Translate this page into:
Dermoscopic pitfall: Microcystic adnexal carcinoma mimicking basal cell carcinoma
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Vishal Gupta
Department of Dermatology and Venereology, Fourth Floor, Teaching Block, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029
India
| How to cite this article: Gupta V, Kakkar A, Agarwal S, Sulaiman M, Ramam M. Dermoscopic pitfall: Microcystic adnexal carcinoma mimicking basal cell carcinoma. Indian J Dermatol Venereol Leprol 2020;86:202-205 |
Sir,
Microcystic adnexal carcinoma is often mistaken for benign adnexal tumors or basal cell carcinoma clinically and histologically.[1] Though dermoscopy is helpful in the differential diagnosis of cutaneous tumors, information on the dermoscopic features of microcystic adnexal carcinoma is limited.
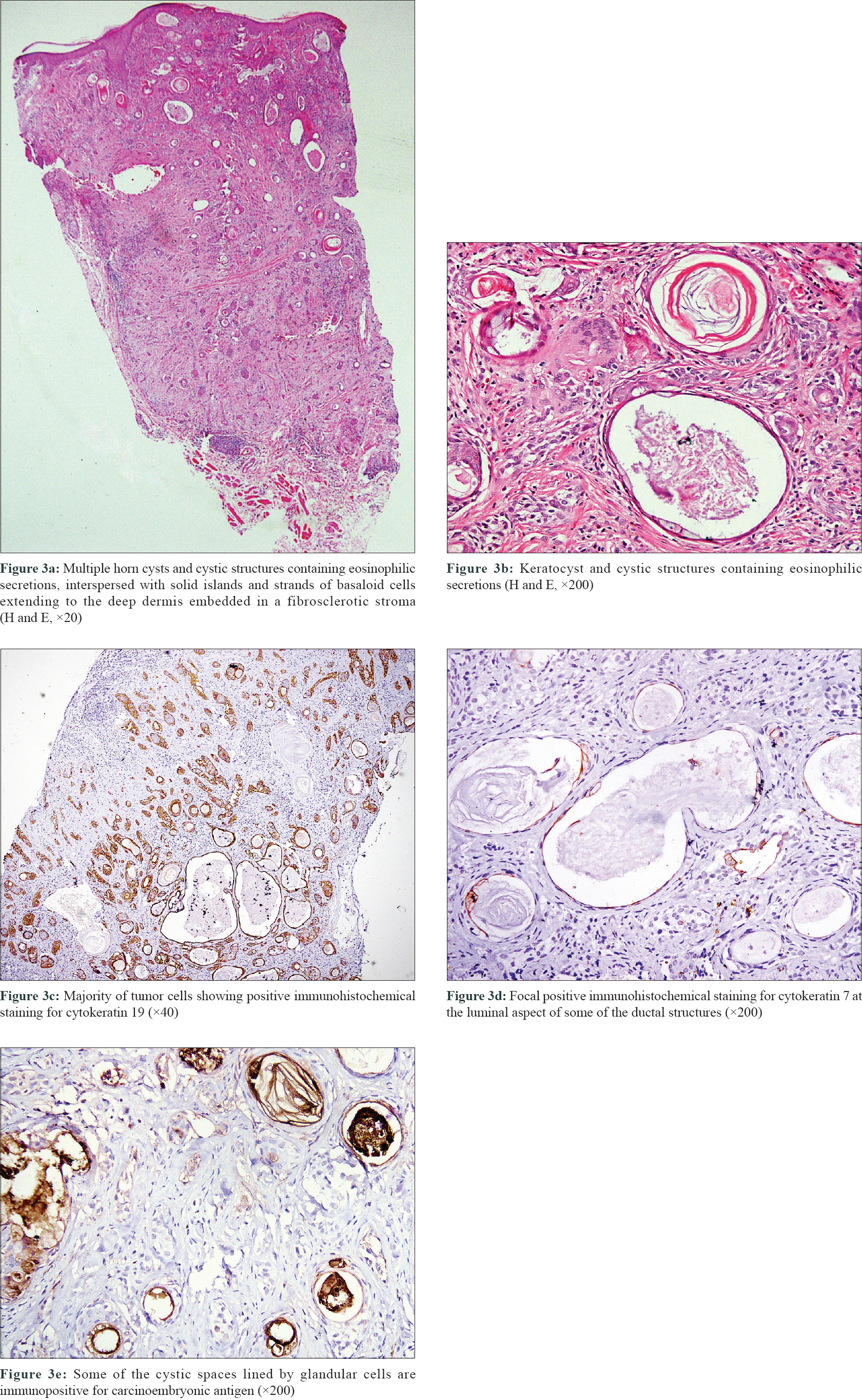
A 53-year-old Indian male, with Fitzpatrick skin phototype V, presented with a slowly enlarging asymptomatic plaque on the right side of his upper lip of 12 years duration. A rapid increase in size in the past 6 months prompted the consultation. At presentation, there was a single indurated plaque of about 3 × 2 cm in size on the right side of upper lip encroaching the vermilion border. There was a central crateriform depression with focal scale-crusts and hemorrhage. The margins were elevated and had a pearly rolled appearance with telangiectasias [Figure - 1]. Oral cavity examination was unremarkable. There was no regional lymphadenopathy. Dermoscopic examination showed a central pinkish-white structureless area with overlying scale-crusts and hemorrhage. There were sharply in-focus arborizing vessels in the periphery and a few yellow-white clods on the inferior margin. Gray-brown dots were also present focally [Figure - 2]. Based on these features, a provisional diagnosis of basal cell carcinoma was considered. Histological examination revealed multiple horn cysts and cystic structures containing eosinophilic secretions lined by basaloid and squamoid cells in the dermis extending down to the subcutis. Cysts were larger and more numerous in the upper dermis and became progressively smaller in the mid and deep dermis. There were solid islands and strands of basaloid cells interspersed with cysts in the mid and deep dermis, embedded in a fibrosclerotic