Translate this page into:
Dermoscopic manifestations of Talaromyces (Penicillium) marneffei infection in an AIDS patient
2 Department of Pathology, West China Hospital, Sichuan University, Chengdu, Sichuan Province, People's Republic of China
Correspondence Address:
Yuping Ran
Department of Dermatovenereology, West China Hospital, Sichuan University, Chengdu - 610041, Sichuan Province
People's Republic of China
| How to cite this article: Xu X, Ran X, Pradhan S, Lei S, Ran Y. Dermoscopic manifestations of Talaromyces (Penicillium) marneffei infection in an AIDS patient. Indian J Dermatol Venereol Leprol 2019;85:348 |
Sir,
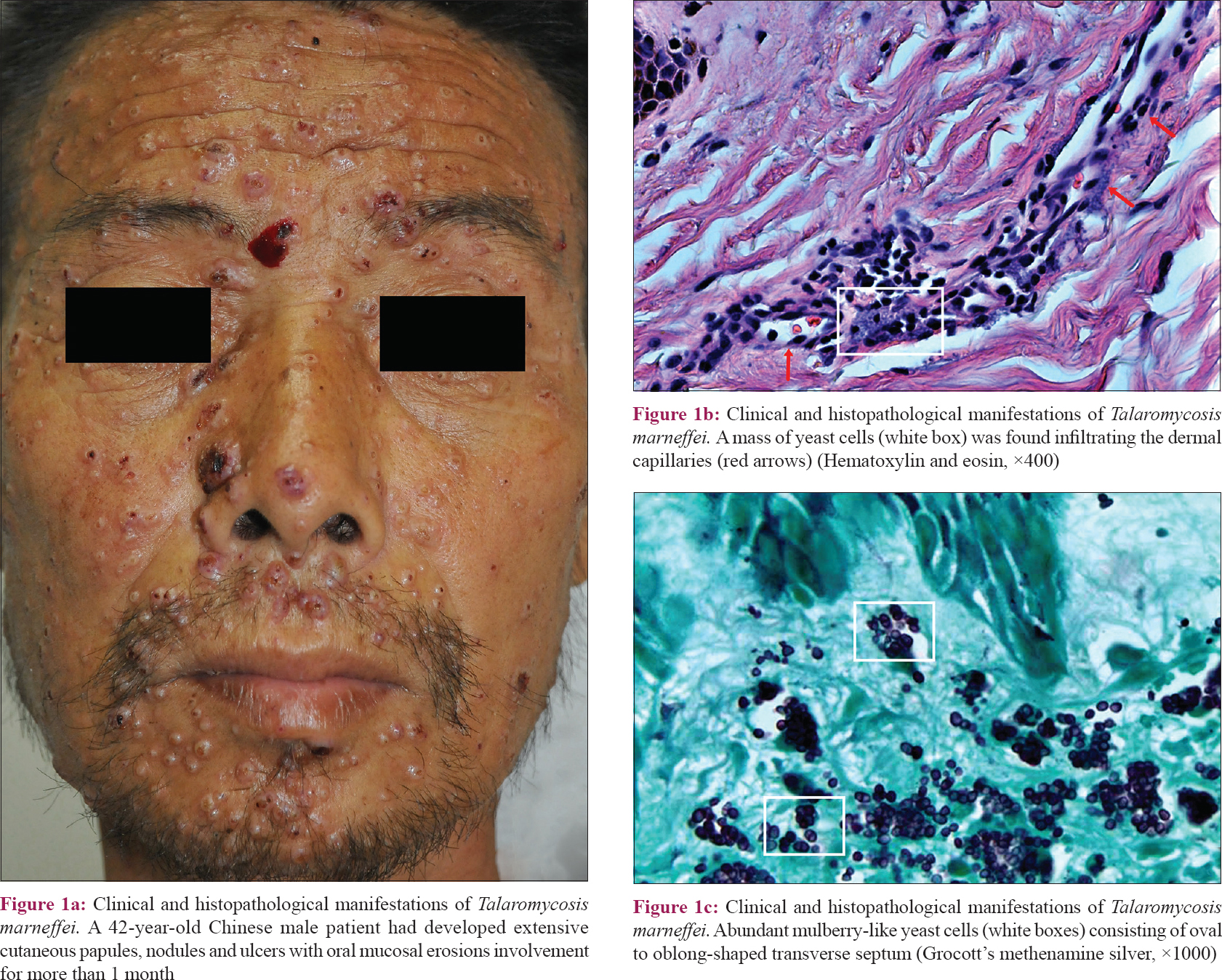
A 42-year-old Chinese male patient, known to be HIV-infected (Human immunodeficiency virus), suffering from Acquired immune deficiency syndrome (AIDS), presented to our clinic (West China Hospital of Sichuan University) on account of extensive cutaneous papules, nodules and ulcers with oral mucosal erosions of more than 1 month duration [Figure - 1]a. On general examination, he looked emaciated and pale. His body temperature was 38.8°C, pulse rate was 100 beats per minute and blood pressure was 110/80 mmHg. His skin appeared moderately icteric with generalized rashes, which were predominantly located on the face, mouth and upper trunk. His cervical lymph nodes were found to be enlarged on palpation and scattered, moist crepitations were heard during chest auscultation. The complete blood cell count revealed a leukocyte count of 3.1 × 10(9) cells/L, hemoglobin level of 67 g/L and blood platelet count of 24 × 10(9)/L. The biochemical parameters were abnormal with total bilirubin level of 241.6 μmol/L, aspartate aminotransferase level of 298 IU/L (normal range: AST <40 IU/L) and alanine aminotransferase -100 IU/L (normal range: ALT <50 IU/L). His serum HIV antigen–antibody complex level, tested by electrochemiluminescence immunoassay was 801.4 COI (normal range: 0–1 COI). The culture of tissue samples exhibited white and cerebriform yeast colonies growing at 37°C and white mycelial-form colonies with a claret-red background, growing at 25°C. The isolate was identical to Talaromyces (Penicillium) marneffei (GenBank Number: KY397946).
