Translate this page into:
Dermoscopic evaluation of cutaneous histoplasmosis
Corresponding author: Dr. Sendhil Kumaran, Department of Dermatology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. mrbangga@catholic.ac.kr
-
Received: ,
Accepted: ,
How to cite this article: Mustari AP, Rao S, Keshavamurthy V, Chatterjee D, Kumaran S. Dermoscopic evaluation of cutaneous histoplasmosis. Indian J Dermatol Venereol Leprol. 2025;91:231-4. doi: 10.25259/IJDVL_889_2022
Dear Editor,
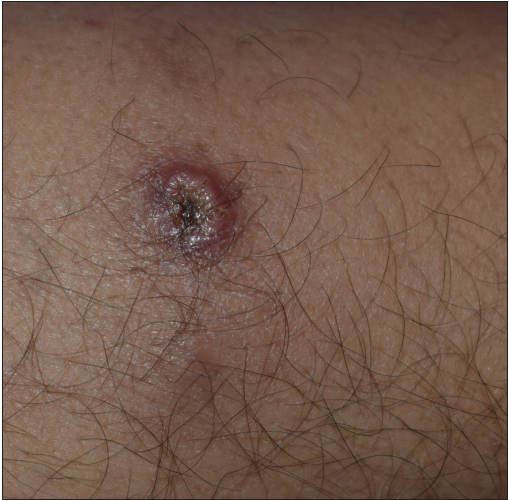
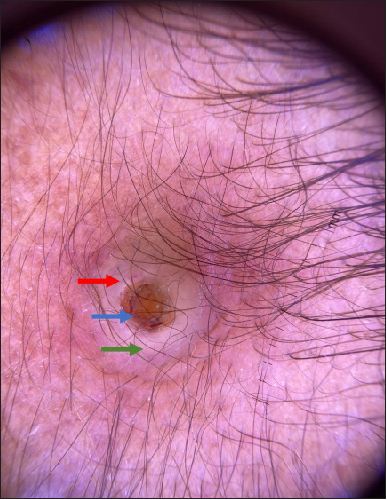
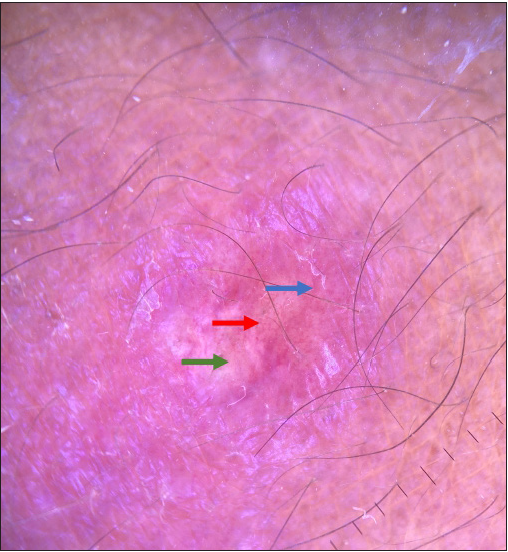
A 46-year-old female homemaker, who underwent a renal transplant five years back, presented with asymptomatic erythematous plaques over her face, forearm, and legs for three months. The lesions started as erythematous papules, gradually progressing to umbilicated plaques with crusting. The patient had received anti-thymocyte globulin (ATG) induction and was on mycophenolate mofetil 360 mg twice daily and prednisolone 7.5 mg once daily as maintenance immunosuppression. There was no cough, breathlessness, hepatosplenomegaly, lymphadenopathy, or mucosal lesions. Serum urea was 67 mg/dl, creatinine was 2.2 mg/dl, and chest radiography was normal. Clinical examination revealed multiple erythematous umbilicated papules and plaques measuring 1–2 cm with central brown-black necrotic slough and perilesional erythema over the temporal area, forearms, and legs [Figures 1a to 1c]. A dermoscopic evaluation was done using DermLite™ DL3 (3Gen, San Juan Capistrano, CA, USA) at 10x magnification in polarised mode. Dermoscopy from umbilicated papules showed a central yellowish crateriform plug with a surrounding rim of the yellow-white area containing ill-focused vessels focally [Figure 1d]. Dermoscopy of the erythematous nodules showed central yellow-white areas containing irregular vessels with surrounding erythema and scaling [Figure 1e], and that of the crusted plaque showed central brown crusting with surrounding yellowish-white structureless areas with irregular outer border, erythema and scaling [Figure 1f]. Skin biopsy demonstrated atrophic epidermis, diffuse dermal infiltrate of lymphocyte, histiocyte, foamy histiocyte, and multinucleate giant cells containing multiple yeasts, with surrounding halo highlighted by the Grocott and periodic acid stain [Figure 2a–2c]. Based on clinical, dermoscopic, and histopathological features, a final diagnosis of cutaneous histoplasmosis was arrived at made. The patient was started on liposomal amphotericin B (5 mg/kg) for 14 days, followed by oral itraconazole 200 mg (twice a day). After 6 weeks, there was complete healing of the lesions.

