Translate this page into:
Dermatoscopic features of incontinentia pigmenti
Correspondence Address:
Keshavamurthy Vinay
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 012
India
| How to cite this article: Bishnoi A, Kumaran SM, Vinay K. Dermatoscopic features of incontinentia pigmenti. Indian J Dermatol Venereol Leprol 2020;86:422-424 |
Sir,
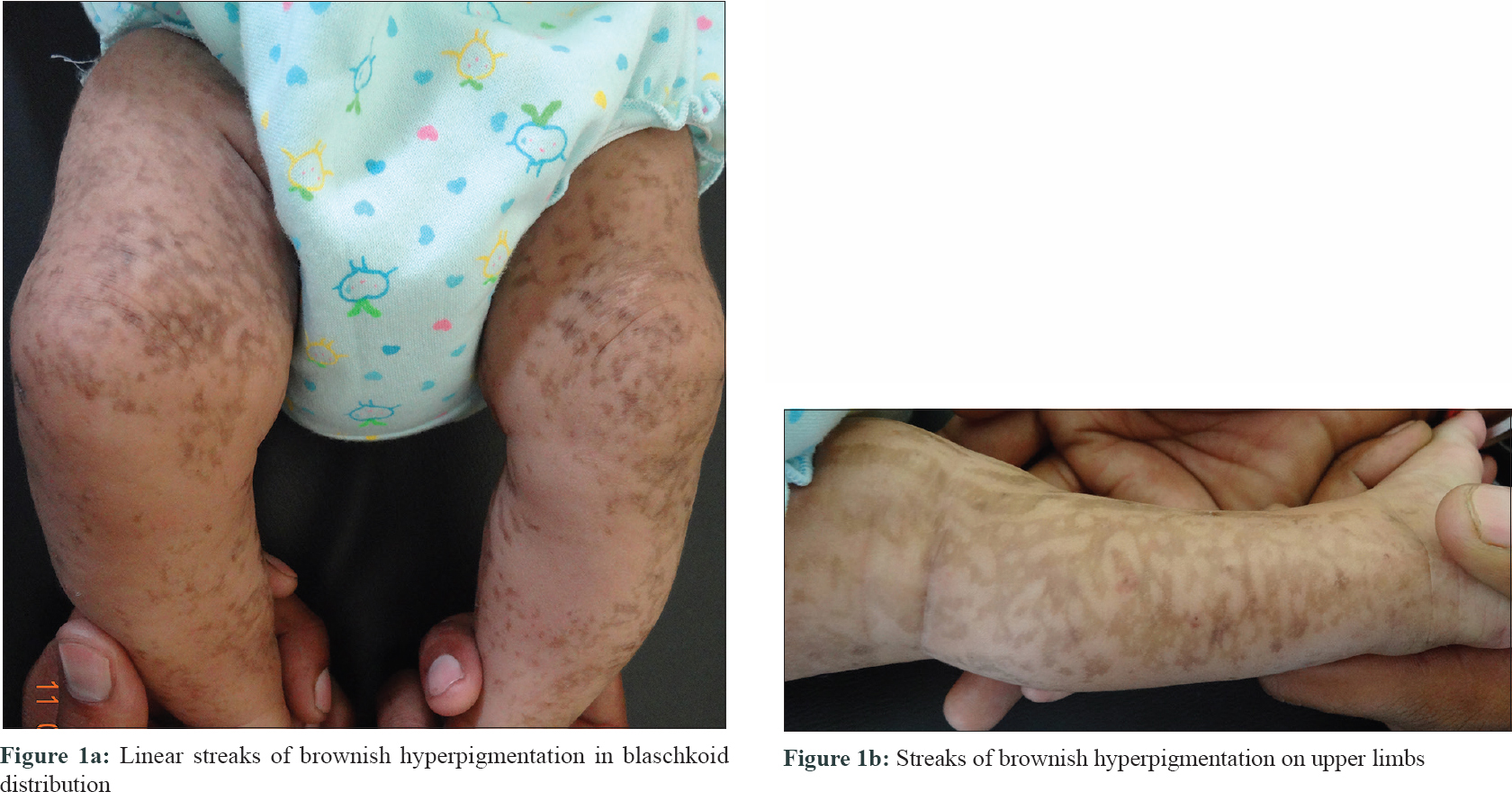
Dermatology consultation was sought by the parents of a 1-month-old Indian girl, born out of a non-consanguineous marriage, for pigmented lesions on her body, which they had noticed since birth. Examination revealed linear streaks of brownish hyperpigmentation on the trunk and limbs with a striking blaschkoid distribution and showing mild atrophy on lower limbs [Figure - 1]a and [Figure - 1]b. Small hyperkeratotic plaques of around 1 cm, which were preceded by bullous lesions at birth, were present on thumbs. Ocular examination revealed no abnormalities. Scalp hair was normal in both mother and the infant. A diagnosis of incontinentia pigmenti was strongly considered.
