Translate this page into:
Dermoscopic features of three cases of Langerhans cell histiocytosis
2 Department of Pathology, Venereology and Leprology, JIPMER, Puducherry, India
Correspondence Address:
Munisamy Malathi
Department of Dermatology, Venereology and Leprology, JIPMER, Puducherry - 605 006
India
| How to cite this article: Behera B, Malathi M, Thappa DM, Gochhait D, Srinivas BH, Toi PC. Dermoscopic features of three cases of Langerhans cell histiocytosis. Indian J Dermatol Venereol Leprol 2018;84:730-735 |
Sir,
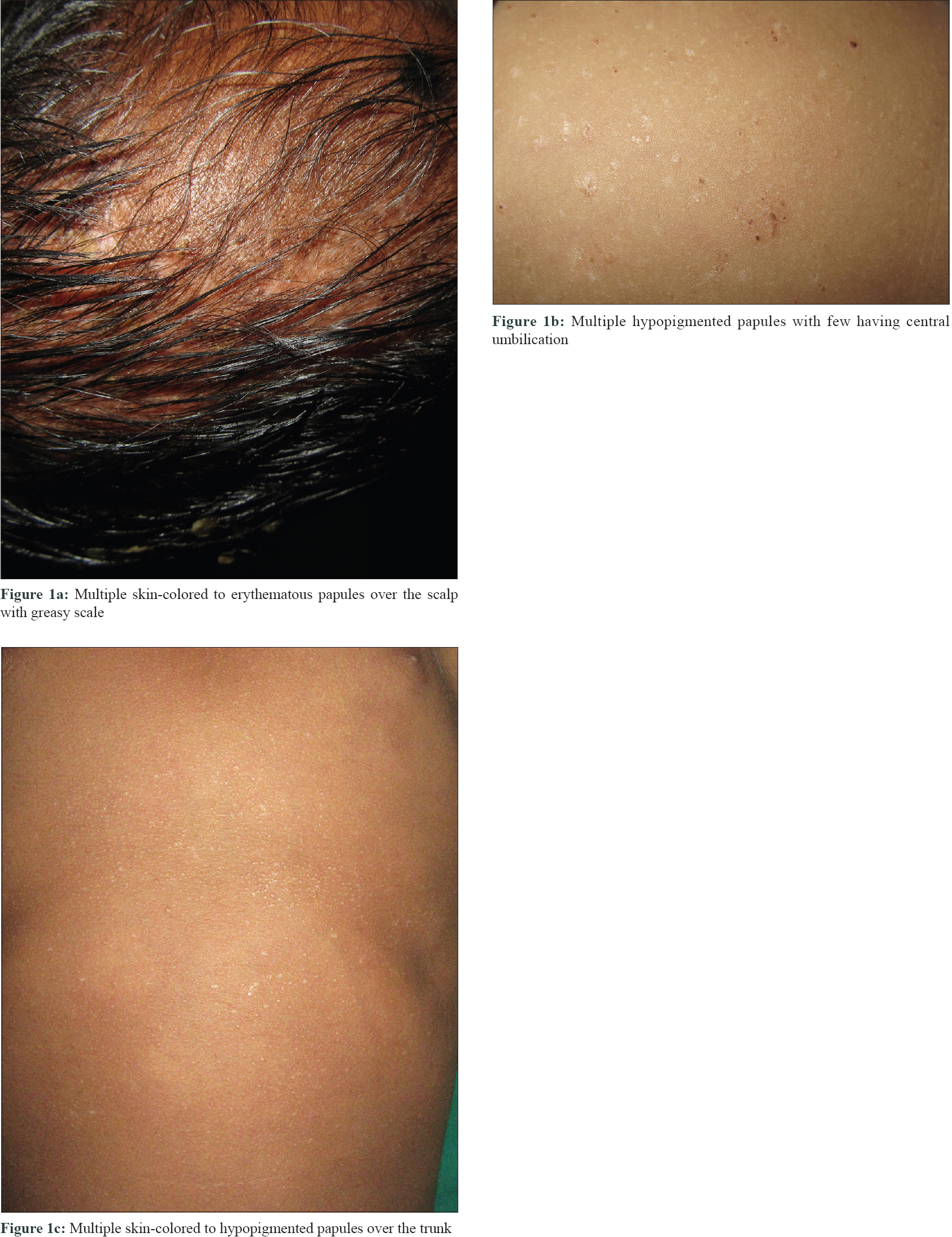