- Umbilicated papule over the left temporal area.
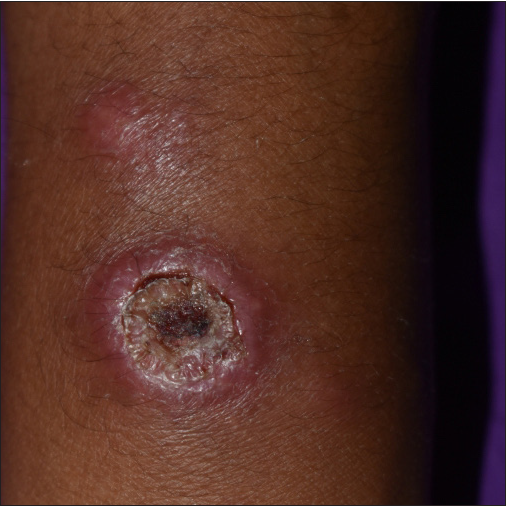
- Erythematous nodule over the left forearm.
- Umbilicated crusted plaque over the left leg.
- Dermoscopy of the crusted papule showing central yellowish keratotic plug (blue arrow) with surrounding yellow-white rim (green arrow) containing ill-focused vessel focally (red arrow) (Polarised mode, 10x).
- Dermoscopy of erythematous nodule showing irregular vessel (red arrow) on a yellow background (green arrow) with surrounding erythema and scaling (blue arrow) (Polarised mode, 10x).
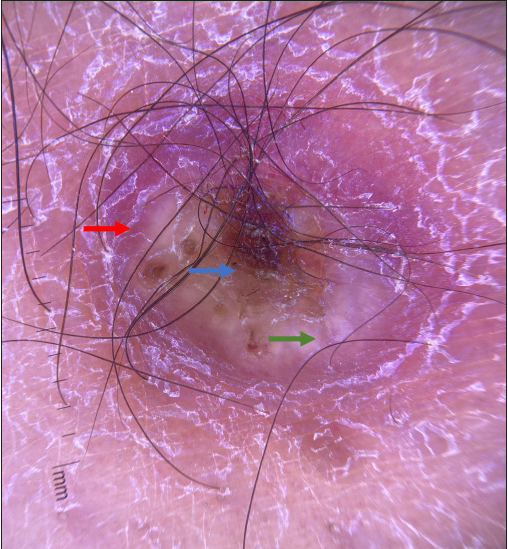