 |
| Figure 1: |
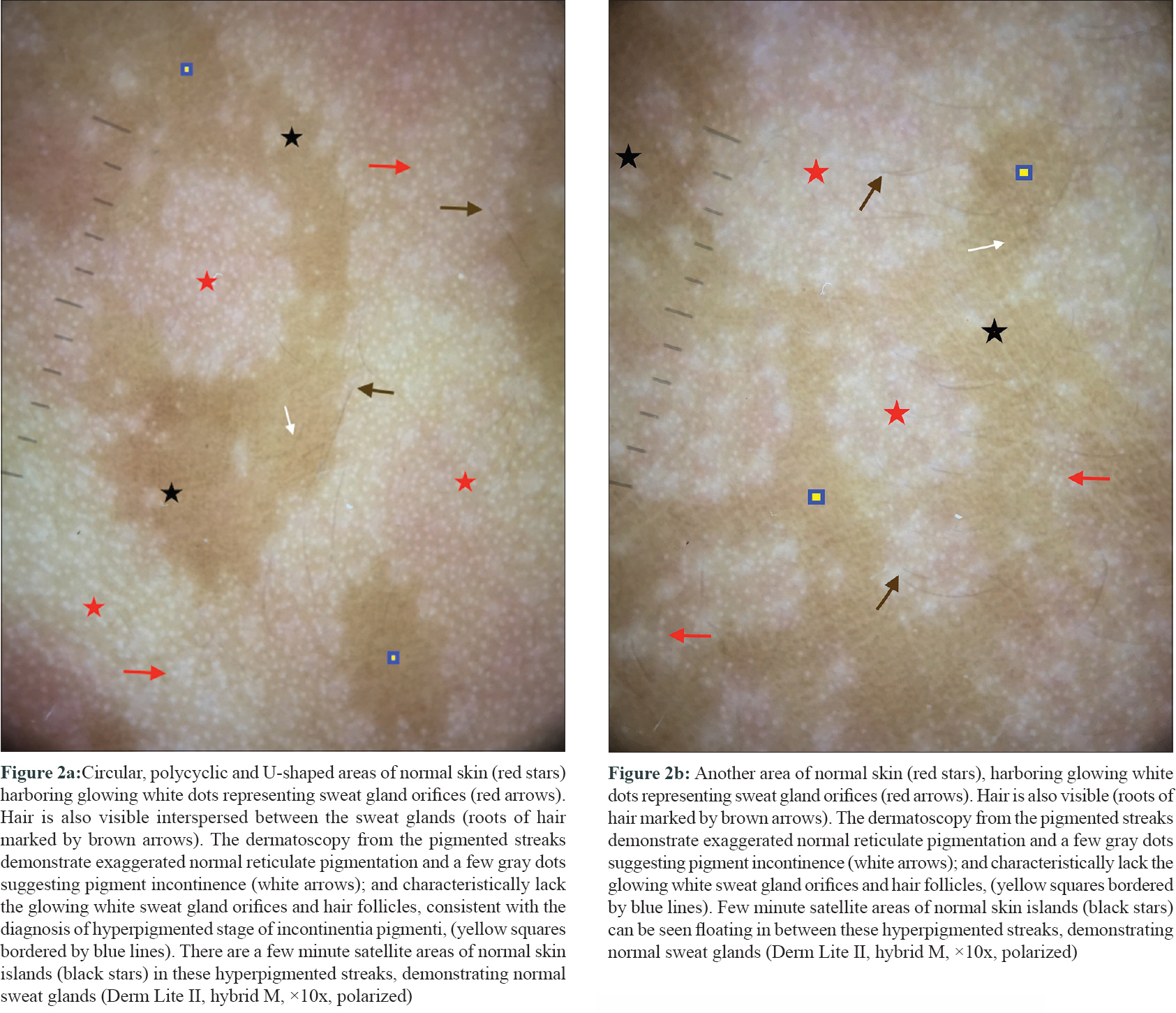
Parents were counselled regarding the need for performing a skin biopsy. Since genetic testing was planned simultaneously, they agreed for the latter; the biopsy was deferred because of its invasive nature. Dermatoscopic examination was performed on an area having both normal skin and hyperpigmented streaks using a Dermlite II hybrid M dermatoscope at 10 × magnification in polarized noncontact mode and photographs were captured with the help of Dermlite app using Apple Iphone 6 plus. The dermatoscopy from the hyperpigmented streaks characteristically lacked sweat gland orifices (visible as glowing white dots in normal skin) and hair follicles, and demonstrated a few gray dots suggestive of pigment incontinence; consistent with the diagnosis of hyperpigmented stage of incontinentia pigmenti [Figure - 2]a and [Figure - 2]b.
