Translate this page into:
Dermoscopic findings of de novo syringocystadenoma papilliferum
Corresponding author: Dr. Biswanath Behera, Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar - 751 019, Odisha, India. biswanathbehera61@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dash S, Nayak AK, Sethy M, Palit A, Behera B. Dermoscopic findings of a de novo syringocystadenoma papilliferum. Indian J Dermatol Venereol Leprol 2021;87:278-80.
Sir,
Syringocystadenoma papilliferum is an uncommon, benign, hamartomatous adnexal tumor arising from pluripotent cells. The histology can exhibit either apocrine or eccrine differentiation. Although commonly associated with other benign adnexal tumours like sebaceous nevus, it can also occur de novo.1
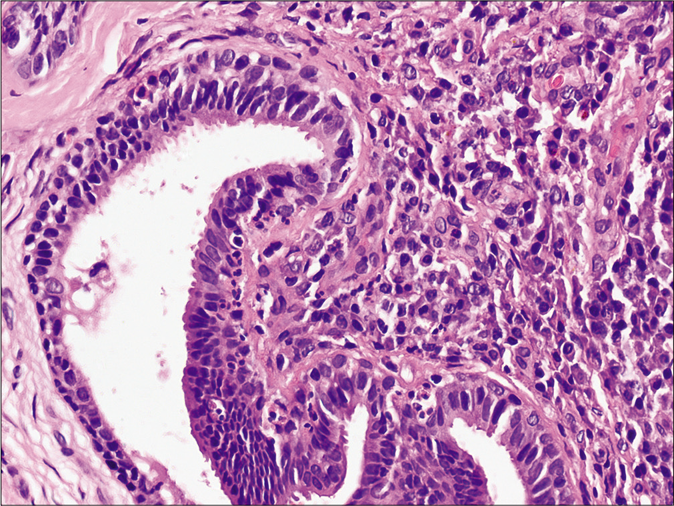
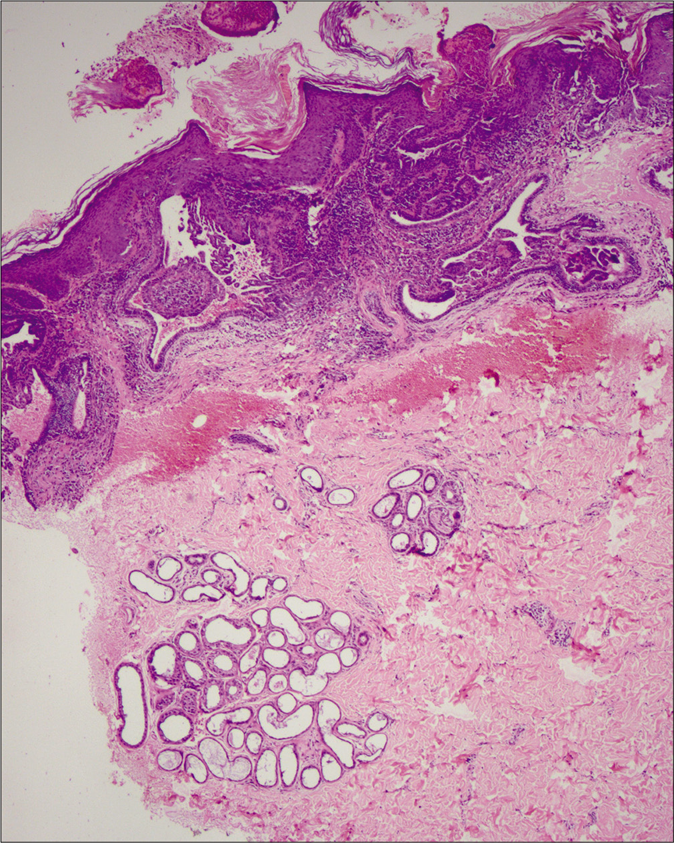
A 7-year-old healthy boy presented with multiple asymptomatic skin-colored, solid elevated lesions on his back since last 4 years. His personal and family history were unremarkable. Cutaneous examination demonstrated multiple, discrete, skin-colored to translucent, firm papules showing mid-back distribution. Most papules bore a central umbilication, while some coalesced to form plaques [Figure 1]. Remaining cutaneous, general and systemic examinations were within normal limits. Dermoscopy under polarized light (Dermlite, DL4, 10× magnification) revealed a pattern comprising of a central crater surrounded by white structureless area and/ or shiny white lines and an outer rim of brown structureless area [Figure 2a]. Occassional white rosettes (white dots, arranged in a square) and dotted vessels [Figure 2b] were identified. We considered syringocystadenoma papilliferum and molluscum contagiosum as differentials. Histopathology revealed hyperkeratosis, papillomatosis and dermal cystic invaginations [Figure 3a] lined by double-layered epithelium- an inner row of columnar cells and outer row of small cuboidal cells [Figure 3b]. We observed multiple luminal papillary projections, and the stroma was infiltrated with lymphocytes, histiocytes, plasma cells and sparse neutrophils. Few columnar cells showed decapitation secretion. The upper dermis showed dense cellular infiltration (lymphocytes > plasma cells), + while lower dermis demonstrated dilated apocrine glands. We made a diagnosis of syringocystadenoma pappiliferum and, referred the patient to the department of plastic surgery for complete surgical excision.