- Dermoscopy of the crusted plaque showing central brown crusting (blue arrow) with surrounding yellow-white structureless area (green arrow), erythema and scaling (red arrow). (Polarised mode, 10x).
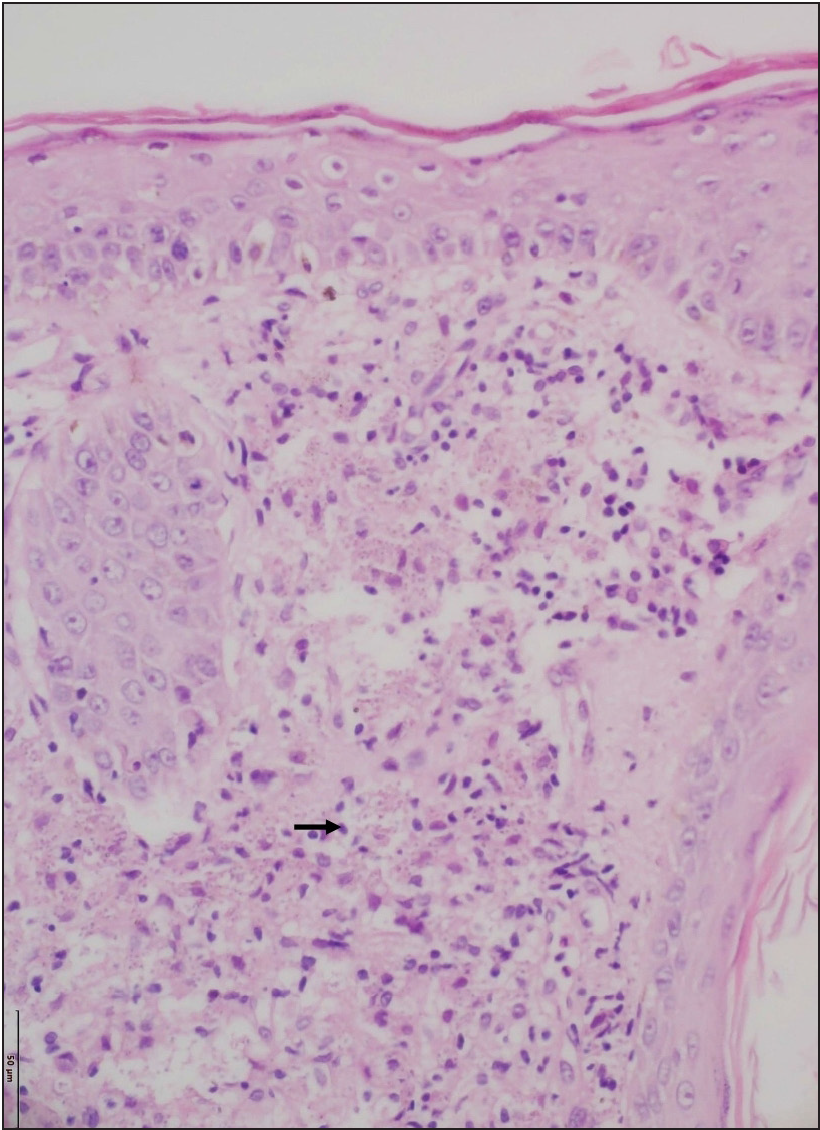
- Skin biopsy shows the presence of numerous histiocytes with abundant foamy cytoplasm in the dermis (black arrow) (Haematoxylin and eosin, 200x).
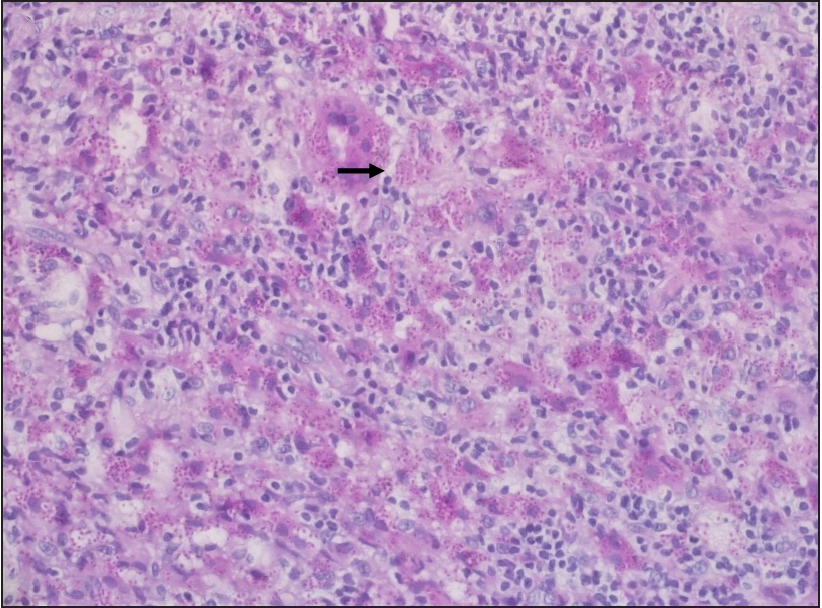
- Many intracytoplasmic fungal spores are highlighted by Periodic acid-stain (black arrow) (200x).
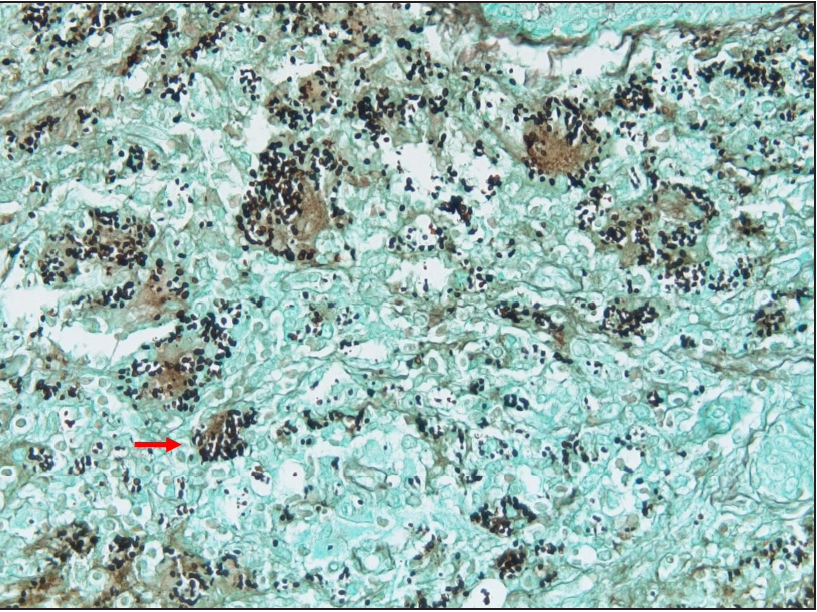
- Many intracytoplasmic fungal spores are highlighted by Grocott stain showing (red arrow) (200x).