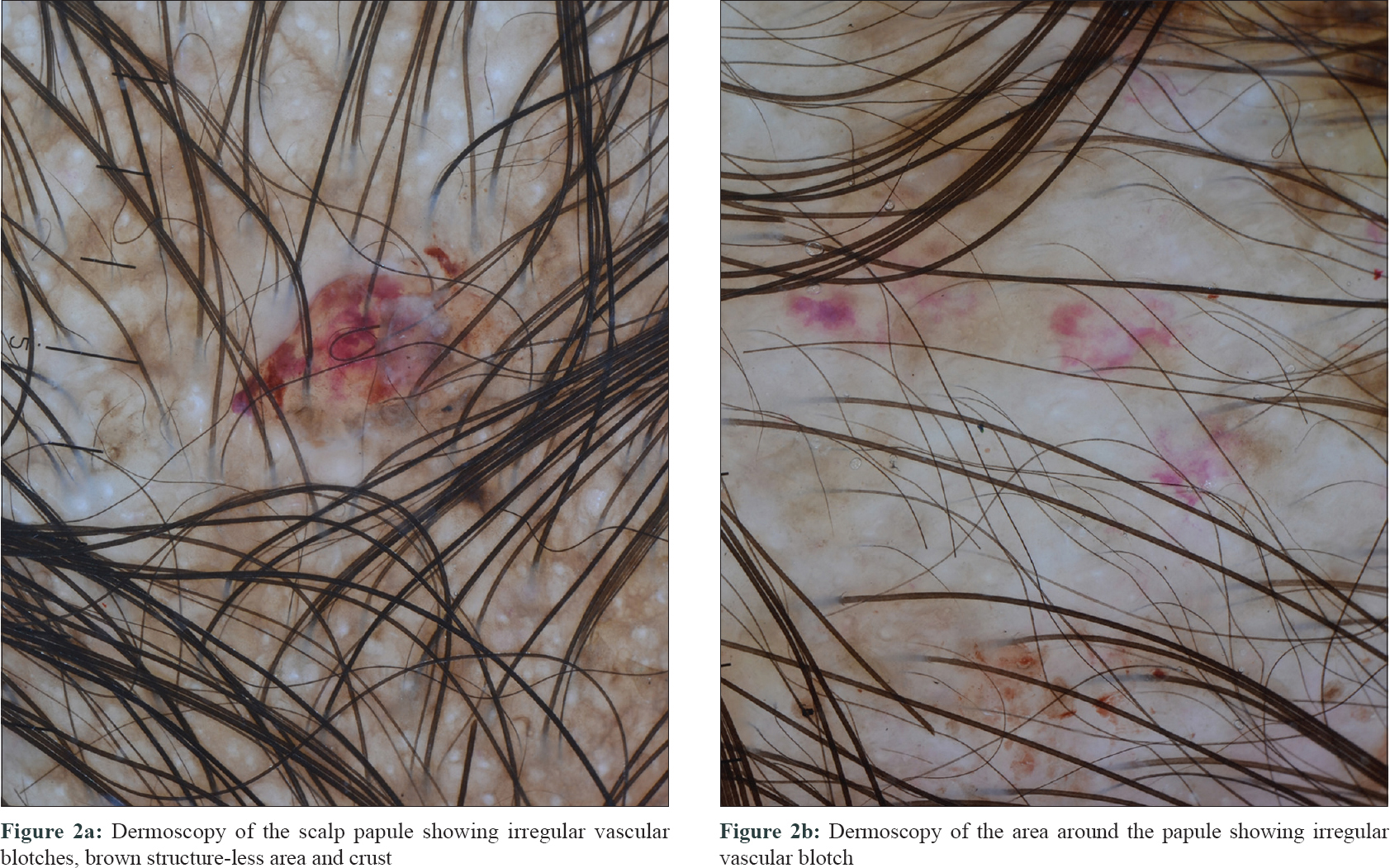
The first case was a 10-month-old male child who was brought by his parents with complaints of scalp scaling of 2 months duration associated with fever. Cutaneous examination revealed multiple skin-colored to erythematous papules with greasy scales all over the scalp [Figure - 1]a. Other cutaneous and mucosal examination was within normal limits. Dermoscopic examination (HEINE DELTA20® Dermatoscope, 10 × magnification) under nonpolarized contact dermoscopy revealed irregular vascular blotches and brown structure-less area and crust [Figure - 2].
