas which may correspond histopathologically to dermal granuloma and resemble other granulomatous dermatoses. However, the detection of additional dermatoscopic features may be helpful for distinguishing it from the other differentials. It presents under dermoscopy as discrete focal orangish structureless areas around follicular openings filled with whitish or yellowish keratotic plugs which are often surrounded with crown-like vessels. 2 Sarcoidosis shows well-focused linear or branching vessels. Granulomatous rosacea is characterized by linear reddish or purple vascular polygons. Granuloma faciale may be identified by a pink background with some areas blackened, white striations in different directions and prominent follicular orifices. 3
To improve diagnostic accuracy, non-invasive methods such as cutaneous ultrasound can provide valuable data about the size, depth, margins and vascularization of subcutaneous lesions. For instance, in our case,4 we detected heterogeneous, hypoechoic, well-defined peanut-like lesions in the dermis of lupus miliaris disseminatus faciei by ultrasound examination. We were unable to find any previous reports of the ultrasound that had been used to evaluate lupus miliaris disseminatus faciei.
In conclusion, the combined use of dermoscopy and high-frequency ultrasound may help clinicians to perform an early diagnosis and evaluation of the therapeutic effect of lupus miliaris disseminatus faciei. However, further studies are needed to better characterize the dermatoscopic and ultrasonic variations of lupus miliaris disseminatus faciei.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There is no conflict of interest.
References
- Lupus miliaris disseminatus faciei: a distinctive facial granulomatous eruption. BMJ Case Rep 2017 bcr-2017-221118
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermatoscopic evaluation of two patients with lupus miliaris disseminatus faciei. Clin Exp Dermatol. 2014;39:500-2.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopy of granulomatous disorders. Dermatol Clin. 2018;36:369-75.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound findings in idiopathic facial aseptic granuloma: Case series and literature review. Pediatr Dermatol. 2018;35:397-400.
- [CrossRef] [PubMed] [Google Scholar]