Histoplasmosis, or Darling’s Disease, is a fungal infection caused by Histoplasma capsulatum, commonly found in soil contaminated with bird droppings. Risk factors include HIV (human immunodeficiency virus) infection with CD4 count 100 cells/µL, post-organ transplant, and chemotherapy. Clinical variants include acute pulmonary, acute disseminated, chronic pulmonary, chronic disseminated, and primary cutaneous histoplasmosis. The route of infection is through direct inoculation of spores from contaminated soil. Primary cutaneous histoplasmosis is rare and presents as asymptomatic erythematous, crusted papules and plaques, pustules, nodules, molluscum-like, wart-like-plaques, pyoderma gangrenosum like ulcers, erythema nodosum like lesions and palatal perforation. Early diagnosis is important to prevent systemic involvement as disseminated histoplasmosis is associated with a poor prognosis. Histopathologically, histoplasmosis is characterized by diffuse dermal suppurative granulomas composed of histiocyte, foamy histiocyte, and multinucleated giant cell with intra and extracellular yeasts (1–5 µm) with clear surrounding halo, which can be highlighted (black) by Grocott’s methenamine silver stain.1
The common differential diagnosis of umbilicated crusted plaques over the face and extremities include histoplasmosis, cryptococcosis, and penicilliosis, which are often difficult to differentiate clinically. Histoplasmosis, cryptococcosis, and penicilliosis are seen in immunocompromised individuals, have overlapping features clinically, and show suppurative granuloma on histopathology, making diagnosis challenging. Cryptococcosis is a fungal infection caused by Cryptococcus neoformans; the presence of large (4–15 µm) spores, thick mucinous capsules, and narrow-based budding differentiate it from histoplasmosis.2 Pencilliosis is a fungal infection caused by Talaromyces marneffei, characterized by sausage-shaped thin-walled yeast-like cells divided by septum, which is absent in histoplasmosis.3
There is paucity of data on dermoscopic features in the above conditions, and the literature is limited to isolated case reports. To the best of our knowledge, dermoscopic features of histoplasmosis have been reported in a single case report, which showed arborizing vessels and superficial scaling.4 Dermoscopy in index case showed yellowish-white areas, which represents a dermal granuloma; irregular vessels are due to neoangiogenesis, erythema is due to inflammation and vasodilation, and brown crusting and scaling correspond to areas of necrosis. Cryptococcosis also shows yellow-white areas with serpentine and linear irregular vessels.5 Penicilliosis shows the central necrotic area with surrounding irregular vessels.6 All the infective fungal granulomatous diseases show central crusting with yellow-white areas and polymorphic vessels dermoscopically, but central crusting with keratotic plug appears to differentiate them from non-infectious granulomatous dermatoses. Further studies with a larger sample size are required to confirm these findings.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Disseminated cutaneous histoplasmosis, an initial manifestation of HIV, diagnosed with fine needle aspiration cytology. Indian J Dermatol. 2014;59:182-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Rare presentation of cutaneous cryptococcosis in advanced HIV. BMJ Case Rep. 2018;11:bcr2018227247.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- [A case of disseminated Penicillium marneffei infection in a liver transplant recipient] Korean J Lab Med. 2010;30:400-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous histoplasmosis as a complication after anti-TNF use – Case report. An Bras Dermatol. 2015;90:104-7.
- [Google Scholar]
- Dermoscopic observations in disseminated cryptococcosis with cutaneous involvement. J Eur Acad Dermatol Venereol. 2018;32:223-4.
- [Google Scholar]
- Dermoscopic manifestations of Talaromyces (Penicillium) marneffei infection in an AIDS patient. Indian J Dermatol Venereol Leprol. 2019;85:348.
- [Google Scholar]