 |
| Figure 1: |
Histopathological Manifestations
Hematoxylin–eosin staining showed abundant inflammatory cell infiltrates in the dermis. Colonies of yeast cells were found around the dermal capillaries [Figure - 1]b. Grocott's methenamine silver staining demonstrated mulberry-like yeast cells which showed an oval to oblong-shaped transverse septum [Figure - 1]c.
Dermoscopic Appearance
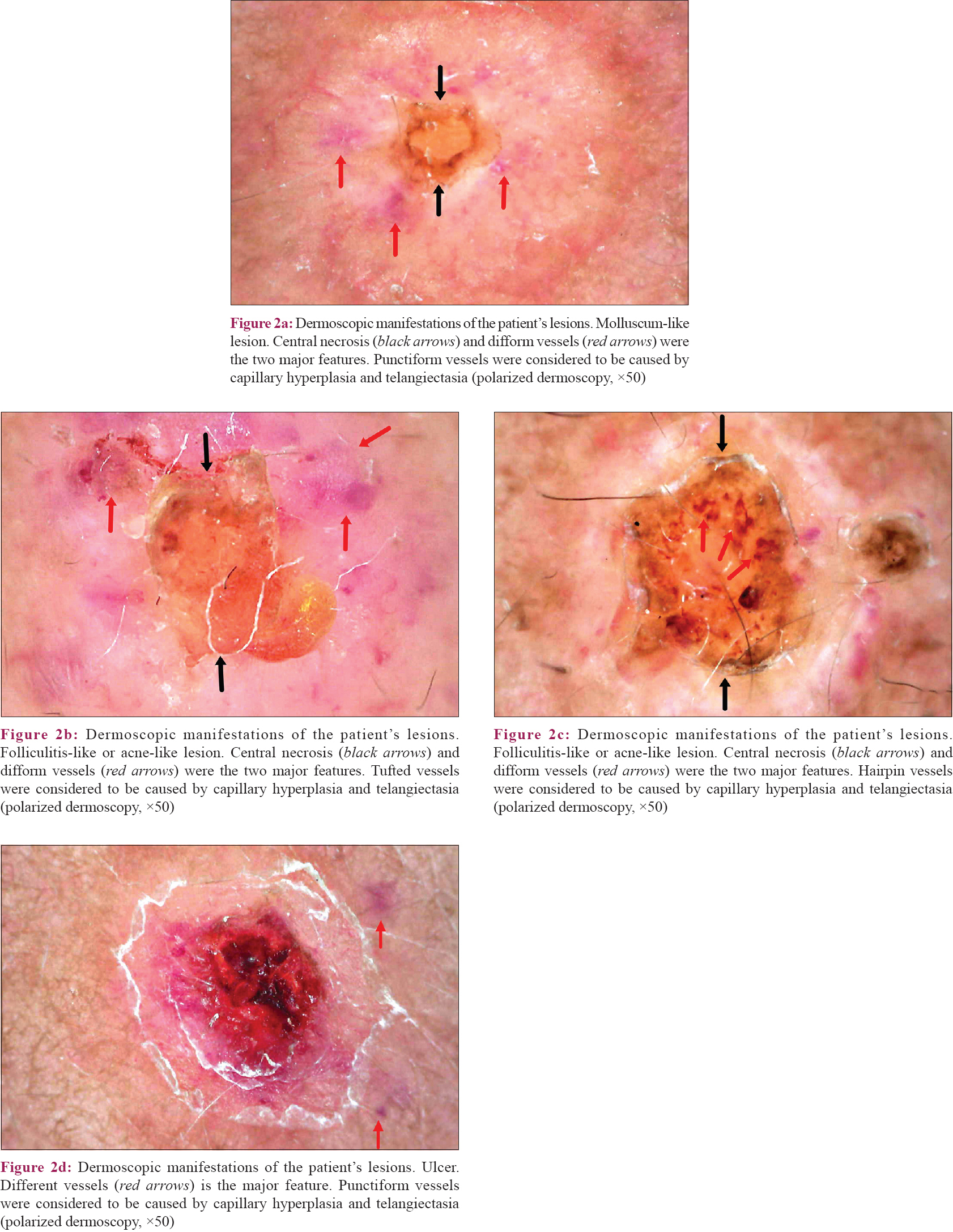
On polarized dermoscopic examination (Dino-Lite AM7013MZT by AnMo Electronics Corporation, Chinese distributor), we observed four types of skin lesions: molluscum-like [Figure - 2]a, folliculitis-like or acne-like [Figure - 2]b and [Figure - 2]c, xanthoma-like rashes and ulcers [Figure - 2]d. They were pervaded by hemispherical papules, nodules and ulcers with a diameter of 5–15 mm. One significant characteristic feature was central necrosis. Papules or nodules with an umbilicated notch centrally were analogous to molluscum contagiosum; papules or nodules with scabs in the middle and hairs grown in or around were similar to folliculitis or acne; yellowish papules or nodules without any scabs, umbilicated notch with hairs had a smooth surface resembling xanthoma. Additionally, different vessels buried inside or around the lesion was another characteristic feature. Punctiform [Figure - 2]a and [Figure - 2]d, tufted [Figure - 2]b, lumbricoid and hairpin [Figure - 2]c vessels appeared irregularly in almost every lesion and were considered to be caused by capillary hyperplasia and telangiectasia.
 |
| Figure 2: |
Cutaneous manifestations are an important aspect of any disease for the clinicians to reach a specific diagnosis. Generally, the skin lesions of Talaromyces (Penicillium) marneffei infection are predominantly located on the face and upper trunk. The main aim of reporting this case is the dermoscopic appearance which may aid in early diagnosis and help in distinguishing it from similar appearing entities such as cutaneous histoplasmosis, blastomycosis and leishmaniasis. Evenly distributed hemispherical papules or nodules with obvious central necrosis and irregular vessels are typical lesions of this disease. Under dermoscopy, histoplasmosis has arborizing telangiectasias on the periphery of the lesion and superficial scaling.