 |
| Figure 2: |
Investigations revealed peripheral eosinophilia (absolute eosinophil count 5400) and a mutation study of the blood sample revealed mutation in nuclear factor κB essential modulator (NEMO) gene confirming the diagnosis of incontinentia pigmenti.
Incontinentia pigmenti is an X-linked dominant genodermatosis that characteristically presents in female infants with typical skin lesions in blaschkoid distribution, a pattern followed by migrating keratinocytes during embryogenesis. Four types of lesions have been described: vesicular, hyperkeratotic, hyperpigmented and hypopigmented.[1] Vesicular lesions reveal histopathological changes typical of incontinentia pigmenti including eosinophilic spongiosis and dyskeratosis. Hyperkeratotic lesions usually follow vesiculobullous lesions and subside in a few initial months of life.[1]
Sometimes the initial stages of incontinentia pigmenti occur and subside during intrauterine life, and hyperpigmented lesions in a blaschkoid pattern present at birth. Though atrophy is usually apparent in hyperpigmented stages of incontinentia pigmenti, histopathological evidence in the form of loss of pilosebaceous and sudomotor appendages is more readily demonstrated in hypopigmented lesions. But, a similar histopathological finding has also been noted in hyperpigmented streaks (stage 3).[2] Our dermatoscopic findings in the form of readily apparent loss of sweat gland orifices and hair, on hyperpigmented streaks, correlated well with histopathological findings noted in a previous study.[2]
Linear and whorled hypermelanosis is an important clinical differential of hyperpigmented stage of IP. The dermatoscopic features have been previously published and demonstrate small hyperpigmented circles/rings, and curved and parallel pigmented streaks.[3],[4] Reticulate pigmentation was also described in one report.[5] Unlike dermatoscopy of incontinentia pigmenti, hypopigmented dots corresponding to perifollicular areas and sweat gland openings are present in both whorled and linear lesions. Since dermatoscopic features of incontinentia pigmenti have not been reported yet, our findings could help differentiate it from linear and whorled hypermelanosis in forthcoming cases.
To conclude, these dermatoscopic findings should be actively looked for in a neonate/infant presenting with streaky hyperpigmentation and may preclude the need for an invasive procedure like skin biopsy, especially in the later stages of the incontinentia pigmenti.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that name and initial of the child will not be published, and due efforts will be made to conceal patient identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Poziomczyk CS, Recuero JK, Bringhenti L, Maria FD, Campos CW, Travi GM, et al. Incontinentia pigmenti. An Bras Dermatol 2014;89:26-36.
[Google Scholar]
|
| 2. |
Hadj-Rabia S, Rimella A, Smahi A, Fraitag S, Hamel-Teillac D, Bonnefont JP, et al. Clinical and histologic features of incontinentia pigmenti in adults with nuclear factor-κB essential modulator gene mutations. J Am Acad Dermatol 2011;64:508-15.
[Google Scholar]
|
| 3. |
Ertam I, Turk BG, Urkmez A, Kazandi A, Ozdemir F. Linear and whorled nevoid hypermelanosis: Dermatoscopic features. J Am Acad Dermatol 2009;60:328-31.
[Google Scholar]
|
| 4. |
Errichetti E, Pegolo E, Stinco G. Linear and whorled nevoid hypermelanosis: A case report with dermoscopic findings. Indian J Dermatol Venereol Leprol 2016;82:91-3.
[Google Scholar]
|
| 5. |
Naveen KN, Reshme P. Linear and whorled nevoid hypermelanosis with dermatoscopic features. Dermatol Online J 2014;20. pii: doj_21760.
[Google Scholar]
|
Fulltext Views
5,120
PDF downloads
2,767