- Multiple, discrete, skin-colored to translucent, firm papules on the mid-back with most having central umbilication and at places coalescing to form plaques.
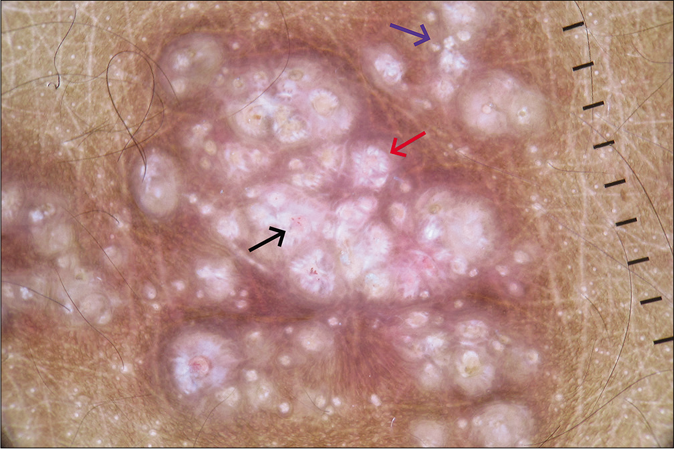
- Dermoscopy (Dermlite, DL4, ×10) under polarized mode showing central crater surrounded by shiny white lines and an outer rim of brown structureless area (red arrow), white rosette (blue arrow) and dotted vessels (black arrow).
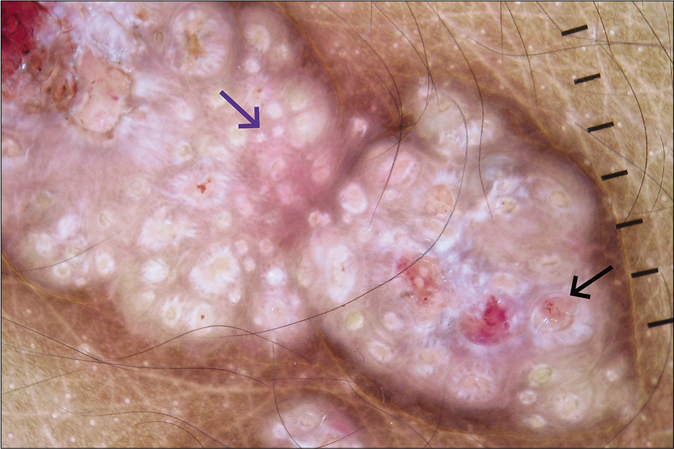
- Dermoscopy (Dermlite, DL4, ×10) under polarized mode showing white rosette (blue arrow) and dotted vessels (black arrow).
- Histopathology showing hyperkeratosis, papillomatosis, dermal cystic invaginations along with dense inflammatory cells in the upper dermis and dilated apocrine ducts in the lower dermis (H and E, ×100).
- Histopathology showing cystic invaginations lined by an inner row of columnar cells and an outer row of small cuboidal cells. A few columnar cells showing decapitation secretion (H and E, ×400).