[1] Blastomycosis shows overlapping pink-colored papillomatous structures and irregular vessels.[2] Leishmaniasis is characterized by burst star-whitish appearance and hairpin vessels.[3] Talaromyces marneffei w as previously termed as Penicillium marneffei. Infection of this fungus is presumably via inhalation of spores from the environment with access to the host tissue. The pathogenic mechanism is still under research.[4] The patient in our case died owing to systemic disseminated infection despite prompt administration of itraconazole. A mass of yeast cells was found infiltrating the dermal capillaries and correspondingly, the phenomena of capillary hyperplasia and telangiectasia of skin lesions through dermoscopy were observed. The multiple dermoscopic manifestations could be linked to the anatomic characteristics (such as local hair follicle distribution or microvessel density) and the stages of the infectious involvement; which in this case, could be considered as indicators of the hematogenous spread of the fungus. Therefore, if a patient exhibits central necrotic papules or nodules with irregular vessels, along with biopsy revealing dermal capillaries infiltrated by yeast cells at the same time, a chest X-ray, abdominal and urinary system ultrasound and other related laboratory examinations should be considered for further evaluation to determine the severity of visceral metastasis.
Declaration of the patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for the images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Zattar GA, Cardoso F, Nakandakari S, Soares CT. Cutaneous histoplasmosis as a complication after anti-TNF use – Case report. An Bras Dermatol 2015;90:104-7.
[Google Scholar]
|
| 2. |
Wang S, Martini MC, Groth JV, Hernandez C. Dermatoscopic and clinicopathologic findings of cutaneous blastomycosis. J Am Acad Dermatol 2015;73:e169-70.
[Google Scholar]
|
| 3. |
Ramot Y, Nanova K, Alper-Pinus R, Zlotogorski A. Zosteriform cutaneous leishmaniasis diagnosed with the help of dermoscopy. Dermatol Pract Concept 2014;4:55-7.
[Google Scholar]
|
| 4. |
Vanittanakom N, Cooper CR Jr., Fisher MC, Sirisanthana T. Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspects. Clin Microbiol Rev 2006;19:95-110.
[Google Scholar]
|
Fulltext Views
3,129
PDF downloads
2,195