stroma. Immunohistochemical staining with cytokeratin 19 was positive in a majority of tumor cells, cytokeratin 7 showed focal positivity at the luminal aspect of some of the ductal structures, while CD23 was negative. Some of the cystic spaces lined by glandular cells were immunopositive for carcinoembryonic antigen [Figure - 3]. These features were diagnostic of microcystic adnexal carcinoma.
 |
| Figure 1: Indurated plaque with a central crateriform depression and elevated pearly rolled out margins on the right side of upper lip |
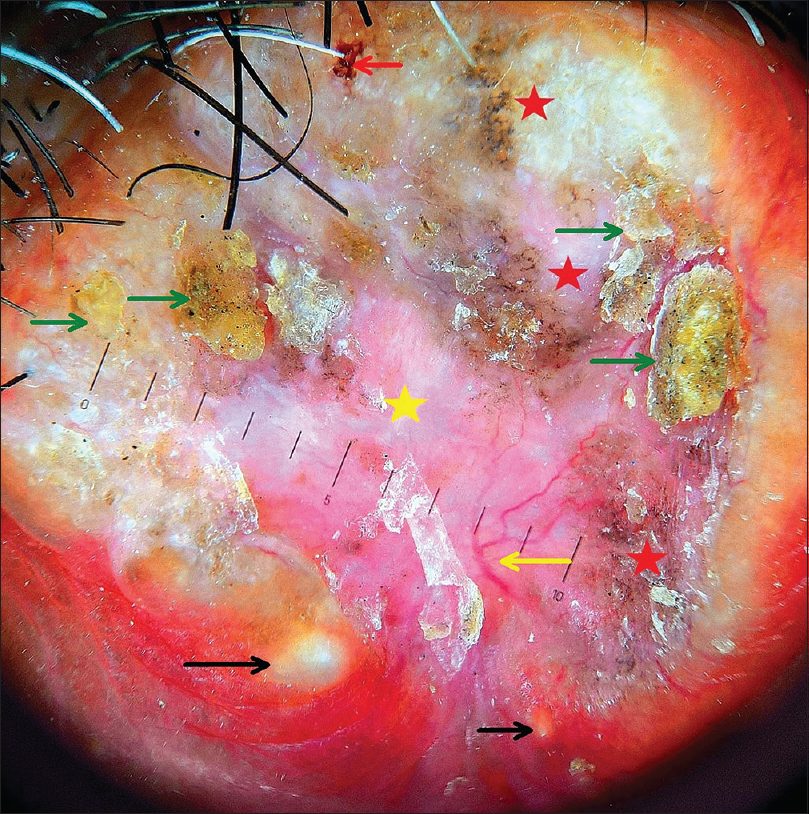 |
| Figure 2: Dermoscopic examination (polarized, 16×; Heine Delta 20T, Heine Optotechnik, Herrsching, Germany) showing pinkish-white background (yellow star) with focal scale-crust (green arrows), hemorrhage (red arrow), gray-brown dots (red star) and in-focus arborizing vessels (yellow arrow). Yellowish-white clods (black arrows) present at the inferior margin |
 |
| Figure 3: |
Microcystic adnexal carcinoma is a rare, locally aggressive, deeply infiltrative malignant adnexal carcinoma with follicular and eccrine differentiation, which typically affects Caucasians.[2] It presents as a slow-growing asymptomatic firm plaque or nodule on the head and neck region, masquerading as benign adnexal tumors or basal cell carcinoma. On histology, it has a superficial component of keratinous cysts and a deeper component of nests and cords of cells embedded in a sclerotic stroma. It is often mistaken for morpheaform basal cell carcinoma, desmoplastic trichoepithelioma or trichoadenoma and syringoma, especially if the biopsy specimen is superficial.[1],[3] Our case showed features of both follicular (keratocysts) and eccrine differentiation (as detected by carcinoembryonic antigen), excluding these histological differential diagnoses. Such a dual differentiation and an infiltrative pattern can also be seen in squamous cell carcinoma (with microcystic adnexal-carcinoma-like differentiation) and squamoid eccrine ductal carcinoma. However, the tumor cells in these neoplasms have an epidermal attachment with a background of in situ squamous cell carcinoma, show prominent cellular atypia, nuclear pleomorphism and mitotic activity.[4] These features were lacking in our case.