Syringocystadenoma papilliferum usually affects infants and children, while adolescents and adults constitute 15–30% cases. The head and neck region is affected most commomnly, in about 75% cases. Although benign, a rare transformation to basal cell, metastatic and ductal carcinoma has been reported. Three different clinical morphologies exist plaque, linear and solitary nodular type. The histogenesis of syringocystadenoma papilliferum is controversial and a hamartomatous origin from mature apocrine, eccrine or undifferentiated pluripotent cells is postulated.2
We found only eight previous reports describing the dermoscopic features of syringocystadenoma papilliferum, with only four having de novo origin. On dermoscopy, we observed, a central crater surrounded by white structureless area and/or shiny white lines in most papules, both discrete and coalescing. The central crater corresponds to the characteristic cystic invagination and the white structureless area represents the surrounding hyperplastic epidermis. A similar observation has been reported by Chauhan et al. and Zaballos et al., who described central depression and ulceration in syringocystadenoma papilliferum and correlated it histologically to cystic spaces opening to the skin.1,3 We were unable to find any previous report depicting shiny white structures and lines, including rosettes, features of polarized mode. Haspeslagh et al. described smaller (0.1–0.2 mm) and larger (0.3–0.5 mm) rosettes, and attributed them to cross-polarization of concentric horn material in follicular and eccrine ducts at the infundibular level of biopsy and concentric perifollicular fibrosis, respectively.4 In our case, the rosettes may be attributed to perifollcicular or perieccrine ductal or pericrater (polarizing) keratinisation.1 Zaballos et al. have reported a polymorphic vascular pattern and correlated the vascular structures to the fibrovascular core of papillary projections; which corroborates our finding of dotted vessels inside the craters.3 Unlike in our case, Lombardi and colleagues reported a yellowish hue representing the underlying nevus sebaceus.5
Molluscum contagiosum is the closest differential of our case, dermoscopically characterized by the co-existence of orifices, polylobular yellowish-white material or uniform homogenous color in the center, vascular structures (crown, punctiform, radial and mixed flower) and white rosettes.6 This vascular pattern is restricted to the amorphous structure, and never crosses the core in contast to syringocystadenoma papilliferum, in which vascular structures may involve the central crater, as in our case. Another close differential diagnosis is linear unilateral basaloid follicular hamartoma, dermoscopically distinguished by brown-gray globules and dots, in focus dots, brown linear and arciform structures, crown vessels, short fine telangiectasias, spoke wheel-like structures without a central dark point, white structureless areas with telangiectasias and keratotic plug.7
To conclude, the dermoscopic pattern consisting of a central crater surrounded by a white homogenous area, representing cystic invagination and surrounding epidermal hyperplasia respectively, can be a valuable diagnostic clue for de novo syringocystadenoma papilliferum. Additionally, we have described two novel dermoscopic features- shiny white lines and rosette.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Dermoscopy of a rare case of linear syringocystadenoma papilliferum with review of the literature. Dermatol Pract Concept. 2018;8:33-8.
- [CrossRef] [PubMed] [Google Scholar]
- Syringocystadenoma papilliferum: A case series and review of the literature in Indian context. Hell J Surg. 2014;86:98-101.
- [CrossRef] [Google Scholar]
- Dermoscopy of tumours arising in naevus sebaceous: A morphological study of 58 cases. J Eur Acad Dermatol Venereol. 2015;29:2231-7.
- [CrossRef] [PubMed] [Google Scholar]
- Rosettes and other white shiny structures in polarized dermoscopy: Histological correlate and optical explanation. J Eur Acad Dermatol Venereol. 2016;30:311-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of syringocystadenoma papilliferum. Australas J Dermatol. 2018;59:e59-61.
- [CrossRef] [PubMed] [Google Scholar]
- Rosette: An additional in vivo dermoscopic finding in molluscum contagiosum. Indian J Pediatr Dermatol. 2019;20:349-50.
- [CrossRef] [Google Scholar]
- Clinicopathological and dermoscopic features in a case of linear and unilateral basaloid follicular hamartoma. Indian Dermatol Online J. 2019;10:710-3.
- [CrossRef] [PubMed] [Google Scholar]