 |
| Figure 1: |
 |
| Figure 2: |
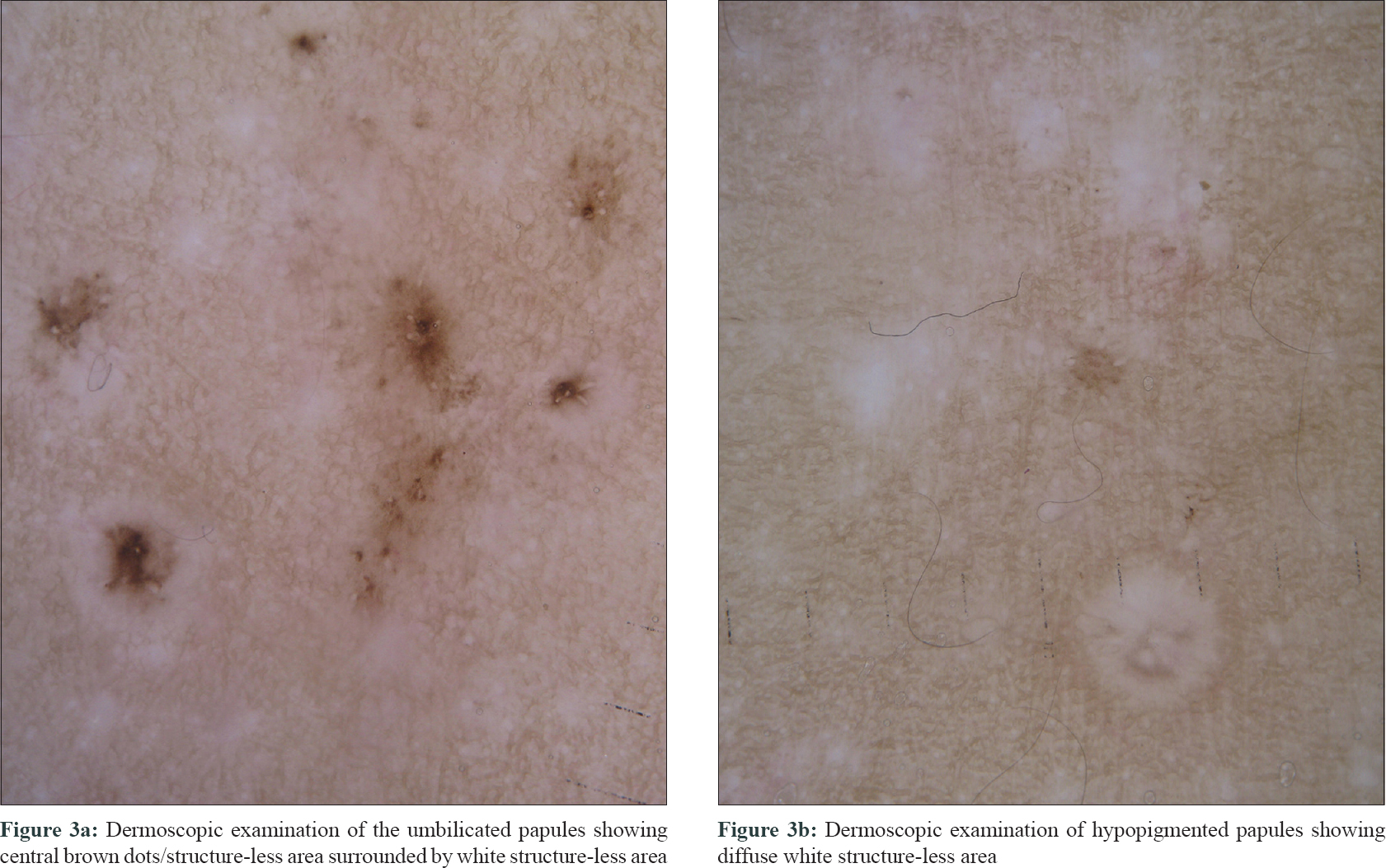
The second case was a 14-month-old male child who presented with asymptomatic skin rash over the face and trunk of 6 months duration. Cutaneous examination revealed multiple hypopigmented papules, few with central umbilication distributed over the face and trunk [Figure - 1]b. The umbilicated papules under nonpolarized contact dermoscopy (10x magnification) showed central brown dots, and structure-less area surrounded by white structureless area and the hypopigmented papules showed diffuse white structure-less area [Figure - 3].
 |
| Figure 3: |
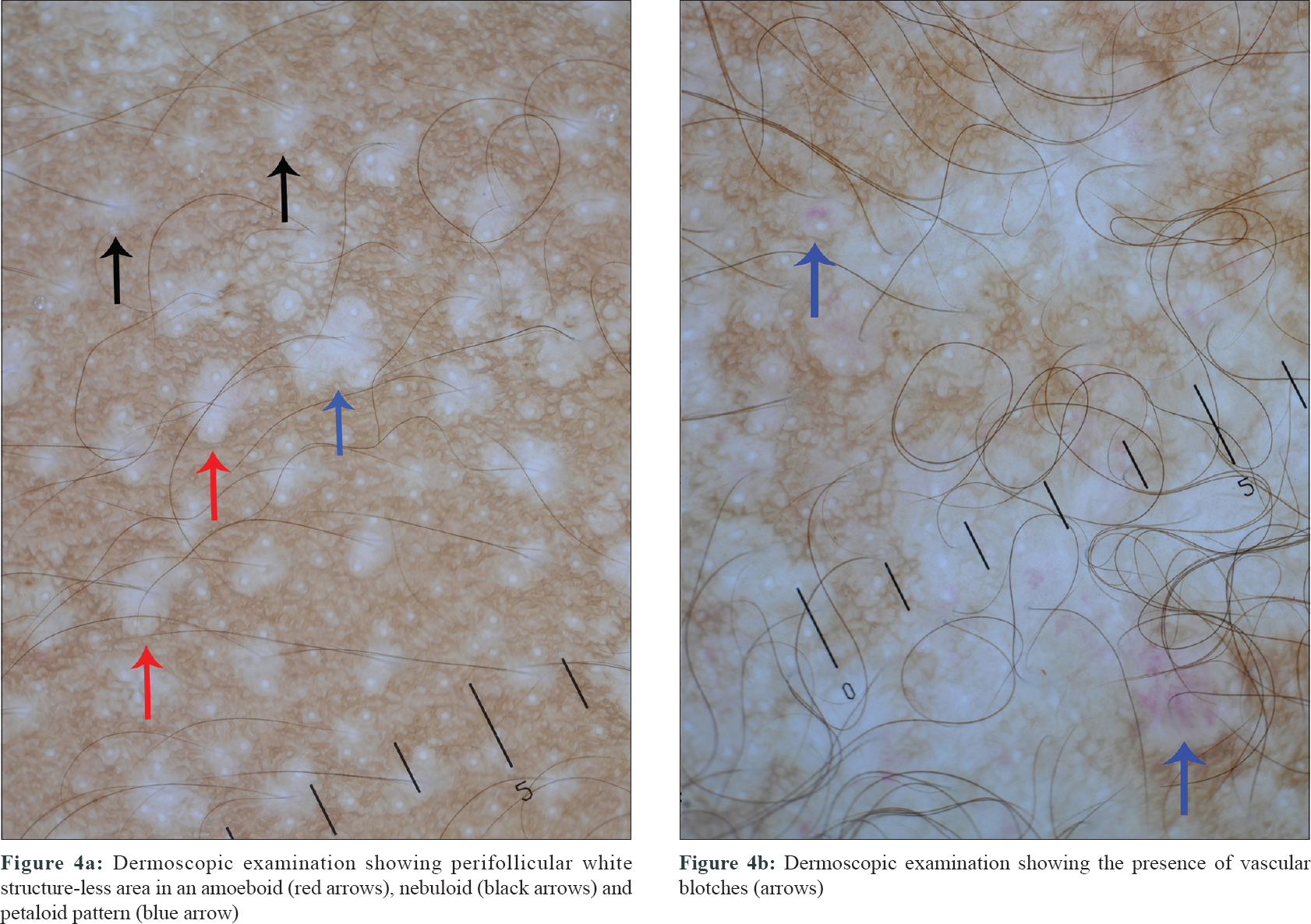