Not much literature is available on the dermoscopic findings of microcystic adnexal carcinoma and we could find only four reports on this.[5],[6],[7],[8] The most characteristic finding appears to be the presence of whitish clods of variable size, probably representing keratinous cysts, reported in three out of four cases. The background color varied from white, yellow-orange or brown along with fine linear branched vessels. Interestingly, the whitish clods were not very conspicuous in our case and were appreciated only on a retrospective review of the dermoscopic images. The scale-crusts, hemorrhage and gray-brown dots as seen in our case have not been previously documented in microcystic adnexal carcinoma. In addition, in-focus arborizing vessels were prominently seen in our case, which are considered to be a hallmark of basal cell carcinoma, although its diagnostic significance is now being reconsidered.[9],[10] Recently, focussed arborizing vessels have been reported in dermoscopy of a few skin disorders other than basal cell carcinoma such as epidermoid cysts, scars, intradermal nevi and actinic keratosis. The authors found the ratio of widest diameter of stem vessel to widest diameter of first branch to be statistically significantly more in the non-basal cell carcinoma group when compared with basal cell carcinomas.[11]
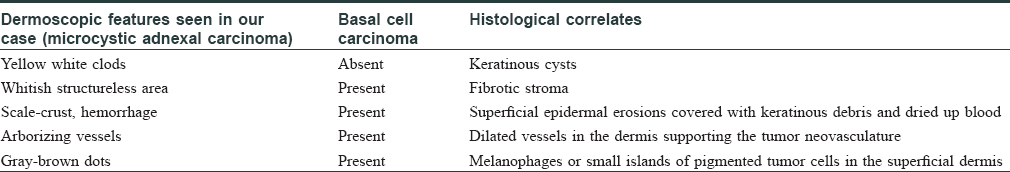
The overall dermoscopic features in our case resembled those of basal cell carcinoma. This is not surprising because microcystic adnexal carcinoma and basal cell carcinoma share several histological features [Table - 1]. Furthermore, benign adnexal tumors, especially the follicular tumors, have also been reported to resemble basal cell carcinoma on dermoscopy, showing arborizing vessels and blue-gray dots or globules. Like microcystic adnexal carcinoma, “whitish clods” representing follicular structures might aid in their correct recognition as well.[12] To conclude, microcystic adnexal carcinoma should be added to the list of dermoscopic mimics of basal cell carcinoma. More data is needed before dermoscopy can be used as a reliable tool to distinguish microcystic adnexal carcinoma from its clinical mimics.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
McKinley LH, Seastrom S, Hanly AJ, Miller RA. Microcystic adnexal carcinoma: Review of a potential diagnostic pitfall and management. Cutis 2014;93:162-5.
[Google Scholar]
|
| 2. |
Gordon S, Fischer C, Martin A, Rosman IS, Council ML. Microcystic adnexal carcinoma: A review of the literature. Dermatol Surg 2017;43:1012-6.
[Google Scholar]
|
| 3. |
Stanoszek LM, Wang GY, Harms PW. Histologic mimics of basal cell carcinoma. Arch Pathol Lab Med 2017;141:1490-502.
[Google Scholar]
|
| 4. |
Ibrahim YL, Lambert S, Kazakov DV, Kaya G. An unusual morphological presentation of cutaneous squamous cell carcinoma mimicking microcystic adnexal carcinoma: A diagnostic pitfall. Dermatopathology (Basel) 2018;5:64-8.
[Google Scholar]
|
| 5. |
Inskip M, Magee J. Microcystic adnexal carcinoma of the cheek – A case report with dermatoscopy and dermatopathology. Dermatol Pract Concept 2015;5:43-6.
[Google Scholar]
|
| 6. |
Yoshida M, Kato H, Watanabe S, Morita A. A case of microcystic adnexal carcinoma complicated with sigmoid colon carcinoma. Rinsho Derma 2011;53:389-92.
[Google Scholar]
|
| 7. |
Shinohara R, Ansai S, Ogita A, Matsuda H, Saeki H, Tanaka M, et al. Dermoscopic findings of microcystic adnexal carcinoma. Eur J Dermatol 2015;25:516-8.
[Google Scholar]
|
| 8. |
Calderón-Castrat X, Román-Curto C, Santos-Briz A, Fernández-López E. Microcystic adnexal carcinoma mimicking basal cell carcinoma. JAAD Case Rep 2017;3:492-4.
[Google Scholar]
|
| 9. |
Lallas A, Apalla Z, Argenziano G, Longo C, Moscarella E, Specchio F, et al. The dermatoscopic universe of basal cell carcinoma. Dermatol Pract Concept 2014;4:11-24.
[Google Scholar]
|
| 10. |
Altamura D, Menzies SW, Argenziano G, Zalaudek I, Soyer HP, Sera F, et al. Dermatoscopy of basal cell carcinoma: Morphologic variability of global and local features and accuracy of diagnosis. J Am Acad Dermatol 2010;62:67-75.
[Google Scholar]
|
| 11. |
Jin H, Yang MY, Kim JM, Kim GW, Kim HS, Ko HC, et al. Arborizing vessels on dermoscopy in various skin diseases other than basal cell carcinoma. Ann Dermatol 2017;29:288-94.
[Google Scholar]
|
| 12. |
Lallas A, Moscarella E, Argenziano G, Longo C, Apalla Z, Ferrara G, et al. Dermoscopy of uncommon skin tumours. Australas J Dermatol 2014;55:53-62.
[Google Scholar]
|
Fulltext Views
4,837
PDF downloads
51,279