Case 3 was a 1-year-old male child who presented with history of asymptomatic skin rash over the trunk of 4 months duration. It was associated with swelling over the frontal scalp and loss of appetite. Cutaneous examination revealed multiple skin-colored to hypopigmented papules of size ranging from 1 mm × 1 mm to 3 mm × 3 mm over the anterior and posterior aspect of the trunk [Figure - 1]c. Under nonpolarized contact dermoscopy (10x magnification) the papules revealed perifollicular white homogenous areas in amoeboid (amoeba-like pseudopods extending at the periphery), nebuloid (indistinct margins, merging into surrounding skin) and petaloid pattern (well-defined borders) [Figure - 4]a[1]. At places, the white homogenous areas coalesced to form an irregular geographic pattern. Few papules demonstrated vascular blotches [arrows, [Figure - 4]b.
 |
| Figure 4: |
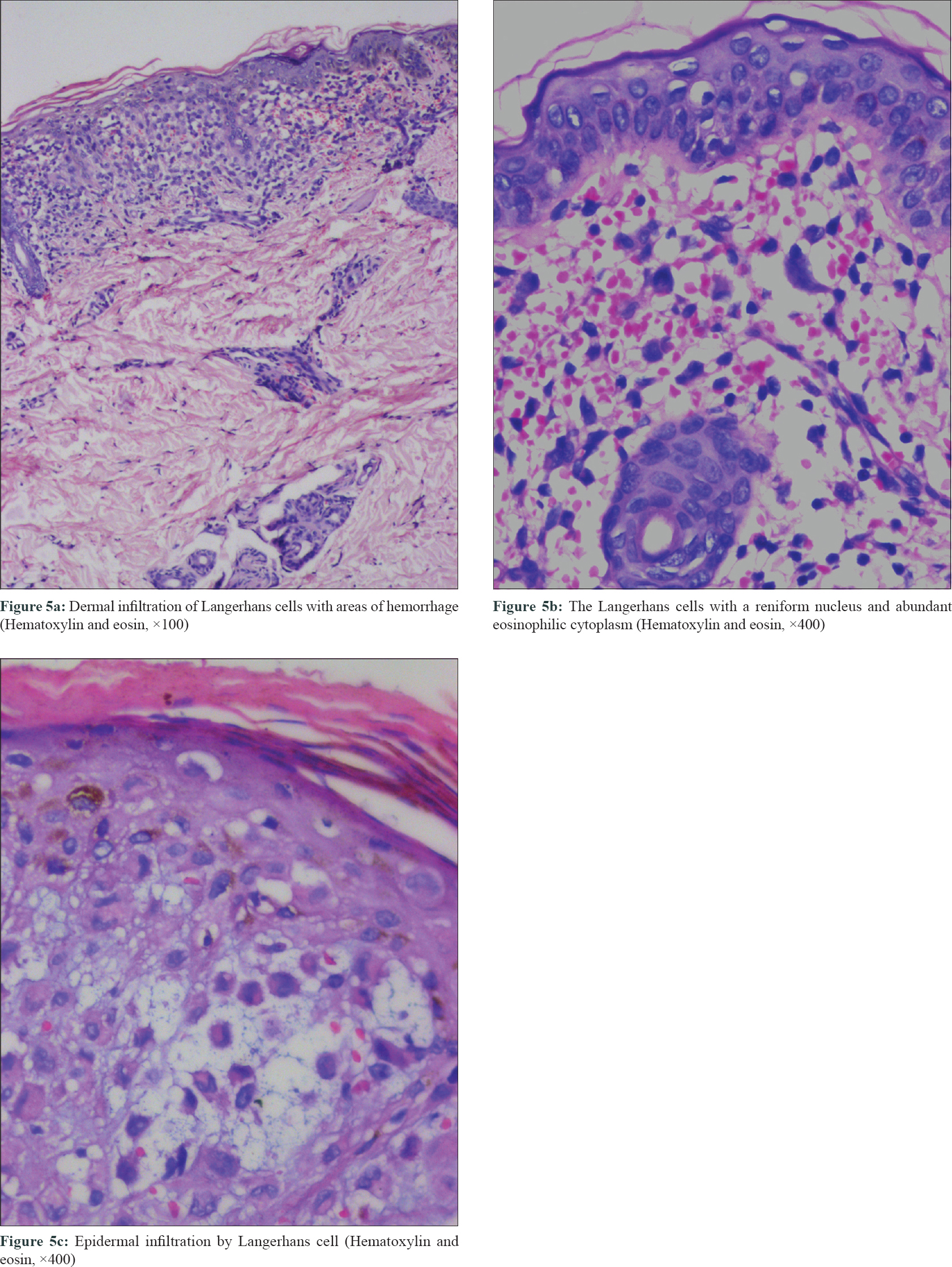
In all cases, a systemic work-up was done, and histopathological examination of the skin biopsy showed dermal infiltration of histiocytes with a reniform nucleus and abundant eosinophilic cytoplasm consistent with a diagnosis of Langerhans cell histiocytosis, which was confirmed by positive S100 and CD1a and negative CD68 immunostaining [Figure - 5]a, [Figure - 5]b, [Figure - 5]c.
 |
| Figure 5: |
Langerhans cell histiocytosis is a rare proliferative Langerhans cell disorder of unknown etiology. Cutaneous presentation of Langerhans cell histiocytosis can have a diverse morphological presentation that includes papules, pustules, vesicles, nodules, petechiae and ulcers. The clinical morphology of Langerhans cell histiocytosis can mimic inflammatory dermatosis such as seborrheic dermatitis to malignant condition such as leukemia cutis. Consequently, the diagnosis and treatment of the condition is delayed.[2] Out of the three cases described by us, the first case had only scalp involvement and the second and third cases had only cutaneous involvement but with different morphology.
Dermoscopy is a simple, rapid, noninvasive outpatient procedure that unfolds the diagnosis of a particular dermatosis by giving a certain subtle clue, thus alleviating the need for biopsy. The data regarding the dermoscopic features of Langerhans cell histiocytosis is very scanty and includes widespread red-blue lacunes of different sizes, reddish-purple areas and brown dots and central white area with peripheral telangiectasia.[2],[3],[4] The dermoscopic features of various dermatological conditions that were considered in the differential diagnosis of each of our cases are delineated in [Table - 1].
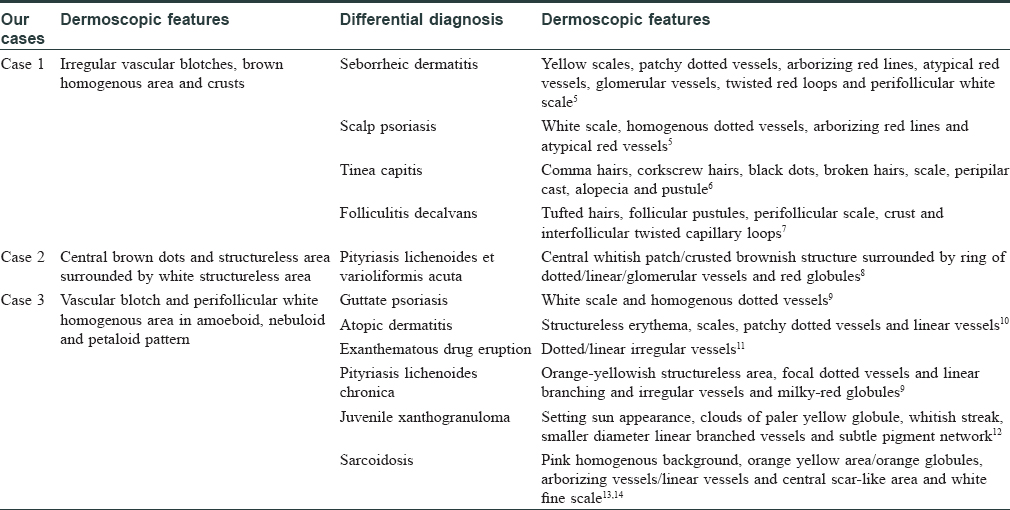
The dermoscopic features that may help in differentiating Langerhans cell histiocytosis involving the scalp from the scalp seborrheic dermatitis and scalp psoriasis are the presence of vascular blotch, brown homogenous area/crust and the absence of dotted and nondotted vessels.[5] The vascular blotch clinically corresponds to the purpuric tinges associated with the lesion. Interestingly, the papules in the third case were not clinically associated with any purpuric tinges, but few of them demonstrated vascular blotch under the dermoscope (blue arrows, [Figure - 4]b), which suggests that dermoscopy can be useful in unveiling the subclinical hemorrhages that cannot be appreciated by the naked eye. The presence of a white structure-less area and absence of a yellow structure which corresponds to the infiltration of xanthomized histiocytes can be an important clue in differentiating Langerhans cell histiocytosis from non-Langerhans cell histiocytic disorders such as juvenile xanthogranuloma, benign cephalic histiocytosis and reticulohistiocytosis.[12]
Analyzing the dermoscopic features of previously reported cases and our present cases, the presence of vascular blotch seems to be a common dermoscopic finding. The cases reported by Rubio-González et al.[2] and Murata et al.[4] demonstrates vascular blotch in the dermoscopic images, although they have not mentioned the same in the text. The vascular blotch present under dermoscopy histologically corresponds to dermal hemorrhage [Figure - 5]b; the white homogenous area corresponds to the dermal Langerhans cell infiltration without epidermal involvement and brown dots/structure-less area/crust to the epidermal infiltration and necrosis by Langerhans cells.
In conclusion, Langerhans cell histiocytosis, similar to its clinical presentation, can have diverse dermoscopic features. In this report, we are describing various dermoscopic features in three cases of Langerhans cell histiocytosis, and we hope that further studies on a larger case series will be helpful in revealing additional dermoscopic features and diagnostic clues.[14]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardians have given their consent for images and other clinical information to be reported in the journal. The guardians understand that names and initials will not be published and due efforts will be made to conceal patient identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ankad BS, Beergouder SL. Dermoscopic evaluation of idiopathic guttate hypomelanosis: A preliminary observation. Indian Dermatol Online J 2015;6:164-7.
[Google Scholar]
|
| 2. |
Rubio-González B, García-Bracamonte B, Ortiz-Romero PL, Postigo-Llorente C, Vanaclocha-Sebastián F. Multisystemic Langerhans cell histiocytosis mimicking diffuse neonatal hemangiomatosis. Pediatr Dermatol 2014;31:e87-9.
[Google Scholar]
|
| 3. |
Behera B, Malathi M, Prabhakaran N, Divya K, Thappa DM, Srinivas BH. Dermoscopy of Langerhans cell histiocytosis. J Am Acad Dermatol 2017;76:S79-81.
[Google Scholar]
|
| 4. |
Murata S, Yoshida Y, Adachi K, Morita E, Yamamoto O. Solitary, late-onset, self-healing Langerhans cell histiocytosis. Acta Derm Venereol 2011;91:103-4.
[Google Scholar]
|
| 5. |
Kim GW, Jung HJ, Ko HC, Kim MB, Lee WJ, Lee SJ, et al. Dermoscopy can be useful in differentiating scalp psoriasis from seborrhoeic dermatitis. Br J Dermatol 2011;164:652-6.
[Google Scholar]
|
| 6. |
Arrazola-Guerrero J, Isa-Isa R, Torres-Guerrero E, Arenas R. Tinea capitis. Dermoscopic findings in 37 patients. Rev Iberoam Micol 2015;32:242-6.
[Google Scholar]
|
| 7. |
Jain N, Doshi B, Khopkar U. Trichoscopy in alopecias: Diagnosis simplified. Int J Trichology 2013;5:170-8.
[Google Scholar]
|
| 8. |
Lacarrubba F, Micali G. Dermoscopy of pityriasis lichenoides et varioliformis acuta. Arch Dermatol 2010;146:1322.
[Google Scholar]
|
| 9. |
Errichetti E, Lacarrubba F, Micali G, Piccirillo A, Stinco G. Differentiation of pityriasis lichenoides chronica from guttate psoriasis by dermoscopy. Clin Exp Dermatol 2015;40:804-6.
[Google Scholar]
|
| 10. |
Luk DC, Lam SY, Cheung PC, Chan BH. Dermoscopy for common skin problems in Chinese children using a novel Hong Kong-made dermoscope. Hong Kong Med J 2014;20:495-503.
[Google Scholar]
|
| 11. |
Errichetti E, Pegolo E, Stinco G. Dermoscopy as an auxiliary tool in the early differential diagnosis of acute generalized exanthematous pustulosis (AGEP) and exanthematous (morbilliform) drug eruption. J Am Acad Dermatol 2016;74:e29-31.
[Google Scholar]
|
| 12. |
Song M, Kim SH, Jung DS, Ko HC, Kwon KS, Kim MB. Structural correlations between dermoscopic and histopathological features of juvenile xanthogranuloma. J Eur Acad Dermatol Venereol 2011;25:259-63.
[Google Scholar]
|
| 13. |
Pellicano R, Tiodorovic-Zivkovic D, Gourhant JY, Catricalà C, Ferrara G, Caldarola G. Dermoscopy of cutaneous sarcoidosis. Dermatology 2010;221:51-4.
[Google Scholar]
|
| 14. |
Ramadan S, Hossam D, Saleh MA. Dermoscopy could be useful in differentiating sarcoidosis from necrobiotic granulomas even after treatment with systemic steroids. Dermatol Pract Concept 2016;6:17-22.
[Google Scholar]
|
Fulltext Views
4,065
PDF downloads
1,635





